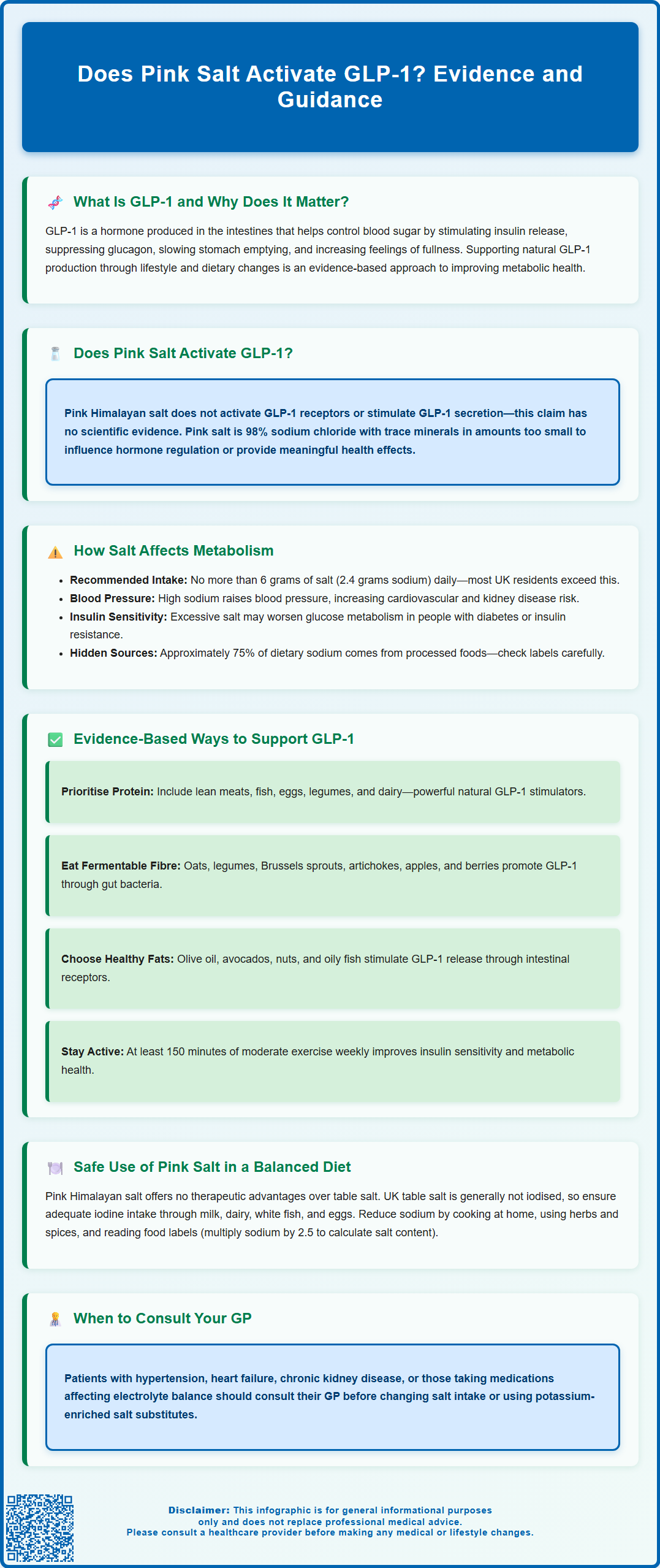
Claims that pink Himalayan salt can activate GLP-1 (glucagon-like peptide-1) have circulated widely on social media and wellness platforms, prompting questions from patients seeking natural approaches to metabolic health. GLP-1 is a crucial incretin hormone that regulates blood glucose, promotes satiety, and has become a therapeutic target in managing type 2 diabetes and obesity. However, there is no scientific evidence that pink salt—or any form of salt—directly stimulates GLP-1 secretion or activates GLP-1 receptors. This article examines the physiological role of GLP-1, evaluates the claim regarding pink salt, and provides evidence-based guidance on supporting natural GLP-1 production through diet and lifestyle modifications aligned with UK clinical recommendations.
Summary: No, pink salt does not activate GLP-1 receptors or stimulate GLP-1 secretion—this claim lacks scientific evidence and physiological basis.
- GLP-1 is an incretin hormone that regulates blood glucose by stimulating insulin secretion, suppressing glucagon, and slowing gastric emptying.
- Pink salt is approximately 98% sodium chloride with trace minerals insufficient to influence hormone regulation or metabolic function.
- GLP-1 release is triggered by macronutrients (proteins, fats, certain carbohydrates) detected by intestinal L-cells, not by mineral salts.
- Evidence-based approaches to support natural GLP-1 include consuming protein-rich foods, fermentable fibre, and healthy fats as part of a balanced diet.
- All salt types, including pink salt, should be limited to no more than 6 grams daily as per UK guidance to reduce cardiovascular risk.
- Patients with hypertension, kidney disease, or taking certain medications should consult their GP before altering sodium intake or using salt substitutes.
Table of Contents
What Is GLP-1 and Why Does It Matter for Health?
The primary mechanism of action involves stimulating insulin secretion from pancreatic beta cells in a glucose-dependent manner. This means GLP-1 promotes insulin release only when blood glucose levels are elevated, thereby reducing the risk of hypoglycaemia. Simultaneously, GLP-1 suppresses glucagon secretion from pancreatic alpha cells, which helps prevent excessive glucose production by the liver. Beyond glycaemic control, GLP-1 slows gastric emptying, which moderates the rate at which nutrients enter the bloodstream and contributes to feelings of satiety.
The clinical significance of GLP-1 has become increasingly apparent in recent years, particularly in the management of type 2 diabetes and obesity. GLP-1 receptor agonists (such as semaglutide and liraglutide) are now established treatments recommended by NICE for specific patient groups with type 2 diabetes (NICE NG28) and for managing obesity in people meeting certain criteria. These medications mimic the action of natural GLP-1 but are resistant to enzymatic degradation, providing sustained therapeutic effects. Understanding how to support natural GLP-1 production through lifestyle and dietary measures has therefore become an area of considerable interest for both healthcare professionals and patients seeking to optimise metabolic health through evidence-based approaches.
Does Pink Salt Activate GLP-1 Receptors?
Pink Himalayan salt has gained popularity as a purportedly healthier alternative to standard table salt, with various health claims circulating on social media and wellness platforms. However, there is no scientific evidence that pink salt directly activates GLP-1 receptors or stimulates GLP-1 secretion. This claim lacks any physiological basis and is not supported by peer-reviewed research.
Pink salt is primarily composed of sodium chloride (approximately 98%), with trace amounts of minerals such as potassium, magnesium, calcium, and iron that give it its characteristic colour. Whilst these minerals may contribute marginally to overall micronutrient intake, the quantities present are insufficient to produce meaningful physiological effects, particularly regarding hormone regulation. The mechanism by which GLP-1 is released involves specific nutrient sensors in intestinal L-cells that respond to macronutrients—particularly proteins, fats, and certain carbohydrates—not mineral salts.
From a clinical perspective, it is important to address such claims with patients who may be seeking alternative approaches to metabolic health. No form of salt, whether pink, sea, or table salt, has been demonstrated to influence GLP-1 activity. Patients interested in supporting their metabolic health should be directed towards evidence-based dietary patterns rather than relying on unsubstantiated claims about specific food products. Healthcare professionals should emphasise that whilst pink salt may be used as a culinary preference, it offers no therapeutic advantage over standard salt and should not be considered a metabolic intervention. The focus should remain on overall dietary quality, appropriate macronutrient balance, and adherence to established nutritional guidelines.
How Salt Intake Affects Metabolism and Hormone Function
Whilst salt does not directly activate GLP-1, excessive sodium intake does have significant implications for metabolic health and cardiovascular function. The UK Scientific Advisory Committee on Nutrition (SACN) recommends that adults consume no more than 6 grams of salt (approximately 2.4 grams of sodium) per day. Current UK population data indicates that average consumption exceeds this recommendation, with potential consequences for blood pressure regulation and cardiovascular risk.
High sodium intake is associated with increased blood pressure through multiple mechanisms, including enhanced fluid retention, increased vascular resistance, and altered endothelial function. Hypertension is a major risk factor for cardiovascular disease, stroke, and chronic kidney disease—conditions that frequently coexist with metabolic disorders such as type 2 diabetes. The relationship between salt intake and metabolic health is therefore indirect but clinically significant, particularly in populations with insulin resistance or established diabetes.
Some research suggests that high sodium intake may influence insulin sensitivity and glucose metabolism, although the evidence is limited and the mechanisms remain incompletely understood. Some studies indicate that high sodium intake may affect insulin signalling pathways and contribute to oxidative stress, potentially exacerbating metabolic dysfunction. However, these effects are related to overall sodium burden rather than the specific type of salt consumed.
From a practical standpoint, patients should be advised to:
-
Monitor total salt intake from all sources, including processed foods, which contribute approximately 75% of dietary sodium in the UK
-
Read food labels carefully, noting that UK food labels typically show salt content; if sodium is listed, multiply by 2.5 to calculate salt equivalent
-
Use herbs and spices as flavour alternatives to reduce reliance on salt
-
Be aware that pink salt contains the same sodium content as table salt and should be used with the same caution
Patients with hypertension, cardiovascular disease, or chronic kidney disease may require more stringent sodium restriction as advised by their healthcare team.
Evidence-Based Ways to Support Natural GLP-1 Production
Supporting endogenous GLP-1 secretion requires a comprehensive approach centred on dietary composition, meal timing, and lifestyle factors. Protein-rich foods are among the most potent stimulators of GLP-1 release, with studies demonstrating that protein intake triggers substantial incretin responses. High-quality protein sources such as lean meats, fish, eggs, legumes, and dairy products should be incorporated into meals to optimise postprandial GLP-1 secretion.
Dietary fibre, particularly soluble and fermentable fibres, plays a crucial role in GLP-1 regulation. These fibres are metabolised by gut microbiota to produce short-chain fatty acids (SCFAs), including butyrate, propionate, and acetate, which directly stimulate L-cells to release GLP-1. Foods rich in fermentable fibre include:
-
Oats, barley, and whole grains
-
Legumes such as lentils, chickpeas, and beans
-
Vegetables including artichokes, Brussels sprouts, and onions
-
Fruits such as apples, pears, and berries
Healthy fats, particularly long-chain fatty acids, also stimulate GLP-1 secretion through specific receptors on intestinal L-cells. Sources such as olive oil, avocados, nuts, and oily fish (rich in omega-3 fatty acids) should be included as part of a balanced dietary pattern.
Meal timing and composition may influence GLP-1 responses, though individual variation exists. Consuming protein and fibre early in meals may enhance satiety signals and improve glycaemic control. Some preliminary evidence suggests that eating patterns that avoid prolonged fasting followed by large meals may support more consistent incretin responses.
Physical activity represents another evidence-based approach to metabolic health. Regular exercise improves insulin sensitivity and may enhance incretin responses, although the direct effects on GLP-1 are complex and influenced by exercise intensity, duration, and individual metabolic status. The UK Chief Medical Officers' Physical Activity Guidelines recommend at least 150 minutes of moderate-intensity aerobic activity weekly for adults, which supports overall metabolic health.
Patients should be advised that these dietary and lifestyle approaches work synergistically and are most effective when implemented as part of a comprehensive, sustainable pattern rather than isolated interventions.
Safe Use of Pink Salt in a Balanced UK Diet
Pink Himalayan salt can be incorporated into a balanced UK diet as a culinary ingredient, but it should not be considered therapeutically superior to standard table salt. The key principle is moderation of total sodium intake, regardless of salt type. Patients often perceive pink salt as healthier due to marketing claims about mineral content, but the trace minerals present do not provide clinically meaningful nutritional benefits when consumed in the small quantities typical of salt use.
One consideration when choosing salt types is iodine content. Unlike some countries, most table salt in the UK is not iodised. Iodine is an essential micronutrient required for thyroid hormone synthesis. Pink salt does not contain iodine, and exclusive use of non-iodised salts may contribute to inadequate iodine intake if dietary sources are limited. The main UK dietary sources of iodine include milk and dairy products, white fish, and eggs. Pregnant women and those planning pregnancy should be particularly mindful of iodine intake, as deficiency can affect foetal neurodevelopment. Standard prenatal supplements containing iodine may be appropriate for those with insufficient dietary intake. Seaweed or kelp supplements should be avoided due to variable and potentially excessive iodine content.
For patients seeking to reduce sodium intake whilst maintaining flavour in cooking, evidence-based strategies include:
-
Gradual reduction in salt use, allowing taste preferences to adapt over time
-
Potassium-enriched salt substitutes (under medical supervision for those with kidney disease or taking certain medications)
-
Fresh herbs, spices, lemon juice, and vinegar as flavour enhancers
-
Home cooking to control sodium content, as processed and restaurant foods are major sodium sources
When to seek medical advice: Patients with hypertension, heart failure, chronic kidney disease, or those taking medications that affect electrolyte balance (such as ACE inhibitors, angiotensin receptor blockers, diuretics, or potassium-sparing medications including spironolactone) should consult their GP or specialist before making significant changes to salt intake or using salt substitutes. These individuals may require tailored sodium and potassium recommendations based on their specific clinical circumstances.
In summary, pink salt may be used as a personal preference in cooking, but it offers no metabolic advantages and should be consumed within recommended sodium limits. Healthcare professionals should emphasise that sustainable metabolic health depends on overall dietary quality, appropriate macronutrient balance, regular physical activity, and adherence to evidence-based guidelines rather than reliance on individual food products with unsubstantiated health claims.
Frequently Asked Questions
Can pink Himalayan salt help with blood sugar control by activating GLP-1?
No, pink salt does not activate GLP-1 or influence blood sugar control. GLP-1 is released in response to macronutrients such as proteins and fats, not mineral salts, and no scientific evidence supports this claim.
What are proven ways to naturally increase GLP-1 levels?
Evidence-based strategies include consuming protein-rich foods, fermentable fibre (such as oats, legumes, and vegetables), and healthy fats (olive oil, nuts, oily fish). Regular physical activity and balanced meal composition also support metabolic health and incretin responses.
Is pink salt healthier than regular table salt?
No, pink salt offers no health advantages over table salt. Both contain approximately the same sodium content, and the trace minerals in pink salt are insufficient to provide meaningful nutritional benefits. All salt types should be limited to 6 grams daily as per UK guidance.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript