Does sugar slow metabolism? This common question reflects widespread concern about sugar's impact on metabolic health. Whilst sugar does not directly reduce basal metabolic rate in healthy individuals, chronic excessive sugar intake can contribute to metabolic dysregulation, insulin resistance, and conditions that indirectly affect energy balance. Understanding the nuanced relationship between sugar consumption and metabolic function is essential for making informed dietary choices. This article examines the evidence on how sugar affects metabolism, explores the link between sugar intake and metabolic rate, and provides evidence-based guidance aligned with NHS and NICE recommendations for optimising metabolic health through appropriate sugar consumption.
Summary: Sugar does not directly slow basal metabolic rate, but chronic excessive sugar intake can contribute to insulin resistance and metabolic dysregulation that indirectly affects metabolic health.
- Basal metabolic rate is primarily determined by body composition, age, sex, and genetics rather than sugar intake alone.
- Excessive sugar consumption, particularly from sugar-sweetened beverages, is associated with insulin resistance, hepatic fat accumulation, and altered lipid profiles.
- SACN recommends limiting free sugars to less than 5% of total energy intake (approximately 30g daily for adults) to minimise metabolic and dental health risks.
- Reducing excessive sugar intake can improve insulin sensitivity, support weight management, and enhance lipid profiles, especially within a balanced dietary pattern.
- Patients with elevated BMI, increased waist circumference, family history of diabetes, or elevated HbA1c should have dietary sugar intake assessed as part of metabolic health screening.
Table of Contents
How Sugar Affects Your Metabolism
Metabolism encompasses all biochemical processes that convert nutrients into energy and maintain cellular function. Sugar, particularly in the form of glucose and fructose, plays a central role in metabolic pathways, but the relationship between sugar consumption and metabolic rate is more nuanced than commonly portrayed.
When you consume sugar, it is rapidly absorbed into the bloodstream, triggering insulin release from the pancreas. Insulin facilitates glucose uptake into many cells for immediate energy use or storage as glycogen in the liver and muscles (though some tissues like the brain, liver and red blood cells can take up glucose independently of insulin). When glycogen stores are full, additional glucose may be converted to fatty acids through de novo lipogenesis, though this process is typically modest unless carbohydrate intake is very high or in energy surplus. This metabolic flexibility allows the body to manage varying energy demands efficiently.
However, chronic excessive sugar intake—especially from added sugars in processed foods and sugar-sweetened beverages—can contribute to metabolic dysregulation. High sugar consumption, particularly in the context of excess energy intake, is associated with:
-
Insulin resistance: Cells become less responsive to insulin, requiring higher levels to achieve glucose uptake
-
Hepatic fat accumulation: Particularly with high intakes of sugar-sweetened beverages and excess energy consumption
-
Altered lipid profiles: Elevated triglycerides and reduced HDL cholesterol
-
Inflammatory responses: Potential activation of inflammatory pathways that may affect metabolic function
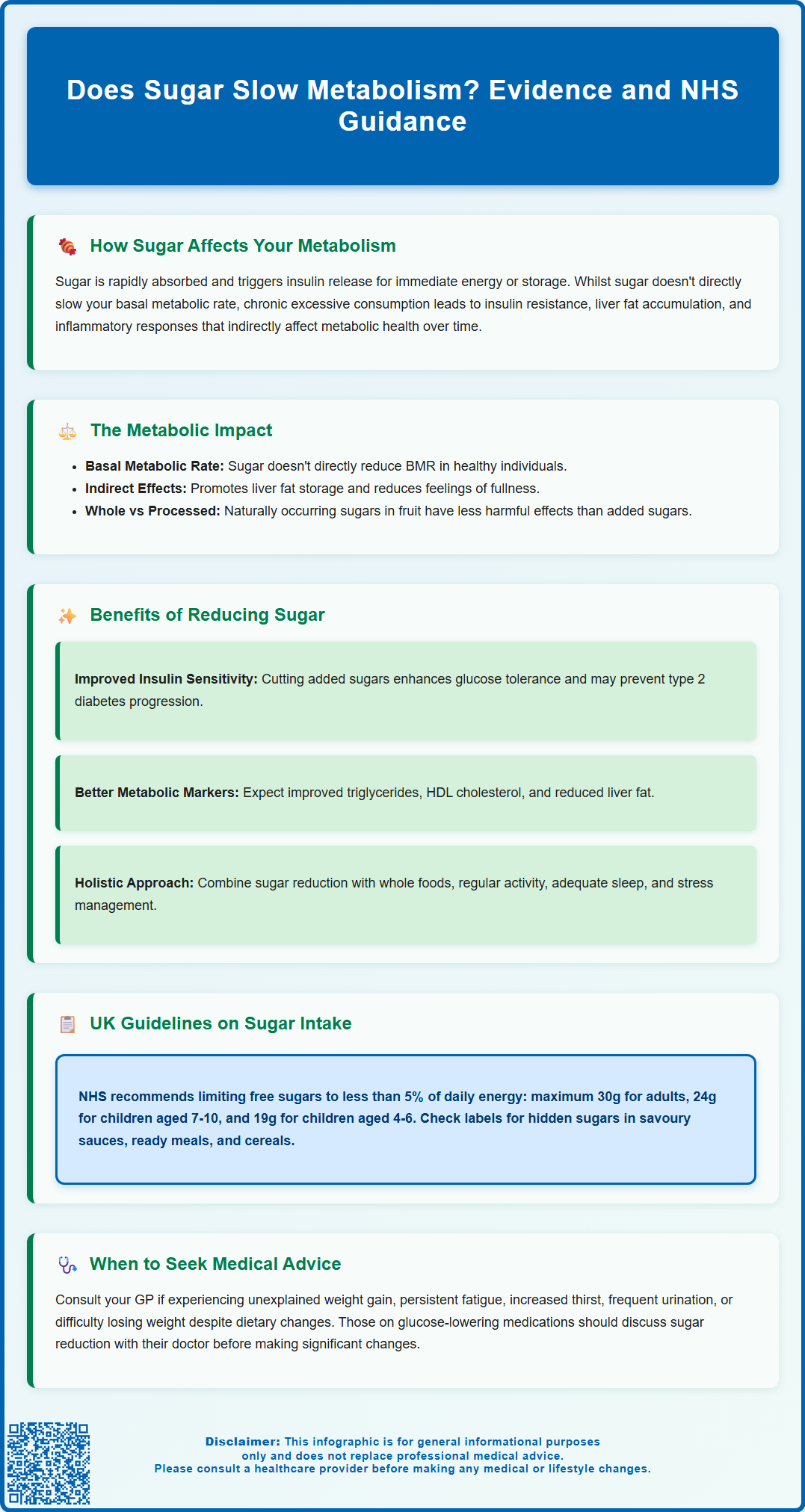
The Link Between Sugar Intake and Metabolic Rate
The question of whether sugar directly slows metabolic rate requires careful examination of available evidence. Basal metabolic rate (BMR), which accounts for 60–75% of total daily energy expenditure, is primarily determined by body composition, age, sex, and genetic factors. There is no robust clinical evidence demonstrating that sugar consumption directly reduces BMR in healthy individuals.
However, the metabolic effects of chronic high sugar intake can create indirect pathways that influence energy balance and body composition. Research suggests that diets high in added sugars may promote:
-
Preferential fat storage: Fructose metabolism in the liver may promote lipogenesis, potentially increasing adipose tissue accumulation, particularly in energy surplus
-
Reduced satiety: Sugar-sweetened beverages provide calories without triggering the same satiety signals as solid foods, leading to passive overconsumption
-
Altered thermogenesis: Some studies suggest high-sugar diets might affect diet-induced thermogenesis—the energy expended digesting and processing food—though evidence remains inconsistent
The NHS and Scientific Advisory Committee on Nutrition (SACN) emphasise that excessive sugar intake contributes to obesity, type 2 diabetes, and cardiovascular disease, all of which are associated with metabolic dysfunction. Obesity itself can alter metabolic rate: whilst absolute energy expenditure may increase with greater body mass, metabolic efficiency per kilogram of body weight may decrease, and insulin resistance can impair cellular energy utilisation.
It is worth noting that the type of sugar matters. Naturally occurring sugars in whole fruits come packaged with fibre, vitamins, and phytonutrients that modulate absorption and metabolic impact, whereas added sugars in processed foods lack these protective factors. The SACN recommends limiting free sugars to no more than 5% of total energy intake—approximately 30g daily for adults—to minimise metabolic and dental health risks. Remember that fruit juices and smoothies count as free sugars and should be limited to 150ml per day.
Does Reducing Sugar Improve Metabolic Function?
Evidence consistently demonstrates that reducing excessive sugar intake can yield improvements in metabolic health markers, though the magnitude of benefit varies among individuals. Clinical trials and observational studies have documented several positive outcomes associated with sugar reduction.
Improvements in insulin sensitivity represent one of the most significant benefits. When individuals reduce added sugar consumption, particularly from sugar-sweetened beverages, studies show decreased fasting insulin levels and improved glucose tolerance. This is especially relevant for those with prediabetes or metabolic syndrome, where even modest dietary changes can help delay or prevent progression to type 2 diabetes.
Reducing sugar intake has also been associated with:
-
Weight management: Modest weight reduction may occur when sugar-sweetened beverages are eliminated, especially if overall energy intake decreases
-
Improved lipid profiles: Potential improvements in triglycerides and HDL cholesterol levels
-
Reduced hepatic fat: Potential decreases in liver fat content in individuals with non-alcoholic fatty liver disease
-
Blood pressure: Modest improvements in some studies, particularly when part of broader dietary improvements
However, it is important to qualify that reducing sugar alone does not guarantee metabolic improvement if overall caloric intake remains excessive or if the diet is otherwise nutritionally poor. The metabolic benefits are most pronounced when sugar reduction occurs within the context of a balanced dietary pattern emphasising whole foods, adequate protein, healthy fats, and fibre.
For patients concerned about metabolic health, NICE guidance recommends a holistic approach that includes regular physical activity, adequate sleep, and stress management alongside dietary modification. Those with existing metabolic conditions should consult their GP or a registered dietitian for personalised advice. People taking glucose-lowering medications should seek medical advice before making substantial changes to sugar intake, as medication adjustments may be needed. Those at high risk of type 2 diabetes may be eligible for the NHS Diabetes Prevention Programme.
Evidence-Based Guidance on Sugar and Metabolism
Current UK clinical guidance provides clear recommendations for sugar intake based on extensive epidemiological and interventional research. The SACN recommendation of limiting free sugars to less than 5% of total energy intake aligns with WHO guidance and is supported by evidence linking excessive sugar consumption to obesity, type 2 diabetes, and cardiovascular disease.
For practical implementation, this translates to:
-
Maximum 30g daily for adults (approximately 7 teaspoons)
-
Maximum 24g daily for children aged 7–10 years
-
Maximum 19g daily for children aged 4–6 years
-
For children under 4 years: avoid sugar-sweetened drinks, do not add sugar to foods, and limit foods with added sugars
The NHS Eatwell Guide emphasises obtaining carbohydrates primarily from whole grains, fruits, vegetables, and pulses rather than foods high in free sugars. Reading nutrition labels is essential, as added sugars appear in unexpected products including savoury sauces, ready meals, and breakfast cereals. Note that 'of which sugars' on labels includes both natural and free sugars. Ingredients listed as sucrose, glucose, fructose, maltose, honey, syrups, and concentrated fruit juices all contribute to free sugar intake.
From a clinical perspective, healthcare professionals should consider dietary assessment including free sugar intake as part of metabolic health screening, particularly for patients with:
-
Elevated BMI (≥25 kg/m² for white populations; ≥23 kg/m² for South Asian, Chinese, and Black populations)
-
Increased waist circumference (men: ≥94 cm white, ≥90 cm South Asian; women: ≥80 cm)
-
Family history of type 2 diabetes or cardiovascular disease
-
Elevated HbA1c (42–47 mmol/mol or 6.0–6.4% indicates high risk; ≥48 mmol/mol or 6.5% indicates diabetes)
-
Elevated fasting glucose (5.5–6.9 mmol/L indicates elevated risk; ≥7.0 mmol/L indicates diabetes)
-
Diagnosed metabolic syndrome or non-alcoholic fatty liver disease
When to seek medical advice: Patients experiencing unexplained weight gain, persistent fatigue, increased thirst, frequent urination, or difficulty losing weight despite dietary efforts should consult their GP. These symptoms may indicate underlying metabolic dysfunction requiring investigation.
Whilst there is no established link between moderate sugar consumption and directly "slowing" metabolism in healthy individuals, the cumulative metabolic effects of excessive sugar intake are well-established. Evidence-based practice supports sugar reduction as one component of comprehensive metabolic health management, integrated with physical activity, weight management, and regular clinical monitoring where indicated.
Frequently Asked Questions
Can eating too much sugar cause weight gain even if I don't eat more calories?
Sugar itself does not cause weight gain independently of total calorie intake. However, sugar-sweetened beverages provide calories without triggering the same satiety signals as solid foods, which can lead to passive overconsumption and weight gain over time.
How much sugar should I eat daily to maintain healthy metabolism?
The Scientific Advisory Committee on Nutrition recommends limiting free sugars to less than 5% of total energy intake, which translates to a maximum of 30g daily for adults (approximately 7 teaspoons). This includes sugars added to foods and those naturally present in honey, syrups, and fruit juices.
Will cutting out sugar improve my insulin resistance?
Reducing excessive sugar intake, particularly from sugar-sweetened beverages, can improve insulin sensitivity and glucose tolerance, especially in individuals with prediabetes or metabolic syndrome. However, improvements are most pronounced when sugar reduction occurs within a balanced dietary pattern that includes whole foods, adequate protein, healthy fats, and fibre.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript