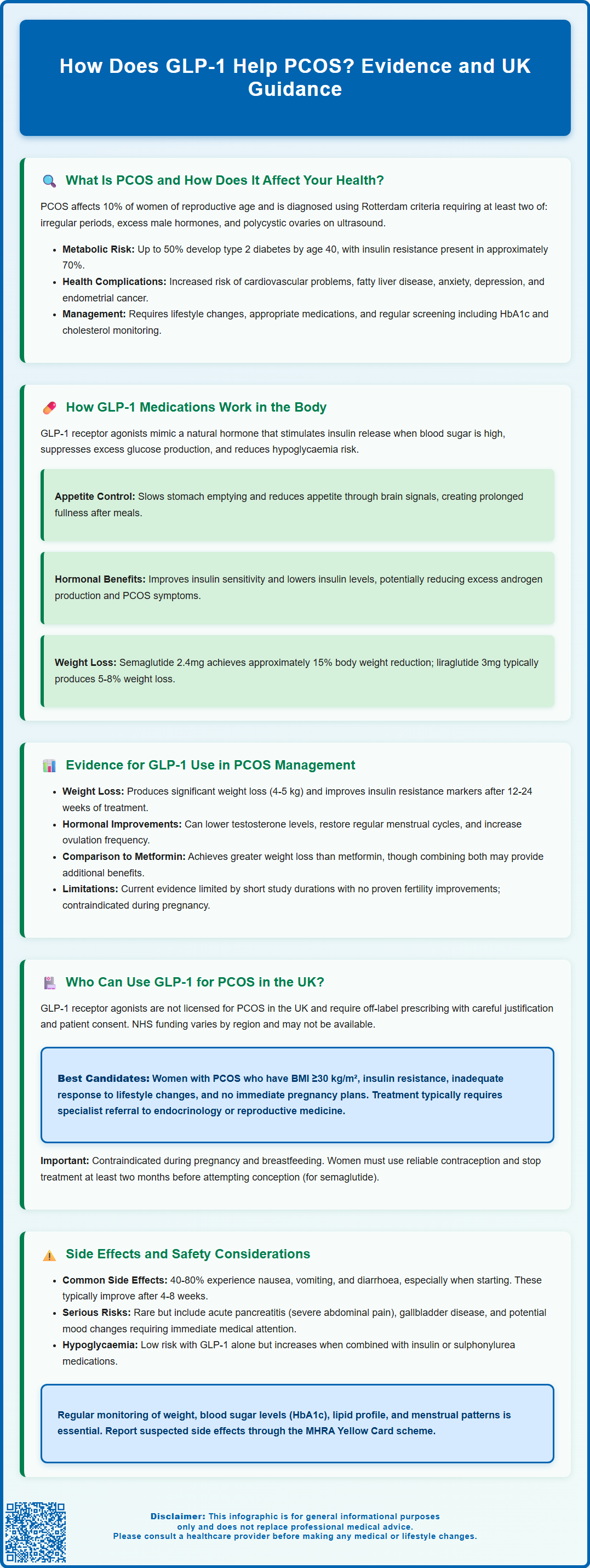
Polycystic ovary syndrome (PCOS) affects approximately 10% of women of reproductive age in the UK, causing hormonal imbalances, irregular periods, and significant metabolic complications including insulin resistance and increased diabetes risk. Glucagon-like peptide-1 (GLP-1) receptor agonists—medications originally developed for type 2 diabetes—are emerging as a potential treatment option for PCOS due to their effects on insulin sensitivity, weight management, and hormonal regulation. Whilst not currently licensed for PCOS in the UK, growing evidence suggests GLP-1 therapy may address both metabolic and reproductive features of this complex condition. This article examines how GLP-1 medications work, the clinical evidence supporting their use, eligibility criteria, and important safety considerations for women with PCOS.
Summary: GLP-1 receptor agonists help PCOS by improving insulin sensitivity, reducing compensatory hyperinsulinaemia, promoting weight loss, and thereby lowering androgen levels and potentially restoring menstrual regularity.
- GLP-1 medications stimulate glucose-dependent insulin secretion, suppress glucagon, slow gastric emptying, and reduce appetite through central mechanisms.
- Clinical trials show GLP-1 therapy reduces body weight, improves insulin resistance markers, lowers testosterone levels, and increases menstrual regularity in women with PCOS.
- GLP-1 receptor agonists are not licensed for PCOS in the UK; their use represents off-label prescribing requiring specialist assessment and informed patient consent.
- Common side effects include nausea, vomiting, and gastrointestinal discomfort, particularly during dose escalation; rare serious risks include pancreatitis and gallbladder disease.
- GLP-1 medications are contraindicated in pregnancy and breastfeeding; women must use reliable contraception and discontinue treatment at least two months before planned conception.
- Access typically requires specialist referral to endocrinology or reproductive medicine services, with NHS funding varying by integrated care board.
Table of Contents
What Is PCOS and How Does It Affect Your Health?
Polycystic ovary syndrome (PCOS) is a common endocrine disorder affecting approximately 10% of women of reproductive age in the UK. It is characterised by a combination of symptoms including irregular menstrual cycles, elevated androgen levels (male hormones), and polycystic ovaries visible on ultrasound. The condition arises from complex interactions between genetic, metabolic, and environmental factors.
Key features of PCOS include:
-
Menstrual irregularities or absent periods (oligomenorrhoea or amenorrhoea)
-
Clinical or biochemical signs of hyperandrogenism (excess facial or body hair, acne, male-pattern baldness)
-
Polycystic ovarian morphology on ultrasound examination
-
Insulin resistance and compensatory hyperinsulinaemia
Diagnosis typically follows the Rotterdam criteria, requiring at least two of the first three features above, after exclusion of other endocrine disorders.
The health implications of PCOS extend well beyond reproductive concerns. Women with PCOS face significantly increased risks of developing type 2 diabetes mellitus, with studies suggesting up to 50% may develop impaired glucose tolerance or diabetes by age 40. Insulin resistance, present in approximately 70% of women with PCOS regardless of body weight, plays a central role in the pathophysiology of the condition.
Additionally, PCOS is associated with increased cardiovascular risk factors including dyslipidaemia, hypertension, and endothelial dysfunction. Weight management presents a particular challenge, as many women with PCOS experience difficulty losing weight due to metabolic abnormalities. The condition also carries psychological burden, with higher rates of anxiety, depression, and reduced quality of life. Non-alcoholic fatty liver disease (NAFLD) occurs more frequently in this population.
Women with PCOS also have an increased risk of endometrial hyperplasia and cancer due to unopposed oestrogen exposure. Guidelines recommend ensuring at least four menstrual bleeds per year, using hormonal contraception or cyclic progestogens if needed.
NICE Clinical Knowledge Summary (CKS) and NHS guidance emphasise the importance of addressing both reproductive and metabolic aspects of PCOS through lifestyle modification, pharmacological intervention when appropriate, and regular screening for associated comorbidities, including periodic HbA1c or glucose tolerance testing and lipid monitoring.
How GLP-1 Medications Work in the Body
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications that mimic the action of naturally occurring GLP-1, an incretin hormone produced by intestinal L-cells in response to food intake. These medications were initially developed for type 2 diabetes management but have gained attention for their broader metabolic effects relevant to PCOS.
Mechanism of action:
GLP-1 receptor agonists bind to GLP-1 receptors located throughout the body, particularly in pancreatic beta cells, the gastrointestinal tract, and the central nervous system. In the pancreas, they stimulate glucose-dependent insulin secretion, meaning insulin is released only when blood glucose levels are elevated, thereby reducing hypoglycaemia risk. Simultaneously, they suppress glucagon secretion from pancreatic alpha cells, which helps prevent excessive hepatic glucose production.
These medications significantly slow gastric emptying, prolonging the sensation of fullness after meals and reducing appetite through central mechanisms in the hypothalamus. This dual action on satiety and gastric motility contributes substantially to their weight loss effects. The gastric emptying effect may diminish somewhat over time with continued treatment (tachyphylaxis). GLP-1 receptor agonists appear to improve insulin sensitivity in peripheral tissues, primarily through weight loss and reduced hyperinsulinaemia.
Relevance to PCOS pathophysiology:
The mechanisms of GLP-1 receptor agonists align well with the metabolic disturbances characteristic of PCOS. By improving insulin sensitivity and reducing compensatory hyperinsulinaemia, these medications may help address the hormonal imbalances that drive androgen excess. Lower insulin levels can reduce ovarian and adrenal androgen production, potentially improving hirsutism, acne, and ovulatory function.
The significant weight loss achieved with GLP-1 therapy varies by agent and dose—with semaglutide 2.4mg (Wegovy) achieving approximately 15% body weight reduction at 68 weeks, while liraglutide 3mg (Saxenda) typically produces 5-8% weight loss. This weight reduction can further improve insulin sensitivity and restore menstrual regularity in many women with PCOS.
Evidence for GLP-1 Use in PCOS Management
The evidence base for GLP-1 receptor agonists in PCOS management is evolving, with several clinical trials demonstrating promising metabolic and reproductive benefits, though it remains an off-label indication in the UK.
Metabolic outcomes:
Multiple randomised controlled trials have examined GLP-1 receptor agonists, particularly liraglutide, in women with PCOS. A systematic review and meta-analysis published in 2020 found that liraglutide treatment resulted in significant reductions in body weight (mean difference approximately 4-5 kg compared to placebo or metformin), improved insulin sensitivity markers, and favourable changes in lipid profiles. Studies typically show improvements in fasting glucose, HbA1c, and HOMA-IR (a measure of insulin resistance) after 12-24 weeks of treatment.
Reproductive and hormonal effects:
Research indicates that GLP-1 therapy can reduce total and free testosterone levels, likely secondary to improved insulin sensitivity and weight loss. Several studies have reported improvements in menstrual regularity, with increased frequency of ovulation in women with oligomenorrhoea. One randomised trial found that 26 weeks of liraglutide treatment restored regular menstrual cycles in a significantly higher proportion of women compared to placebo.
Comparative effectiveness:
When compared to metformin—a commonly used insulin-sensitising medication for metabolic features of PCOS—GLP-1 receptor agonists appear to produce greater weight loss. Metformin is often considered for women with PCOS who have metabolic features or impaired glucose regulation, particularly as it has a well-established safety profile, oral administration, and cost-effectiveness. Some studies suggest combining GLP-1 therapy with metformin may provide additive benefits.
Limitations of current evidence:
It is important to note that most studies have been relatively short-term (12-26 weeks), with limited data on long-term reproductive outcomes, fertility, or pregnancy rates. There is no official link established between GLP-1 use and improved fertility outcomes in large-scale trials, and these medications are contraindicated in pregnancy. Further research is needed to establish optimal dosing, treatment duration, and patient selection criteria specifically for PCOS management.
Any use of GLP-1 receptor agonists for PCOS should involve shared decision-making between patient and clinician, with clear discussion of the off-label nature of treatment and monitoring requirements.
Who Can Use GLP-1 for PCOS in the UK?
In the UK, GLP-1 receptor agonists are not currently licensed specifically for PCOS treatment. Their use in this context represents off-label prescribing, which requires careful clinical justification and informed patient consent. The MHRA has approved various GLP-1 medications for type 2 diabetes and, more recently, for weight management in specific circumstances.
Current licensing and NICE guidance:
Semaglutide (Wegovy) is licensed for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with at least one weight-related comorbidity. NICE Technology Appraisal 875 recommends semaglutide as an option for weight management within its licensed indication, subject to specific criteria including specialist weight management service involvement.
Liraglutide (Saxenda) has similar indications, with NICE Technology Appraisal 664 recommending its use under specific circumstances. However, NICE guidance on obesity management (CG189) and the NICE Clinical Knowledge Summary (CKS) for PCOS do not currently include GLP-1 receptor agonists as recommended treatment options specifically for PCOS.
Potential candidates for off-label use:
Clinicians may consider GLP-1 therapy for women with PCOS who meet the following criteria:
-
Overweight or obesity (particularly BMI ≥30 kg/m²) with PCOS
-
Insulin resistance or impaired glucose tolerance
-
Inadequate response to lifestyle modification and other treatments
-
No contraindications to GLP-1 therapy
-
Not planning pregnancy in the immediate future
Contraindications and precautions:
GLP-1 receptor agonists are contraindicated in pregnancy and breastfeeding. Women of childbearing potential must use reliable contraception during treatment. For semaglutide, treatment should be discontinued at least two months before planned conception attempts; other GLP-1 medications may have different recommendations (check the specific product SmPC).
Precautions and warnings (not formal contraindications) include personal or family history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, severe gastrointestinal disease, and previous pancreatitis.
Access and prescribing considerations:
Access to GLP-1 medications for PCOS typically requires specialist referral to endocrinology or reproductive medicine services. NHS funding for off-label use varies by integrated care board and may not be available; private prescription may be necessary. Patients should discuss the evidence, potential benefits, costs, and limitations with their healthcare provider before commencing treatment. Regular monitoring of weight, metabolic parameters, and menstrual patterns is essential during therapy.
Side Effects and Safety Considerations
GLP-1 receptor agonists are generally well-tolerated, but patients should be aware of potential adverse effects and safety considerations before starting treatment for PCOS.
Common gastrointestinal side effects:
The most frequently reported adverse effects are gastrointestinal in nature, occurring in up to 40-80% of patients with higher doses, particularly during dose escalation:
-
Nausea (most common, typically improves after 4-8 weeks)
-
Vomiting
-
Diarrhoea or constipation
-
Abdominal discomfort or bloating
-
Reduced appetite
These effects can be minimised by starting with low doses and gradually titrating upwards according to manufacturer guidance. Eating smaller, lower-fat meals and staying well-hydrated may help reduce nausea. Severe or prolonged gastrointestinal symptoms can lead to dehydration and acute kidney injury in some cases, so maintaining adequate fluid intake is important.
Serious but rare adverse effects:
Whilst uncommon, several serious adverse effects require awareness. Acute pancreatitis has been reported rarely with GLP-1 therapy; patients should seek immediate medical attention if they experience severe, persistent abdominal pain radiating to the back. There is a theoretical risk of thyroid C-cell tumours based on animal studies, though no definitive link has been established in humans. Gallbladder disease, including cholelithiasis and cholecystitis, occurs more frequently with rapid weight loss.
Hypoglycaemia risk is low when GLP-1 agonists are used alone but increases when combined with insulin or sulphonylureas. Injection site reactions (redness, itching, bruising) affect approximately 10% of patients but are usually mild.
Monitoring and patient safety advice:
Patients should be monitored regularly during treatment, with assessment of:
-
Weight and BMI
-
Metabolic parameters (fasting glucose, HbA1c, lipid profile)
-
Menstrual cycle patterns
-
Symptoms of adverse effects
When to contact your GP:
Patients should seek medical advice if they experience severe or persistent abdominal pain, signs of pancreatitis, symptoms of gallbladder disease, unexplained neck lumps, significant mood changes, or if they suspect pregnancy. Women planning conception should discontinue GLP-1 therapy according to product-specific guidance and inform their healthcare provider.
Suspected adverse reactions should be reported through the MHRA Yellow Card scheme. Regular follow-up ensures treatment remains appropriate, effective, and safe for individual circumstances.
Frequently Asked Questions
Are GLP-1 medications approved for PCOS treatment in the UK?
No, GLP-1 receptor agonists are not currently licensed specifically for PCOS in the UK. Their use for PCOS represents off-label prescribing, which requires specialist assessment, clinical justification, and informed patient consent.
How long does it take for GLP-1 therapy to improve PCOS symptoms?
Most clinical studies show improvements in metabolic markers and insulin sensitivity within 12–24 weeks of GLP-1 treatment. Menstrual regularity and hormonal improvements may occur within 26 weeks, though individual responses vary and long-term data remain limited.
Can I take GLP-1 medication if I'm trying to conceive?
No, GLP-1 receptor agonists are contraindicated in pregnancy and must be discontinued before conception attempts—at least two months before for semaglutide. Women of childbearing potential must use reliable contraception during treatment and inform their healthcare provider when planning pregnancy.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript