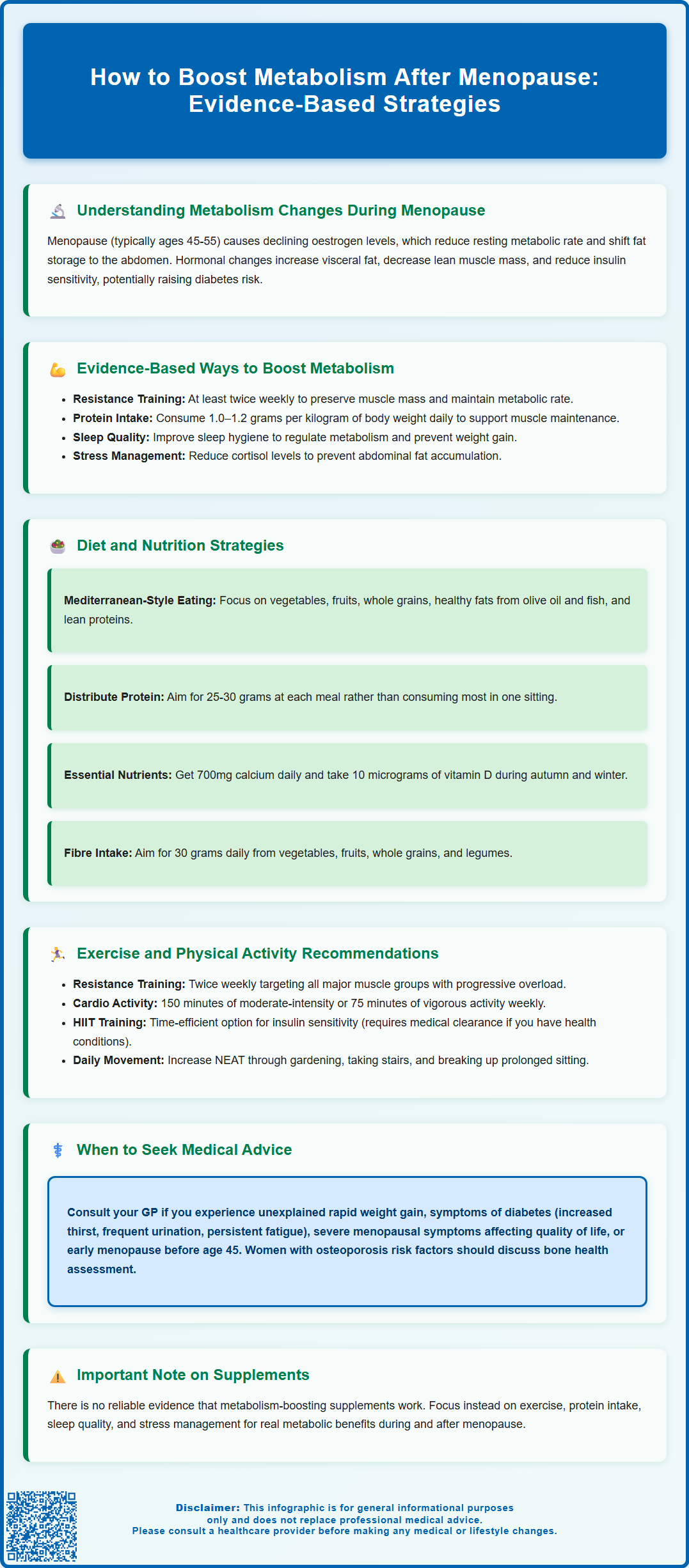
Menopause brings significant metabolic changes that many women find challenging, including a slower resting metabolic rate, increased abdominal fat, and reduced muscle mass. These shifts result primarily from declining oestrogen levels, though age-related factors also contribute. Whilst metabolism naturally slows during this transition, evidence-based strategies can effectively support metabolic health. This article explores how to boost metabolism after menopause through resistance training, optimised nutrition, improved sleep quality, and lifestyle modifications. Understanding the physiological changes and implementing practical, sustainable approaches can help women maintain healthy weight, body composition, and overall wellbeing during and after the menopausal transition.
Summary: Metabolism after menopause can be supported through resistance training at least twice weekly, adequate protein intake (1.0–1.2g per kg body weight daily), improved sleep quality, and Mediterranean-style dietary patterns.
- Declining oestrogen during menopause reduces resting metabolic rate and increases visceral fat accumulation around internal organs.
- Resistance exercise preserves lean muscle mass, which burns more calories at rest than fat tissue, helping maintain metabolic rate.
- Protein has a higher thermic effect than other macronutrients and supports muscle protein synthesis when combined with strength training.
- Poor sleep quality alters glucose metabolism and increases appetite hormones, negatively affecting metabolic function.
- Unexplained rapid weight gain, diabetes symptoms, or severe menopausal symptoms warrant GP consultation to exclude underlying conditions.
- Early menopause (before age 45) or premature ovarian insufficiency (before age 40) requires medical review for appropriate management.
Table of Contents
Understanding Metabolism Changes During Menopause
Menopause marks a significant physiological transition in women's lives, typically occurring between ages 45 and 55, characterised by the permanent cessation of menstruation. During this period, declining oestrogen levels trigger numerous metabolic changes that can affect body composition, energy expenditure, and overall health.
The hormonal mechanism behind metabolic changes involves the reduction in oestrogen production by the ovaries. Oestrogen plays a crucial role in regulating metabolism, influencing how the body stores fat and maintains muscle mass. As oestrogen levels decline, women often experience a decrease in resting metabolic rate (RMR)—the number of calories the body burns at rest. Research suggests this decline may occur, though individual variation is considerable and estimates vary widely.
Additionally, the menopausal transition is associated with changes in body composition, including:
-
Increased visceral adiposity (fat stored around internal organs)
-
Reduced lean muscle mass (sarcopenia)
-
Altered fat distribution, with more fat accumulating around the abdomen rather than hips and thighs
-
Decreased insulin sensitivity, potentially increasing diabetes risk
These metabolic shifts are not solely attributable to hormonal changes. Age-related factors, including reduced physical activity, changes in sleep patterns, and lifestyle modifications, also contribute significantly. Understanding these physiological changes provides the foundation for implementing evidence-based strategies to support metabolic health during and after the menopausal transition.
It's important to note that early menopause (before age 45) or premature ovarian insufficiency (before age 40) warrant discussion with a GP or menopause specialist, as these conditions may require specific management approaches for both symptoms and long-term health.
Evidence-Based Ways to Boost Metabolism After Menopause
Whilst there is no single intervention that dramatically reverses menopausal metabolic changes, a combination of evidence-based approaches can effectively support metabolic function and overall health during this life stage.
Resistance training and muscle preservation represent the most robust evidence-based strategy for maintaining metabolic rate. Muscle tissue is metabolically active, burning more calories at rest than fat tissue. Studies demonstrate that regular resistance exercise can help preserve or even increase lean muscle mass, thereby supporting resting metabolic rate. The UK Chief Medical Officers' physical activity guidelines emphasise the importance of muscle-strengthening activities at least twice weekly for adults, including postmenopausal women.
Protein intake optimisation is increasingly recognised as crucial for metabolic health after menopause. Research suggests that adequate protein consumption (approximately 1.0–1.2 grams per kilogram of body weight daily for healthy older adults) supports muscle protein synthesis, particularly when combined with resistance exercise. Protein also has a higher thermic effect than carbohydrates or fats, meaning the body expends more energy digesting and processing it. Those with kidney disease should discuss protein intake with their healthcare provider.
Sleep quality and circadian rhythm regulation significantly influence metabolic function. Poor sleep is associated with altered glucose metabolism, increased appetite hormones, and weight gain. The British Menopause Society acknowledges that sleep disturbances are common during menopause. Addressing these through sleep hygiene measures, cognitive behavioural therapy for insomnia (CBT-I), or, when appropriate, medical intervention including HRT for vasomotor-related sleep disturbance, can support metabolic health.
Stress management should not be overlooked, as chronic stress elevates cortisol levels, which can promote abdominal fat accumulation and insulin resistance. Stress reduction techniques, including mindfulness-based interventions, may offer benefits for overall wellbeing, though evidence for specific metabolic effects varies. Additionally, moderating alcohol intake and smoking cessation can positively impact metabolic health. There is no reliable evidence linking specific 'metabolism-boosting' supplements with clinically significant metabolic improvements, and women should approach such products with caution.
Diet and Nutrition Strategies for Metabolic Health
Nutritional strategies play a fundamental role in supporting metabolic health after menopause, with evidence favouring whole-food, balanced approaches rather than restrictive dieting.
Mediterranean-style dietary patterns have substantial evidence supporting their benefits for postmenopausal women. This approach emphasises:
-
Abundant vegetables, fruits, and whole grains providing fibre and micronutrients
-
Healthy fats from olive oil, nuts, and oily fish rich in omega-3 fatty acids
-
Moderate portions of lean protein from fish, poultry, legumes, and pulses
-
Limited processed foods, refined sugars, and saturated fats
Research indicates this dietary pattern supports cardiovascular health, helps maintain healthy weight, and may improve insulin sensitivity—all relevant concerns for postmenopausal women. The UK Eatwell Guide provides similar principles for a balanced diet.
Adequate protein distribution throughout the day appears more beneficial than consuming most protein in a single meal. Distributing protein intake across breakfast, lunch, and dinner (approximately 25–30 grams per meal) may optimally stimulate muscle protein synthesis. Good protein sources include lean meats, fish, eggs, dairy products, legumes, and soya-based foods.
Calcium and vitamin D intake warrant particular attention during and after menopause due to increased osteoporosis risk. The NHS recommends adults obtain 700mg of calcium daily through dietary sources such as dairy products, fortified plant-based alternatives, leafy green vegetables, and tinned fish with bones. Vitamin D supplementation (10 micrograms daily) is advised for UK adults during autumn and winter months, with year-round supplementation recommended for those with limited sun exposure, darker skin, or who cover most of their skin when outdoors.
Fibre intake supports metabolic health through multiple mechanisms, including improved glycaemic control, enhanced satiety, and beneficial effects on gut microbiota. The recommended intake is 30 grams daily from varied sources including vegetables, fruits, whole grains, and legumes. Hydration is also essential, as adequate fluid intake supports all metabolic processes, with water being the preferred beverage choice over sugary drinks.
Exercise and Physical Activity Recommendations
Physical activity represents one of the most effective interventions for supporting metabolic health after menopause, with benefits extending beyond calorie expenditure to include improvements in insulin sensitivity, body composition, and cardiovascular health.
Resistance training should form the cornerstone of any exercise programme for postmenopausal women. The UK Chief Medical Officers' physical activity guidelines recommend muscle-strengthening activities on at least two days per week, targeting all major muscle groups. This can include:
-
Weight training using free weights or resistance machines
-
Bodyweight exercises such as press-ups, squats, and lunges
-
Resistance band exercises
-
Pilates or similar resistance-based classes (ensuring sufficient intensity to challenge muscles)
Progressive overload—gradually increasing resistance or repetitions—is essential for continued muscle adaptation and metabolic benefits. Women new to resistance training should consider guidance from qualified fitness professionals to ensure proper technique and appropriate progression.
Cardiovascular exercise remains important for overall health and calorie expenditure. The guidelines recommend at least 150 minutes of moderate-intensity aerobic activity (such as brisk walking, cycling, or swimming) or 75 minutes of vigorous-intensity activity weekly. Moderate intensity means exercising at a level where conversation is possible but somewhat challenging.
High-intensity interval training (HIIT) has emerged as a time-efficient option, involving short bursts of intense activity alternated with recovery periods. Evidence suggests HIIT can improve insulin sensitivity and cardiovascular fitness in postmenopausal women, though it may not be suitable for everyone. Those with cardiovascular disease, joint problems, or other health conditions should consult their GP before starting vigorous exercise programmes.
Non-exercise activity thermogenesis (NEAT)—the energy expended during daily activities outside formal exercise—contributes significantly to total energy expenditure. Increasing NEAT through activities like gardening, housework, taking stairs, and reducing sedentary time can meaningfully support metabolic health. The NHS recommends minimising sedentary time and breaking up long periods of sitting as regularly as possible throughout the day.
When to Seek Medical Advice About Metabolic Changes
Whilst metabolic changes during menopause are common, certain symptoms or circumstances warrant medical evaluation to exclude underlying conditions or assess whether additional interventions may be beneficial.
Unexplained or rapid weight gain despite maintaining healthy lifestyle habits should prompt consultation with a GP. Whilst some weight change during menopause is common, significant or sudden increases may indicate thyroid dysfunction, particularly hypothyroidism, which becomes more prevalent with age. Thyroid function tests (TSH and free T4) can readily identify this treatable condition. Additionally, conditions such as Cushing's syndrome or polycystic ovary syndrome (PCOS), though less common, can affect metabolism and weight.
Symptoms suggesting diabetes or non-diabetic hyperglycaemia (prediabetes) require prompt medical assessment. These include:
-
Increased thirst and urination
-
Persistent fatigue
-
Blurred vision
-
Slow-healing wounds or recurrent infections
-
Unexplained weight loss (in type 1 diabetes)
Postmenopausal women have increased diabetes risk. NICE recommends risk assessment and blood glucose or HbA1c testing for individuals with risk factors including obesity, family history, or certain ethnic backgrounds. Early detection enables timely intervention.
Severe menopausal symptoms affecting quality of life, including debilitating hot flushes, night sweats, mood changes, or sleep disturbances, merit discussion with a healthcare professional. Hormone replacement therapy (HRT) may be appropriate for some women to address symptoms and protect bone health, though decisions should be individualised based on personal and family medical history. HRT is not prescribed specifically for weight management.
Early menopause (before age 45) or premature ovarian insufficiency (before age 40) should always prompt medical review, as these conditions increase long-term health risks and typically warrant consideration of HRT until at least the average age of menopause.
Concerns about bone health are relevant given the increased osteoporosis risk after menopause. Women with risk factors—including early menopause, prolonged amenorrhoea, low body weight, family history of osteoporosis, or previous fragility fractures—should discuss bone health assessment with their GP. Tools such as FRAX or QFracture can help determine if bone density scanning (DXA) is indicated. Finally, if lifestyle modifications have been implemented consistently for several months without expected improvements in metabolic health markers, medical review can help identify any barriers or additional strategies that may be beneficial.
Frequently Asked Questions
Why does metabolism slow down after menopause?
Declining oestrogen levels during menopause reduce resting metabolic rate and alter body composition, leading to decreased muscle mass and increased visceral fat. Age-related factors such as reduced physical activity and changes in sleep patterns also contribute to metabolic slowing.
What type of exercise is most effective for boosting metabolism after menopause?
Resistance training is the most effective exercise for maintaining metabolic rate after menopause, as it preserves or increases lean muscle mass. UK guidelines recommend muscle-strengthening activities targeting all major muscle groups at least twice weekly, combined with 150 minutes of moderate-intensity aerobic activity.
When should I see a doctor about metabolic changes during menopause?
Consult your GP if you experience unexplained rapid weight gain, symptoms suggesting diabetes (increased thirst, frequent urination, persistent fatigue), severe menopausal symptoms affecting quality of life, or if menopause occurs before age 45. These situations may require medical assessment to exclude underlying conditions or consider additional interventions.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript