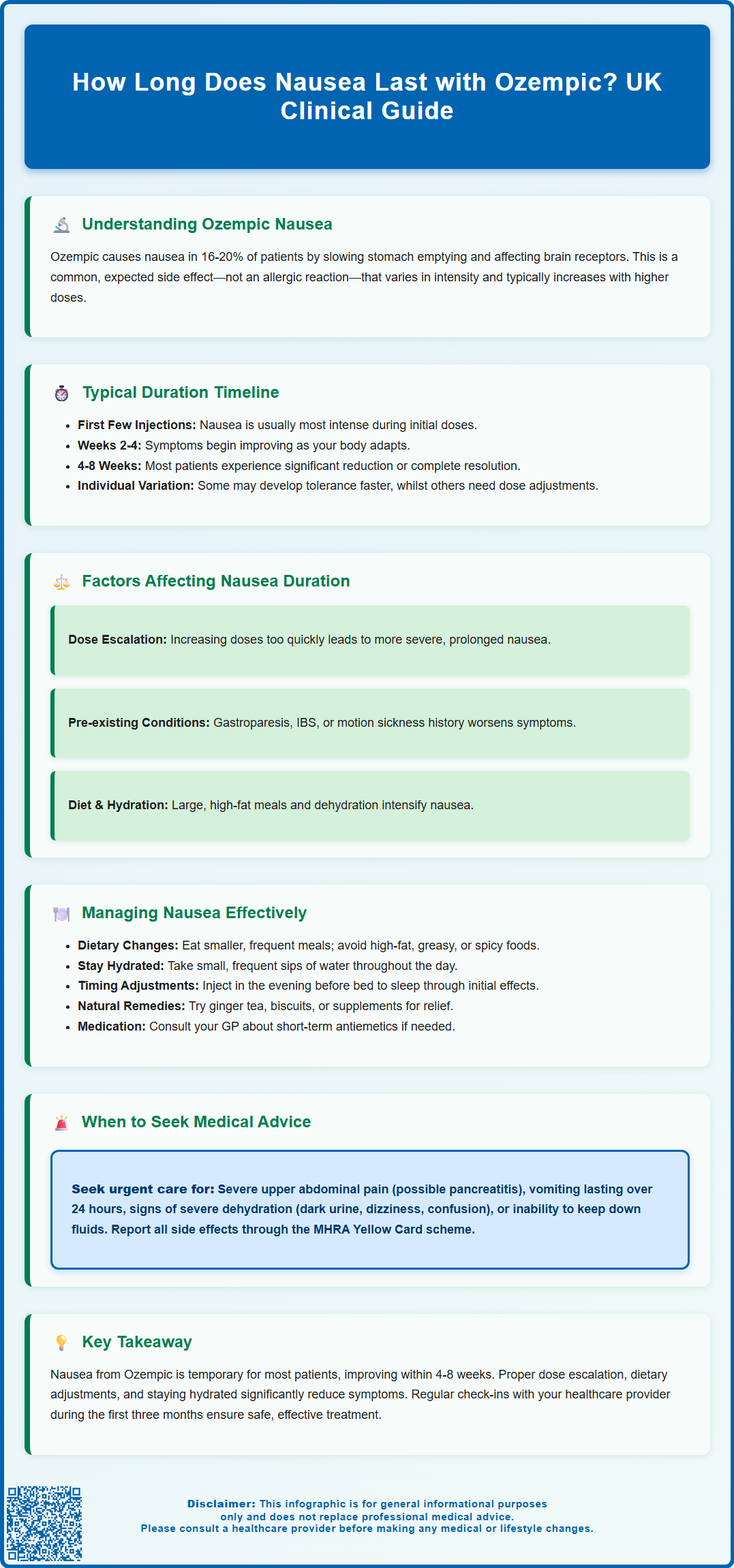
Nausea is one of the most frequently reported side effects when starting Ozempic (semaglutide), affecting approximately 16-20% of patients with type 2 diabetes. Understanding how long does nausea last with Ozempic is crucial for managing expectations and treatment adherence. For most patients, nausea is transient and self-limiting, typically improving within the first 4-8 weeks as the body adapts to the medication. The duration varies considerably between individuals and depends on factors including dose escalation speed, dietary habits, and individual gastrointestinal sensitivity. This article examines the timeline of Ozempic-related nausea, influencing factors, and evidence-based management strategies aligned with UK clinical guidance.
Summary: Ozempic-related nausea typically lasts 4-8 weeks for most patients, with symptoms often improving as the body adapts during the initial titration phase.
- Ozempic is a GLP-1 receptor agonist that slows gastric emptying, causing nausea in approximately 16-20% of patients.
- Nausea is usually most intense during the first few weeks and gradually improves with continued treatment.
- Gradual dose escalation starting at 0.25 mg weekly for four weeks minimises gastrointestinal side effects.
- Dietary modifications, smaller meals, and avoiding high-fat foods can reduce nausea severity and duration.
- Persistent vomiting, severe abdominal pain, or signs of dehydration require prompt medical evaluation.
- The UK MHRA recommends reporting unexpected or severe side effects through the Yellow Card scheme.
Table of Contents
Understanding Nausea as a Side Effect of Ozempic
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in response to food intake, suppresses glucagon release, and slows gastric emptying. This mechanism of action, whilst therapeutically beneficial for glycaemic control and weight management, is directly responsible for one of the most commonly reported adverse effects: nausea.
According to the UK Summary of Product Characteristics (SmPC), nausea is classified as a very common side effect, occurring in approximately 16-20% of patients initiating Ozempic therapy. Other gastrointestinal effects including vomiting, diarrhoea, and constipation are also common and may occur alongside nausea. The slowing of gastric emptying means food remains in the stomach for longer periods, which can trigger feelings of fullness, bloating, and nausea. Additionally, GLP-1 receptors are present in areas of the brain involved in appetite regulation and the emetic response, contributing to these gastrointestinal symptoms.
Key points about Ozempic-related nausea:
-
It is a recognised and expected side effect, not an allergic reaction
-
The intensity varies considerably between individuals
-
It typically correlates with the dose administered
-
Most cases are mild to moderate in severity
Understanding that nausea is a pharmacological consequence of how Ozempic works can help patients and healthcare professionals anticipate and manage this side effect more effectively. It is important to distinguish between expected gastrointestinal symptoms and more serious adverse reactions that may require medical intervention.
It's worth noting that while semaglutide is also available under the brand name Wegovy for weight management, this article focuses on Ozempic's licensed use for type 2 diabetes.
How Long Does Ozempic Nausea Typically Last?
For many patients who experience nausea with Ozempic, symptoms are transient and self-limiting, with improvement often occurring within the first few weeks of treatment. According to the European Medicines Agency's European Public Assessment Report (EPAR), gastrointestinal adverse events typically occur during the initial titration phase, when the body is adapting to the medication's effects on the gastrointestinal system, and tend to decline over time.
The standard UK prescribing regimen for Ozempic begins with a starting dose of 0.25 mg once weekly for four weeks, followed by an increase to 0.5 mg weekly. If additional glycaemic control is needed after at least 4 weeks, the dose can be further increased to 1 mg weekly and subsequently to a maximum of 2 mg weekly if required. This gradual dose escalation is specifically designed to minimise gastrointestinal side effects, including nausea. The UK SmPC advises that if patients experience gastrointestinal symptoms, delaying dose increases or reducing to a previous dose should be considered until symptoms improve.
Timeline of nausea experience:
-
Initial weeks: Nausea often most intense, particularly after the first few injections
-
Subsequent weeks: Symptoms typically begin to improve as the body adapts
-
Beyond initial adaptation: Most patients experience significant reduction or resolution
-
Longer term: A minority of patients may experience persistent symptoms
Clinical experience suggests that while many patients see improvement within 4-8 weeks, the exact timeline varies considerably between individuals. In clinical trials, a proportion of participants discontinued Ozempic due to gastrointestinal symptoms, highlighting that tolerance is not universal.
Patients should be reassured that experiencing nausea does not indicate treatment failure or harm, and that symptom improvement is expected with continued use for most people. Regular review with healthcare professionals during the first three months of treatment allows for monitoring of tolerance and adjustment of management strategies as needed.
Factors That Influence Nausea Duration
Several individual and treatment-related factors can influence both the severity and duration of nausea experienced with Ozempic therapy. Understanding these variables can help healthcare professionals identify patients who may require additional support or modified treatment approaches.
Dose escalation speed is perhaps the most significant modifiable factor. Patients who increase their dose too rapidly, or who skip the recommended 0.25 mg starting phase, are more likely to experience prolonged or severe nausea. The UK SmPC emphasises the importance of gradual titration to improve gastrointestinal tolerability. Some patients may benefit from extending the time spent at lower doses before escalating.
Individual gastrointestinal sensitivity varies considerably. The SmPC includes a specific caution regarding patients with severe gastrointestinal disease, including severe gastroparesis, as Ozempic may potentially worsen existing gastrointestinal motility disorders. Patients with pre-existing conditions such as gastroparesis, functional dyspepsia, or irritable bowel syndrome may experience more pronounced or prolonged symptoms. Similarly, those with a history of motion sickness or medication-induced nausea may be more susceptible.
Dietary habits and meal composition significantly impact nausea duration. Large, high-fat meals can exacerbate symptoms due to Ozempic's effect on gastric emptying. Patients who adapt their eating patterns early in treatment typically report shorter duration of nausea.
Concurrent medications may also play a role. Other drugs that affect gastrointestinal motility or have nausea as a side effect can compound symptoms. A thorough medication review is essential when assessing persistent nausea.
Hydration status is frequently overlooked but important. Dehydration can worsen nausea and delay resolution, creating a problematic cycle if patients reduce fluid intake due to feeling unwell. Prolonged vomiting and dehydration can increase the risk of acute kidney injury, particularly in vulnerable patients, so early intervention is important.
Individual factors such as age and comorbidities may influence how patients experience and adapt to side effects, though responses vary widely between individuals.
Managing and Reducing Nausea While Taking Ozempic
Effective management of Ozempic-related nausea involves a combination of lifestyle modifications, dietary adjustments, and, when necessary, pharmacological interventions. NICE guidance on type 2 diabetes management (NG28) and the technology appraisal for semaglutide (TA623) emphasise the importance of patient education and proactive symptom management to improve treatment adherence.
Dietary modifications form the cornerstone of nausea management:
-
Eat smaller, more frequent meals rather than three large meals daily
-
Avoid high-fat, greasy, or heavily spiced foods that delay gastric emptying further
-
Choose bland, easily digestible options such as toast, crackers, rice, or bananas during symptomatic periods
-
Stay well hydrated with small, frequent sips of water or clear fluids
-
Avoid lying down immediately after eating; remain upright for at least 30–60 minutes
-
Identify and avoid personal trigger foods that worsen symptoms
Injection timing can be optimised to minimise impact. According to the SmPC, Ozempic can be administered at any time of day, with or without meals, but should be given on the same day each week. If necessary, the day of weekly administration can be changed as long as the time between two doses is at least 72 hours. Some patients find that administering Ozempic on an evening before bed, or on a day when they can rest if needed, helps them manage initial post-injection symptoms more comfortably.
Ginger-based remedies, whilst not formally studied with Ozempic specifically, have evidence for reducing nausea in other contexts and may provide symptomatic relief. Ginger tea, ginger biscuits, or ginger supplements are generally safe options.
Antiemetic medications may be considered for patients with persistent or severe nausea. Options include:
-
Metoclopramide (short-term use only, maximum 5 days due to risk of extrapyramidal effects, as per MHRA safety guidance)
-
Domperidone (restricted use in UK due to cardiac risks; requires careful cardiovascular assessment and is contraindicated in certain patients, as per MHRA safety guidance)
-
Prochlorperazine for acute symptomatic relief
-
Cyclizine as an alternative antihistamine-based antiemetic
-
Ondansetron may be considered by prescribers for short-term use (with awareness of QT interval prolongation risk)
When to Seek Medical Advice About Ozempic Side Effects
Whilst nausea is an expected side effect of Ozempic, certain symptoms warrant prompt medical evaluation to exclude more serious complications or conditions requiring intervention. Patients should be educated about red flag symptoms that necessitate contact with their GP or diabetes specialist team.
Seek medical advice within 24–48 hours if:
-
Nausea persists without improvement despite management strategies
-
Symptoms significantly worsen rather than improve over time
-
Nausea is accompanied by persistent vomiting (more than 24 hours) that prevents adequate fluid or medication intake
-
Signs of dehydration develop: dark urine, dizziness, reduced urination, dry mouth, or confusion
-
Significant unintentional weight loss occurs (beyond expected therapeutic effect)
-
Nausea interferes substantially with daily activities, work, or quality of life
-
Recurrent hypoglycaemia occurs, particularly if taking Ozempic alongside insulin or sulfonylureas (medication review may be needed)
Seek urgent medical attention (same day GP, NHS 111, or A&E) if:
-
Severe, persistent abdominal pain, particularly in the upper abdomen, which may indicate pancreatitis (a rare but serious side effect of GLP-1 agonists)
-
Vomiting with severe abdominal pain that radiates to the back
-
Signs of severe dehydration or inability to keep down any fluids
-
Right upper quadrant pain, fever, or yellowing of skin/eyes, which may indicate gallbladder problems (GLP-1 receptor agonists can increase the risk of gallstone formation)
-
Reduced urine output, swelling, or breathlessness which may indicate acute kidney injury from dehydration
-
Allergic reaction symptoms: facial swelling, difficulty breathing, or widespread rash
The MHRA's Yellow Card scheme (yellowcard.mhra.gov.uk) allows patients and healthcare professionals to report suspected side effects directly, contributing to ongoing medication safety monitoring. Patients experiencing unexpected or severe reactions should be encouraged to report these.
Regular follow-up appointments during the first three months of Ozempic therapy provide an opportunity to assess tolerance, review blood glucose control, and adjust treatment plans as necessary. Open communication between patients and healthcare teams is essential for optimising both safety and therapeutic outcomes.
It is important to note that Ozempic is not licensed for use in type 1 diabetes in the UK.
Scientific References
Frequently Asked Questions
Does Ozempic nausea go away on its own?
Yes, for most patients Ozempic-related nausea is transient and self-limiting, typically improving within 4-8 weeks as the body adapts to the medication. Gradual dose escalation and dietary modifications can help reduce symptom duration.
What can I do to reduce nausea while taking Ozempic?
Eat smaller, more frequent meals, avoid high-fat and greasy foods, stay well hydrated, and remain upright after eating. Ginger-based remedies may provide relief, and antiemetic medications can be prescribed by your GP for persistent symptoms.
When should I contact my doctor about Ozempic nausea?
Seek medical advice if nausea persists without improvement, is accompanied by persistent vomiting for more than 24 hours, or if you develop signs of dehydration, severe abdominal pain, or symptoms that significantly interfere with daily activities.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript