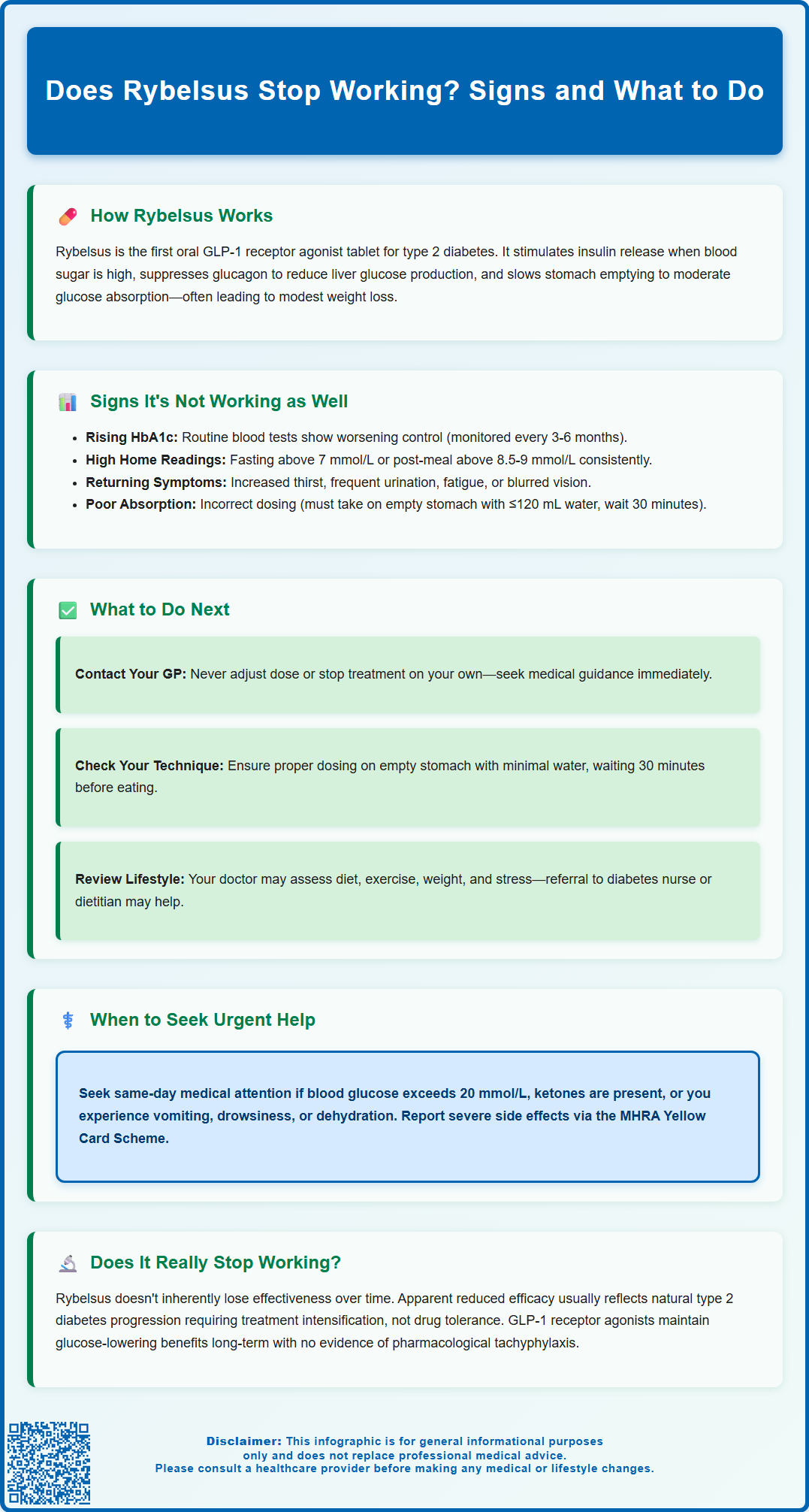
Does Rybelsus stop working over time? Many patients taking this oral GLP-1 receptor agonist for type 2 diabetes wonder whether its glucose-lowering effects diminish with continued use. Rybelsus (semaglutide) works by mimicking natural incretin hormones to stimulate insulin release, suppress glucagon, and slow gastric emptying. Whilst type 2 diabetes is a progressive condition that often requires treatment intensification, there is no evidence that Rybelsus itself loses pharmacological effectiveness through repeated use. This article explains how to recognise signs of inadequate glycaemic control, what factors may contribute to apparent treatment failure, and when to seek medical review for treatment adjustment.
Summary: Rybelsus does not inherently stop working over time, but type 2 diabetes is progressive and may require treatment intensification as beta-cell function declines.
- Rybelsus (semaglutide) is an oral GLP-1 receptor agonist that stimulates insulin secretion, suppresses glucagon, and slows gastric emptying in a glucose-dependent manner.
- Rising HbA1c levels, persistently elevated blood glucose readings, or return of hyperglycaemic symptoms may indicate inadequate glycaemic control requiring medical review.
- There is no evidence of pharmacological tachyphylaxis with Rybelsus; apparent loss of efficacy often reflects disease progression, adherence issues, or lifestyle changes.
- Rybelsus must be taken on an empty stomach with no more than 120 mL of water, followed by a 30-minute wait before eating or taking other medications to ensure proper absorption.
- Treatment options if control worsens include dose escalation to 14 mg daily, adding SGLT2 inhibitors or other agents, or switching to injectable GLP-1 agonists or insulin therapy.
- Regular HbA1c monitoring every three to six months and prompt contact with your diabetes care team enable timely treatment adjustment in line with NICE guidance.
Table of Contents
How Rybelsus Works for Type 2 Diabetes
Rybelsus (semaglutide) is an oral glucagon-like peptide-1 receptor agonist (GLP-1 RA) licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It is the first GLP-1 receptor agonist available in tablet form, offering an alternative to injectable formulations. Rybelsus is typically prescribed when diet and exercise alone, or in combination with other glucose-lowering medicines such as metformin, have not achieved adequate glycaemic control.
The mechanism of action of Rybelsus centres on mimicking the effects of the naturally occurring incretin hormone GLP-1. When blood glucose levels rise after eating, Rybelsus stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner. This means insulin release occurs primarily when blood sugar is elevated, reducing the risk of hypoglycaemia when used as monotherapy (though this risk increases when combined with insulin or sulfonylureas). Concurrently, semaglutide suppresses the release of glucagon—a hormone that raises blood glucose—thereby preventing excessive glucose production by the liver.
Beyond its effects on insulin and glucagon, Rybelsus also slows gastric emptying, which moderates the rate at which glucose enters the bloodstream after meals. Many patients experience reduced appetite and modest weight loss, which can further improve insulin sensitivity and overall metabolic control. According to NICE guidance (NG28), GLP-1 receptor agonists like Rybelsus are recommended as part of a comprehensive treatment strategy that includes lifestyle modification. For patients with established cardiovascular or kidney disease, SGLT2 inhibitors are often prioritised, but Rybelsus may be used in dual or triple therapy regimens depending on individual patient needs and HbA1c targets.
Rybelsus treatment begins with a 3 mg daily dose for 30 days, then increases to 7 mg daily. After at least another 30 days, the dose may be increased to 14 mg daily if needed for glycaemic control. It is important to note that Rybelsus is not indicated for type 1 diabetes or diabetic ketoacidosis.
Signs That Rybelsus Isn't Working as Well
Recognising when Rybelsus may not be providing adequate glycaemic control is essential for timely intervention and treatment adjustment. The most reliable indicator is a rising HbA1c level on routine blood tests. HbA1c reflects average blood glucose over the preceding two to three months, and an upward trend—or failure to reach individualised targets—suggests that current therapy may be insufficient. Your GP or diabetes specialist nurse will typically monitor HbA1c every three to six months to assess treatment efficacy, in line with NICE recommendations.
Home blood glucose monitoring can also reveal patterns of poor control, particularly for those on insulin, at risk of hypoglycaemia, or during treatment adjustments. If you monitor your glucose and notice consistently elevated fasting readings (typically above 7 mmol/L) or post-meal values that remain high (above 8.5–9 mmol/L two hours after eating), this may indicate diminished drug effectiveness. These targets are individualised based on your specific circumstances and should be discussed with your healthcare team. Some patients report a return of symptoms they experienced before starting treatment, such as increased thirst (polydipsia), frequent urination (polyuria), unexplained fatigue, or blurred vision. These classic hyperglycaemic symptoms warrant prompt medical review.
It is important to distinguish between true treatment failure and suboptimal adherence. Rybelsus must be taken on an empty stomach with no more than 120 mL of water, and patients must wait at least 30 minutes before eating, drinking, or taking other oral medications. Failure to follow these specific instructions can significantly impair absorption and reduce efficacy. Additionally, weight gain, increased carbohydrate intake, intercurrent illness, or the introduction of medications that raise blood glucose (such as corticosteroids) can all contribute to apparent loss of glycaemic control.
Seek urgent same-day medical advice if you experience persistent blood glucose readings above 20 mmol/L, positive ketones in urine or blood, vomiting, drowsiness, or signs of dehydration. These could indicate severe hyperglycaemia requiring immediate attention. If you suspect Rybelsus is not working as well, do not stop the medication abruptly—contact your healthcare team for assessment and guidance.
What to Do If Rybelsus Stops Controlling Your Blood Sugar
If you notice signs of worsening blood glucose control while taking Rybelsus, the first step is to contact your GP or diabetes care team promptly. Do not attempt to adjust your dose independently or discontinue treatment without medical advice. Your healthcare professional will arrange blood tests, including HbA1c and possibly fasting glucose, to objectively assess your current glycaemic status and determine whether treatment modification is necessary.
During your consultation, your clinician will conduct a thorough medication review to ensure you are taking Rybelsus correctly. They will confirm that you are adhering to the specific administration requirements—taking the tablet on an empty stomach first thing in the morning with a small amount of water (no more than 120 mL), then waiting at least 30 minutes before consuming food or other medications. If you miss a dose, the advice is to skip that dose and take your next scheduled dose the following day. Even minor deviations from these instructions can substantially reduce drug absorption. Your doctor will also review other medications you may be taking, as certain drugs can interfere with glucose control or interact with Rybelsus.
Lifestyle factors will be reassessed as part of this evaluation. Changes in diet, physical activity levels, body weight, or stress can all influence diabetes control. Your healthcare team may refer you to a diabetes specialist nurse or dietitian for additional support with meal planning, carbohydrate counting, and exercise recommendations. If adherence and lifestyle factors are optimised but glycaemic control remains inadequate, your doctor will consider treatment intensification in line with NICE guidelines.
Options may include increasing the Rybelsus dose (if you are not already on the maximum 14 mg daily), adding another oral glucose-lowering agent such as an SGLT2 inhibitor (particularly beneficial for those with cardiovascular or kidney disease), or switching to an injectable GLP-1 receptor agonist or insulin therapy. If insulin or a sulfonylurea is added, careful monitoring will be needed as the risk of hypoglycaemia increases with these combinations. The choice depends on your individual circumstances, HbA1c level, presence of complications, and personal preferences. Regular follow-up appointments will be scheduled to monitor your response to any treatment changes and ensure your diabetes remains well controlled.
Does Rybelsus Stop Working Over Time?
A common concern among patients is whether Rybelsus, like some other diabetes medications, loses effectiveness over time—a phenomenon sometimes referred to as secondary treatment failure. It is important to understand that type 2 diabetes is a progressive condition characterised by gradual decline in pancreatic beta-cell function and worsening insulin resistance. This natural disease progression means that many patients will eventually require treatment intensification, regardless of which medication they are taking. This does not necessarily indicate that Rybelsus has "stopped working," but rather that the underlying condition has advanced.
Clinical trial data from the PIONEER studies and regulatory assessments suggest that GLP-1 receptor agonists generally maintain their glucose-lowering efficacy over extended periods when used appropriately. While the gastric emptying effects may attenuate somewhat over time, the glycaemic benefits typically persist. However, individual responses vary, and some patients may experience a gradual reduction in treatment effect over months or years. Factors contributing to apparent loss of efficacy include progressive beta-cell dysfunction, weight gain, reduced physical activity, dietary changes, development of other medical conditions, or introduction of medications that raise blood glucose (such as corticosteroids or certain antipsychotics).
There is no evidence of pharmacological tachyphylaxis (diminishing response to repeated drug administration) specifically associated with Rybelsus—the drug's mechanism of action does not inherently diminish with continued use. If glycaemic control deteriorates, a comprehensive assessment is needed to identify the underlying cause. This may reveal modifiable factors such as suboptimal adherence, lifestyle changes, or concurrent illness, rather than true drug failure.
Regular monitoring through HbA1c testing and clinical review allows early detection of deteriorating control, enabling timely treatment adjustment. NICE recommends individualised HbA1c targets and a stepwise approach to therapy intensification. If Rybelsus alone becomes insufficient, combination therapy or alternative treatments can be introduced to maintain optimal glucose control and reduce the risk of long-term complications. Open communication with your diabetes care team ensures that your treatment plan evolves appropriately as your condition changes over time.
If you experience side effects while taking Rybelsus, such as nausea, vomiting, diarrhoea, or severe abdominal pain (which could indicate pancreatitis, a rare but serious adverse effect), report these to your healthcare provider and consider reporting suspected side effects via the MHRA Yellow Card Scheme.
Frequently Asked Questions
How do I know if Rybelsus has stopped working for my diabetes?
The most reliable indicator is a rising HbA1c level on routine blood tests, or consistently elevated fasting and post-meal glucose readings at home. Return of symptoms such as increased thirst, frequent urination, or unexplained fatigue may also suggest worsening glycaemic control and warrants prompt review by your GP or diabetes care team.
Can Rybelsus lose effectiveness over time?
There is no evidence that Rybelsus develops pharmacological tolerance or tachyphylaxis. However, type 2 diabetes is a progressive condition, and many patients eventually require treatment intensification due to declining beta-cell function and worsening insulin resistance, rather than true drug failure.
What should I do if my blood sugar rises whilst taking Rybelsus?
Contact your GP or diabetes care team promptly for assessment. Do not stop Rybelsus or adjust your dose independently. Your healthcare professional will review your adherence, lifestyle factors, and HbA1c, then consider dose escalation, adding another medication, or switching therapy if needed.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript