Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist widely prescribed in the UK for type 2 diabetes mellitus. Whilst it delivers excellent glycaemic control and cardiovascular benefits, gastrointestinal issues with Ozempic are amongst the most frequently reported side effects. Nausea, vomiting, diarrhoea and constipation commonly occur, particularly during treatment initiation and dose escalation. Understanding why these symptoms arise, how to manage them effectively, and when to seek medical advice is essential for patients and healthcare professionals. This article explores the mechanisms behind GI side effects, practical management strategies, and alternative treatment options for those unable to tolerate Ozempic.
Summary: Gastrointestinal issues with Ozempic occur because semaglutide delays gastric emptying and stimulates GLP-1 receptors in the brainstem, commonly causing nausea, vomiting, diarrhoea and constipation, particularly during treatment initiation.
- Ozempic is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus treatment.
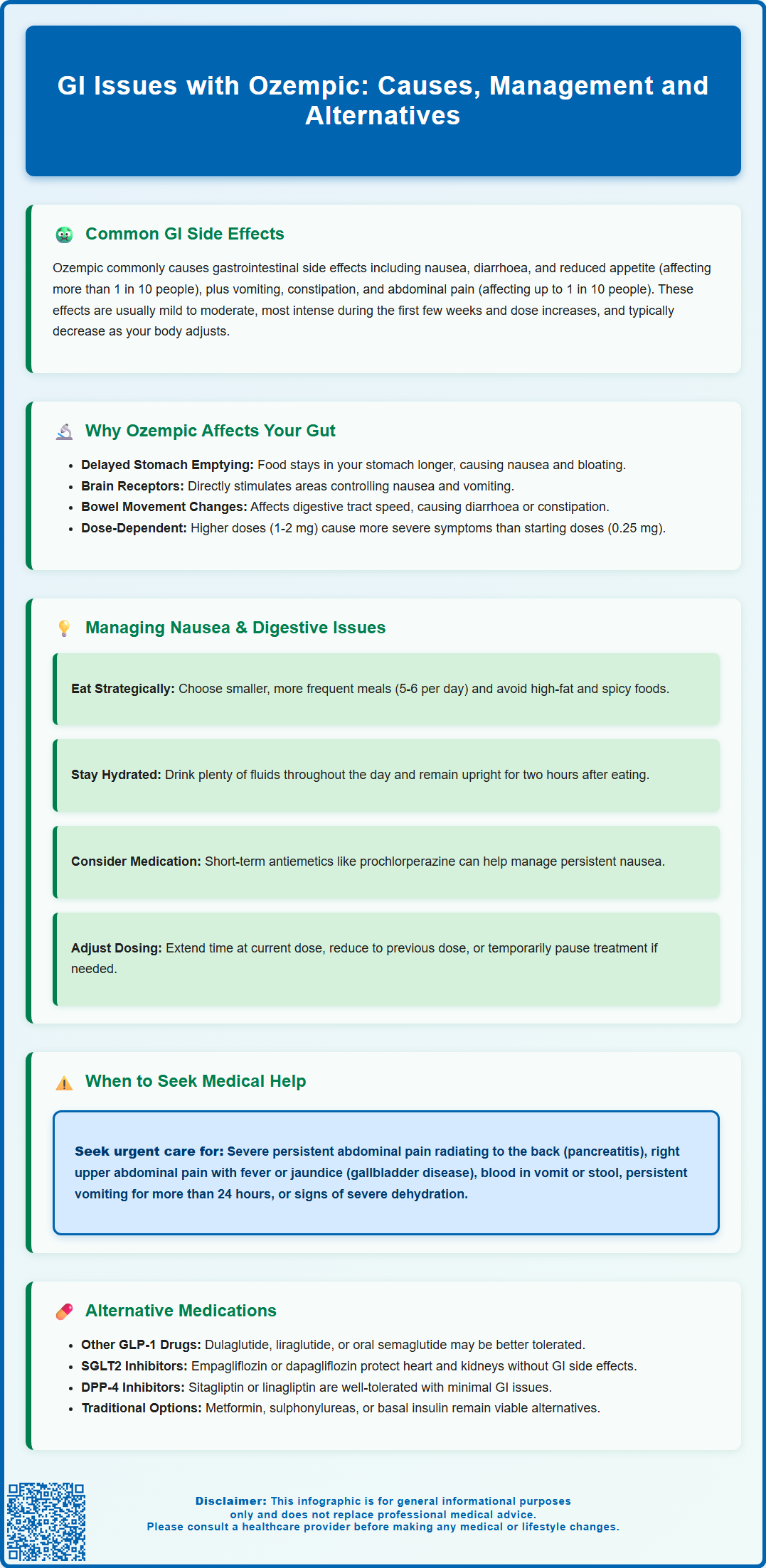
- Very common GI side effects include nausea, diarrhoea and reduced appetite (affecting more than 1 in 10 people).
- Symptoms arise from delayed gastric emptying and direct stimulation of nausea centres in the brainstem.
- Management includes smaller frequent meals, avoiding high-fat foods, adequate hydration, and short-term antiemetics if needed.
- Rare serious complications include acute pancreatitis and gallbladder disease requiring urgent medical assessment.
- Alternative treatments include other GLP-1 agonists, SGLT2 inhibitors, DPP-4 inhibitors, or insulin therapy as per NICE guidance.
Table of Contents
What Are the Common GI Issues with Ozempic?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Whilst it offers significant glycaemic control and cardiovascular benefits, gastrointestinal (GI) side effects are amongst the most frequently reported adverse reactions, particularly during treatment initiation and dose escalation.
The most common GI issues include:
-
Nausea – very common (may affect more than 1 in 10 people), typically most pronounced in the first few weeks of therapy
-
Vomiting – common (may affect up to 1 in 10 people), often more frequent with higher doses
-
Diarrhoea – very common (may affect more than 1 in 10 people), which may be transient or persistent
-
Constipation – common (may affect up to 1 in 10 people), sometimes alternating with diarrhoea
-
Abdominal pain or discomfort – common (may affect up to 1 in 10 people)
-
Dyspepsia and bloating – common but generally less troublesome complaints
-
Reduced appetite – very common (may affect more than 1 in 10 people), which can contribute to GI symptoms
These symptoms are generally mild to moderate in severity and tend to diminish over time as the body adapts to the medication. However, some patients find GI side effects intolerable, leading to dose reduction or discontinuation. The incidence and severity of these effects are dose-dependent, with higher maintenance doses (1 mg or 2 mg weekly) associated with greater GI intolerance than lower starting doses (0.25 mg weekly).
It's important to be aware of rare but serious GI complications including acute pancreatitis (persistent severe abdominal pain, sometimes radiating to the back, with or without vomiting) and gallbladder disease (right upper quadrant pain, fever or jaundice). These require urgent medical assessment. Additionally, vomiting and diarrhoea can cause dehydration, which may worsen renal function, particularly in patients with pre-existing kidney disease.
Patients should be counselled about these potential side effects prior to commencing treatment and advised on strategies to minimise discomfort during the titration phase.
Why Does Ozempic Cause Gastrointestinal Side Effects?
Understanding the pharmacological mechanism of semaglutide helps explain why GI side effects are so prevalent. As a GLP-1 receptor agonist, Ozempic mimics the action of endogenous GLP-1, a naturally occurring incretin hormone released by intestinal L-cells in response to food intake. This hormone plays a crucial role in glucose homeostasis, but it also exerts significant effects on the gastrointestinal tract.
Key mechanisms underlying GI side effects include:
-
Delayed gastric emptying – GLP-1 receptor activation slows the rate at which the stomach empties its contents into the small intestine. This prolonged gastric retention contributes to early satiety, nausea, and feelings of fullness or bloating. This effect is most pronounced during treatment initiation and tends to diminish over time with continued use. Whilst this mechanism aids weight loss and glycaemic control, it can cause considerable discomfort, particularly after larger meals.
-
Central nervous system effects – GLP-1 receptors are present in the brainstem area postrema and nucleus tractus solitarius, regions involved in nausea and vomiting reflexes. Direct stimulation of these receptors may trigger nausea independently of gastric effects.
-
Altered GI motility – Beyond the stomach, semaglutide affects intestinal transit time throughout the GI tract. Some patients experience accelerated colonic transit (leading to diarrhoea), whilst others develop slower motility (resulting in constipation). Individual variation in receptor distribution and sensitivity likely accounts for these differing presentations.
-
Changes in gut microbiome – Some preliminary research suggests GLP-1 receptor agonists may influence intestinal bacterial composition, though this remains investigational and the clinical significance is currently uncertain.
The dose-dependent nature of these effects explains why gradual titration is recommended in clinical practice. Starting at 0.25 mg weekly for four weeks allows physiological adaptation before escalating to therapeutic doses, thereby reducing the intensity of GI symptoms.
How to Manage Nausea, Vomiting and Diarrhoea on Ozempic
Effective management of GI side effects can significantly improve treatment adherence and patient quality of life. A combination of lifestyle modifications, dietary adjustments, and, when necessary, pharmacological interventions should be considered.
Dietary and lifestyle strategies:
-
Eat smaller, more frequent meals – Consuming five to six small portions throughout the day rather than three large meals reduces gastric distension and may alleviate nausea and bloating.
-
Avoid high-fat and spicy foods – These can exacerbate delayed gastric emptying and trigger nausea. Opt for bland, easily digestible options during the initial treatment phase.
-
Stay well hydrated – Particularly important for patients experiencing vomiting or diarrhoea to prevent dehydration. Sipping water throughout the day is preferable to drinking large volumes at once. Consider oral rehydration salts if fluid losses are significant.
-
Timing of injections – Some patients anecdotally report that administering Ozempic in the evening reduces daytime nausea, though there is no evidence-based preferred time and official guidance does not mandate a specific administration time.
-
Avoid lying down immediately after eating – Remaining upright for at least two hours post-meal may reduce reflux and nausea.
Pharmacological management:
For persistent nausea, short-term antiemetics may be considered:
-
Prochlorperazine (5 mg up to three times daily) or cyclizine (50 mg up to three times daily) are options with fewer restrictions
-
Metoclopramide (10 mg up to three times daily) can be used for up to 5 days only due to risk of extrapyramidal side effects
-
Domperidone (10 mg up to three times daily) can be used for up to 7 days only and is contraindicated in those with cardiac conditions or taking medications that prolong the QT interval
For diarrhoea, loperamide (initially 4 mg, then 2 mg after each loose stool, maximum 16 mg daily) can provide symptomatic relief.
Patients taking sulfonylureas or insulin should discuss dose adjustments with their healthcare provider if experiencing reduced oral intake, to minimise hypoglycaemia risk.
When to seek medical advice:
Patients should contact their healthcare provider promptly if they experience:
-
Persistent vomiting preventing oral intake or medication adherence
-
Signs of dehydration (reduced urine output, dizziness, dry mouth)
-
Inability to keep fluids down for more than 24 hours
Seek urgent medical attention for:
-
Severe, persistent abdominal pain, particularly if radiating to the back (possible pancreatitis)
-
Right upper abdominal pain with fever or yellowing of skin/eyes (possible gallbladder disease)
-
Blood in vomit or stool
-
Severe dehydration (extreme thirst, very dry mouth, little or no urination, weakness, dizziness)
In cases of intolerable side effects despite management strategies, dose adjustment options include extending time at the current dose, stepping back to a previous dose, or temporary treatment interruption. NICE guidance supports individualised treatment approaches, and discontinuation should be considered if GI symptoms significantly impair quality of life.
Suspected adverse reactions should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Alternatives to Ozempic for Type 2 Diabetes Management
For patients unable to tolerate Ozempic due to GI side effects, several evidence-based alternatives exist within and beyond the GLP-1 receptor agonist class. Treatment selection should be guided by individual patient factors including renal function, cardiovascular risk profile, weight management goals, and previous medication history, in line with NICE guideline NG28.
Alternative GLP-1 receptor agonists:
Other agents in this class may be better tolerated by some individuals, though GI side effects are common across the class. Dulaglutide (Trulicity), administered once weekly, has a slightly different side effect profile. Liraglutide (Victoza), a daily injection, allows more flexible dose titration. Exenatide (both twice-daily and once-weekly formulations) represents an older generation GLP-1 agonist. Oral semaglutide (Rybelsus) provides a non-injectable option but still carries similar GI side effect risks. Tirzepatide (Mounjaro), a newer GLP-1/GIP dual agonist, is also available in the UK but has similar GI effects.
SGLT2 inhibitors:
Sodium-glucose co-transporter-2 inhibitors such as empagliflozin, dapagliflozin, and canagliflozin offer cardiovascular and renal protection without significant GI side effects. These agents work by increasing urinary glucose excretion and are particularly suitable for patients with established cardiovascular disease or chronic kidney disease. Common side effects include genital mycotic infections and, rarely, diabetic ketoacidosis. NICE recommends SGLT2 inhibitors as first-line options for patients with cardiovascular disease, heart failure or chronic kidney disease, and as an option when metformin is contraindicated or not tolerated.
DPP-4 inhibitors:
Dipeptidyl peptidase-4 inhibitors (sitagliptin, linagliptin, saxagliptin) enhance endogenous GLP-1 activity with a lower risk of GI side effects compared with GLP-1 receptor agonists. Whilst generally well tolerated, they offer more modest glycaemic improvement and lack the weight loss and cardiovascular benefits of GLP-1 agonists or SGLT2 inhibitors.
Traditional agents:
Metformin remains the cornerstone of type 2 diabetes management, though it too can cause GI upset, particularly diarrhoea. Modified-release formulations may improve tolerability. Sulfonylureas (gliclazide) and pioglitazone represent additional options, though weight gain and hypoglycaemia risk must be considered.
Insulin therapy:
For patients with significant hyperglycaemia or beta-cell failure, basal insulin (such as insulin glargine or degludec) provides effective glycaemic control without GI side effects, though it requires careful dose titration and patient education regarding hypoglycaemia risk.
Treatment decisions should be made collaboratively between patients and healthcare professionals, considering individual circumstances, comorbidities, and treatment goals as outlined in NICE guidance. Regular review and adjustment of diabetes management plans ensure optimal outcomes whilst minimising adverse effects.
Frequently Asked Questions
How long do GI side effects from Ozempic typically last?
Most gastrointestinal side effects from Ozempic are most pronounced during the first few weeks of treatment and tend to diminish over time as the body adapts to the medication. Gradual dose titration helps reduce symptom intensity.
Can I take anti-sickness medication whilst on Ozempic?
Yes, short-term antiemetics such as prochlorperazine or cyclizine may be used to manage persistent nausea. Metoclopramide and domperidone have restricted use (5-7 days maximum) due to potential side effects, so discuss options with your healthcare provider.
When should I seek urgent medical help for GI symptoms on Ozempic?
Seek urgent medical attention if you experience severe persistent abdominal pain (especially radiating to the back), right upper abdominal pain with fever or jaundice, blood in vomit or stool, or signs of severe dehydration such as little or no urination and extreme weakness.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript