Does your metabolism go back to normal after pregnancy? For most women, metabolism does gradually return to pre-pregnancy levels, though the timeline varies considerably. Pregnancy induces profound metabolic changes—including increased basal metabolic rate, insulin resistance, and altered lipid metabolism—to support foetal development. Following delivery, these adaptations reverse over weeks to months, influenced by factors such as breastfeeding, weight retention, sleep, and pre-existing conditions. Understanding postpartum metabolic recovery helps set realistic expectations and identifies when medical review may be warranted. This article explores how pregnancy affects metabolism, recovery timelines, and evidence-based strategies to support metabolic health after childbirth.
Summary: For most women, metabolism does return to pre-pregnancy levels over weeks to months postpartum, though the timeline varies based on individual factors such as breastfeeding status and weight retention.
- Pregnancy increases basal metabolic rate and induces insulin resistance to support foetal growth, changes orchestrated by placental hormones.
- Insulin sensitivity typically improves within days to weeks after delivery in women without gestational diabetes.
- Breastfeeding temporarily elevates metabolic rate above pre-pregnancy levels throughout lactation.
- Women with previous gestational diabetes require fasting plasma glucose testing at 6–13 weeks postpartum and annual HbA1c monitoring thereafter.
- Factors affecting metabolic recovery include breastfeeding status, weight retention, sleep quality, maternal age, and pre-existing metabolic conditions.
- Gradual return to exercise, balanced nutrition, and attendance at postnatal appointments support optimal metabolic recovery.
Table of Contents
How Pregnancy Changes Your Metabolism
Pregnancy induces profound metabolic adaptations to support foetal growth and development. During the first trimester, maternal metabolism remains relatively stable, but significant changes emerge as pregnancy progresses. The basal metabolic rate (BMR) increases during pregnancy, particularly in the later stages, driven primarily by the metabolic demands of the growing foetus, placenta, and increased maternal tissue mass.
Key metabolic changes during pregnancy include:
-
Insulin resistance: Progressive insulin resistance develops, particularly in the second and third trimesters, to ensure adequate glucose supply to the foetus. This physiological adaptation redirects nutrients towards the baby but can predispose some women to gestational diabetes.
-
Altered lipid metabolism: Triglyceride and cholesterol levels rise substantially during pregnancy. Fat storage increases, particularly in early pregnancy, whilst fat mobilisation predominates later.
-
Increased energy expenditure: The body requires additional energy to maintain pregnancy, though individual requirements vary considerably. According to NHS guidance, women generally don't need extra calories until the third trimester, when approximately 200 additional kilocalories daily are needed.
-
Thyroid function changes: Thyroid hormone production increases to support the increased metabolic demands of pregnancy.
These adaptations are orchestrated by placental hormones, including human placental lactogen, oestrogen, and progesterone, which fundamentally alter how the body processes carbohydrates, proteins, and fats. Understanding these changes provides essential context for postpartum metabolic recovery and helps set realistic expectations for the months following childbirth.
Does Your Metabolism Go Back to Normal After Pregnancy?
For most women, metabolism does return to pre-pregnancy levels, though the timeline and completeness of recovery vary considerably between individuals. Basal metabolic rate gradually returns towards pre-pregnancy levels over the months following delivery, with the rate of change influenced by factors such as breastfeeding status and weight loss.
The postpartum period represents a distinct metabolic phase characterised by gradual reversal of pregnancy-induced changes. Insulin sensitivity generally improves after delivery, with most women returning to baseline within weeks to months, provided gestational diabetes resolves. However, women who experienced gestational diabetes face a significantly elevated risk of developing type 2 diabetes later in life. According to NICE guidance, around half of women with previous gestational diabetes may develop type 2 diabetes within 5-10 years, highlighting the importance of ongoing metabolic monitoring.
Important considerations regarding metabolic recovery:
-
Breastfeeding influence: Lactation increases energy expenditure, with requirements varying depending on exclusivity and stage of breastfeeding. This temporarily elevates metabolic rate above pre-pregnancy levels throughout the breastfeeding period.
-
Individual variation: Genetic factors, age, lifestyle, and pre-existing metabolic conditions significantly influence recovery trajectories. Some women may experience persistent metabolic changes, particularly if substantial weight is retained postpartum.
-
Hormonal normalisation: The dramatic hormonal shifts following delivery affect metabolic regulation. Oestrogen and progesterone levels decline rapidly after birth, whilst prolactin rises in breastfeeding women, each influencing metabolic processes differently.
There is no official link suggesting permanent metabolic impairment from uncomplicated pregnancy itself, though pregnancy can unmask underlying metabolic vulnerabilities that warrant medical attention and lifestyle modification.
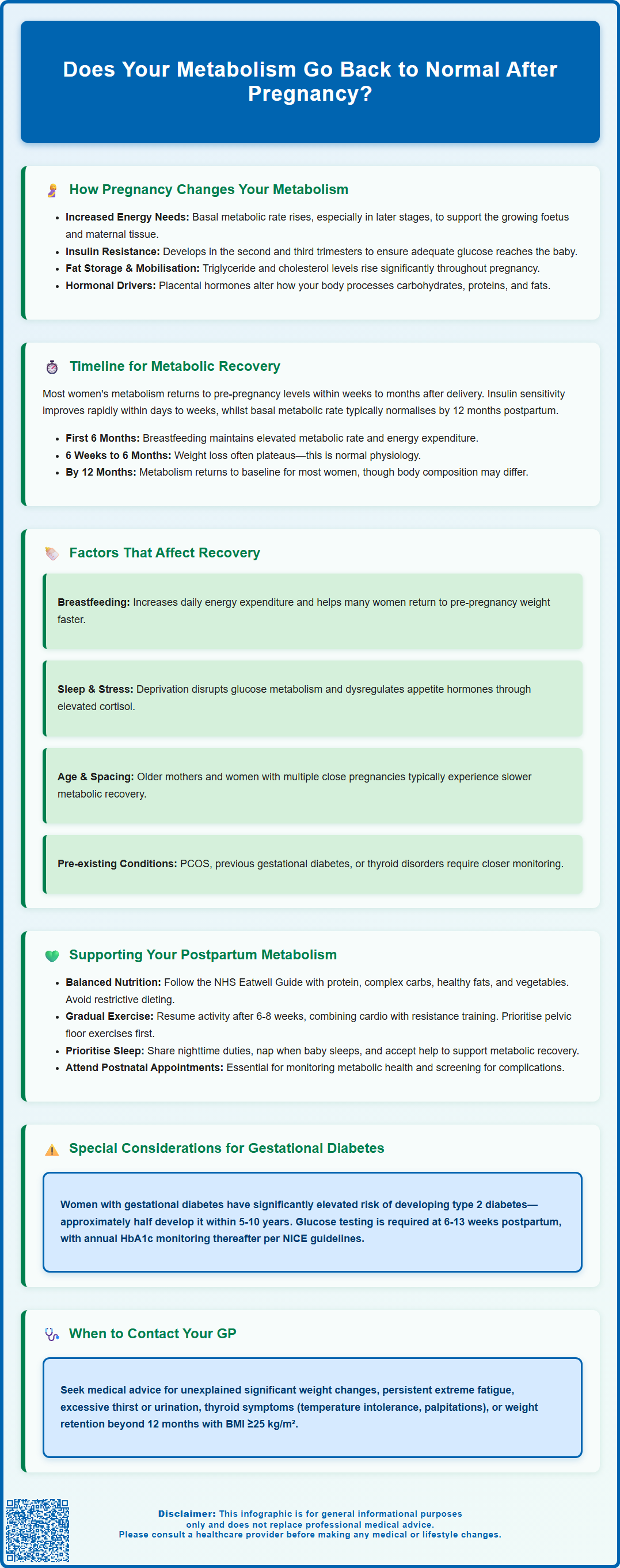
Timeline for Metabolic Recovery After Giving Birth
Metabolic recovery follows a generally predictable pattern, though individual experiences vary. Understanding this timeline helps set realistic expectations and identify when medical review may be warranted.
Immediate postpartum (0–6 weeks): The most dramatic metabolic shifts occur immediately after delivery. Basal metabolic rate begins declining towards pre-pregnancy levels within days, though it remains elevated, particularly in breastfeeding women. Insulin sensitivity improves rapidly after birth, with pregnancy-related insulin resistance typically resolving over days to weeks in women without gestational diabetes. Fluid retention decreases substantially, contributing to initial weight loss. The NHS recommends a postnatal check at 6–8 weeks to assess overall recovery, including metabolic health markers if concerns exist.
Early postpartum (6 weeks–6 months): Metabolic rate continues normalising, though breastfeeding maintains elevated energy expenditure. Thyroid function typically stabilises, though postpartum thyroiditis affects some women, causing temporary hyper- or hypothyroidism. Weight loss often plateaus during this period, which can be frustrating but represents normal physiology rather than metabolic dysfunction. Lipid profiles gradually return towards baseline, though complete normalisation may require several months.
Late postpartum (6–12 months): For most women, basal metabolic rate approaches pre-pregnancy levels by 12 months postpartum, assuming return to pre-pregnancy weight. However, body composition may differ from pre-pregnancy, with potential increases in fat mass and decreases in lean muscle mass, which can affect metabolic efficiency. Women with ongoing concerns about weight retention beyond 12 months should consult their GP, as this may indicate underlying metabolic issues requiring investigation or intervention, particularly if BMI is 25 kg/m² or above.
Factors That Affect Postpartum Metabolism
Multiple interconnected factors influence how quickly and completely metabolism returns to pre-pregnancy status. Recognising these variables helps women understand their individual recovery trajectory and identify modifiable factors.
Breastfeeding status: Lactation significantly affects postpartum metabolism, increasing daily energy expenditure. Exclusive breastfeeding promotes earlier return to pre-pregnancy weight in many women, though individual responses vary. The metabolic effects of breastfeeding extend beyond simple calorie expenditure, influencing hormone profiles, insulin sensitivity, and fat mobilisation patterns.
Weight retention and body composition: Postpartum weight retention, particularly when resulting in a BMI of 25 kg/m² or above, is associated with long-term metabolic consequences, including increased risk of obesity and metabolic syndrome. Body composition changes—specifically increased visceral adiposity—can impair metabolic function even when overall weight appears acceptable. Gradual, sustainable weight loss through balanced nutrition and physical activity represents the safest approach.
Sleep deprivation and stress: Chronic sleep disruption, nearly universal in new parents, adversely affects metabolic regulation. Poor sleep impairs glucose metabolism, increases appetite-regulating hormone dysregulation, and promotes weight retention. Elevated cortisol from chronic stress similarly disrupts metabolic homeostasis.
Age and parity: Maternal age influences metabolic recovery, with older mothers often experiencing slower normalisation. Multiple pregnancies in close succession may compound metabolic stress, potentially preventing full recovery between pregnancies.
Pre-existing conditions: Women with polycystic ovary syndrome (PCOS), previous gestational diabetes, or thyroid disorders face greater challenges in metabolic recovery and require closer monitoring. NICE recommends that women with previous gestational diabetes have a fasting plasma glucose test at 6–13 weeks after birth, and annual HbA1c testing thereafter to detect early progression to type 2 diabetes.
Supporting Your Metabolism After Pregnancy
Evidence-based strategies can optimise metabolic recovery whilst supporting overall postpartum health. These approaches should be implemented gradually, respecting the physical and emotional demands of new parenthood.
Nutrition for metabolic health: A balanced diet rich in whole foods supports metabolic recovery without compromising breastfeeding or energy levels. Focus on balanced meals containing protein, complex carbohydrates, healthy fats, and abundant vegetables whilst avoiding restrictive dieting, which can impair metabolism and milk production. The NHS Eatwell Guide provides an appropriate nutritional framework for postpartum women, emphasising variety and balance rather than specific macronutrient targets.
Physical activity: Gradual return to exercise, following appropriate postnatal recovery (typically 6–8 weeks for uncomplicated vaginal delivery, longer after caesarean section), supports metabolic health. Combining cardiovascular exercise with resistance training optimises body composition and metabolic function. Start conservatively and progress gradually, ideally with guidance from physiotherapists specialising in postnatal care. Pelvic floor exercises should be prioritised before resuming high-impact activities, in line with UK Chief Medical Officers' physical activity guidelines.
Sleep optimisation: Whilst challenging with a newborn, prioritising sleep when possible supports metabolic recovery. Strategies include sharing night-time responsibilities, napping when the baby sleeps, and seeking support from partners or family members.
Medical monitoring: Attend all scheduled postnatal appointments and request additional review if concerns arise. Women with gestational diabetes require a fasting plasma glucose test at 6–13 weeks postpartum (or HbA1c if fasting glucose is not possible) and annual HbA1c testing thereafter, as recommended by NICE guidance.
When to seek medical advice: Contact your GP if you experience significant unexplained weight gain or loss, persistent extreme fatigue, excessive thirst or urination (potential diabetes indicators), or symptoms suggesting thyroid dysfunction (heat/cold intolerance, palpitations, mood changes). Early identification and management of metabolic issues optimises long-term health outcomes.
Frequently Asked Questions
How long does it take for metabolism to return to normal after pregnancy?
For most women, basal metabolic rate approaches pre-pregnancy levels by 12 months postpartum, assuming return to pre-pregnancy weight. However, breastfeeding maintains elevated energy expenditure throughout lactation, and individual recovery timelines vary based on factors such as age, weight retention, and pre-existing conditions.
Does breastfeeding affect postpartum metabolism?
Yes, breastfeeding significantly increases daily energy expenditure and temporarily elevates metabolic rate above pre-pregnancy levels. Lactation influences hormone profiles, insulin sensitivity, and fat mobilisation patterns, often promoting earlier return to pre-pregnancy weight, though individual responses vary.
When should I see a GP about postpartum metabolic concerns?
Contact your GP if you experience significant unexplained weight changes, persistent extreme fatigue, excessive thirst or urination, or symptoms suggesting thyroid dysfunction such as heat or cold intolerance, palpitations, or mood changes. Women with previous gestational diabetes require fasting plasma glucose testing at 6–13 weeks postpartum and annual HbA1c monitoring.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












