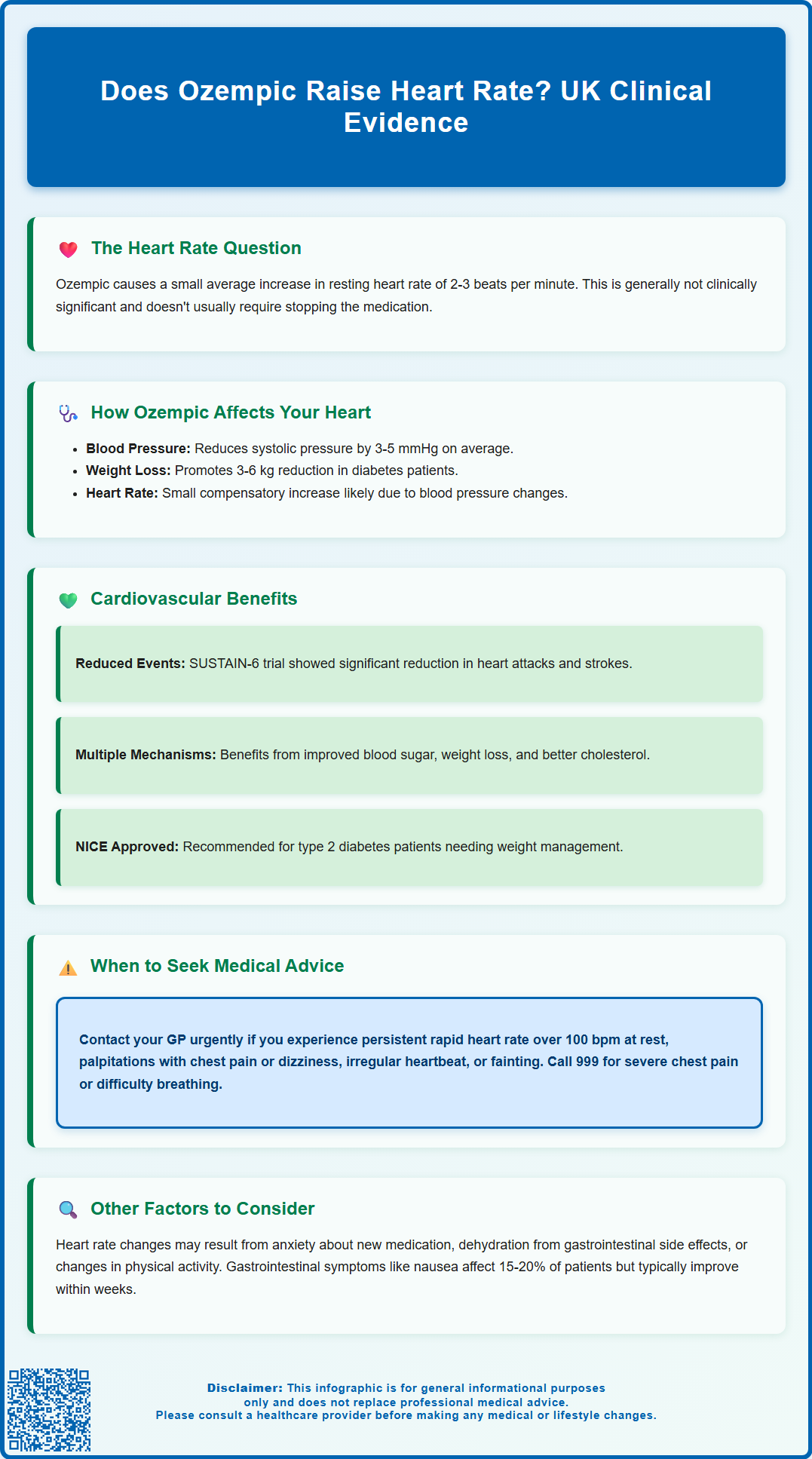
Does Ozempic raise heart rate? This is a common question among patients prescribed semaglutide for type 2 diabetes. Clinical evidence shows that Ozempic (semaglutide), a GLP-1 receptor agonist, is associated with a small increase in resting heart rate—typically 2–3 beats per minute on average. This modest change is generally not clinically significant for most patients. Despite this minor effect, large-scale trials such as SUSTAIN-6 have demonstrated cardiovascular benefits in people with type 2 diabetes at high cardiovascular risk. Understanding how Ozempic affects heart rate and overall cardiovascular function is essential for informed treatment decisions.
Summary: Ozempic is associated with a small increase in resting heart rate of approximately 2–3 beats per minute on average, which is generally not clinically significant.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus treatment.
- The small heart rate increase is documented in the Summary of Product Characteristics and does not usually require treatment modification.
- Large-scale trials including SUSTAIN-6 have demonstrated cardiovascular benefits and reduced major adverse cardiovascular events in high-risk patients.
- The mechanism behind the heart rate effect is not fully understood but may relate to autonomic nervous system changes.
- Patients experiencing persistent palpitations, chest pain, or irregular heartbeat should contact their GP for cardiovascular assessment.
- MHRA and EMA have reviewed extensive safety data confirming the cardiovascular profile of semaglutide.
Table of Contents
Does Ozempic Raise Heart Rate?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Many patients and healthcare professionals have questioned whether this medication can affect heart rate.
Clinical evidence shows that Ozempic is associated with a small increase in resting heart rate — typically in the range of 2-3 beats per minute on average, as documented in the Summary of Product Characteristics. This modest increase is generally not considered clinically significant for most patients and does not usually require treatment modification.
Despite this small heart rate effect, large-scale cardiovascular outcome trials, including the SUSTAIN-6 study, have demonstrated that semaglutide is associated with cardiovascular benefits in people with type 2 diabetes at high cardiovascular risk. The Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) have reviewed extensive safety data on semaglutide.
The mechanism behind this minor heart rate effect is not fully understood but may potentially relate to autonomic nervous system changes or other physiological adaptations. It's important to note that this is distinct from Wegovy (semaglutide), which is the licensed brand for weight management in the UK.
It is important to distinguish between medication effects and other factors that might influence heart rate, such as anxiety about starting a new medication, concurrent illness, dehydration (which can occur with gastrointestinal side effects), or changes in physical activity levels. If you notice palpitations or a persistently elevated heart rate after starting Ozempic, this warrants discussion with your GP or diabetes specialist to rule out other causes and ensure appropriate monitoring.
Common Side Effects of Ozempic on Heart Function
Whilst Ozempic is associated with a small mean increase in heart rate, understanding its broader cardiovascular side effect profile is essential for both patients and clinicians. The most frequently reported adverse effects relate to the gastrointestinal system rather than direct cardiac effects, including nausea (occurring in approximately 15-20% of patients according to the SmPC), vomiting, diarrhoea, and constipation. These symptoms are usually mild to moderate and tend to diminish over the first few weeks of treatment.
From a cardiovascular perspective, Ozempic has demonstrated protective effects in clinical trials. The SUSTAIN-6 trial showed a significant reduction in major adverse cardiovascular events (MACE), including non-fatal myocardial infarction and non-fatal stroke, specifically in patients with type 2 diabetes and established cardiovascular disease or multiple cardiovascular risk factors. This cardioprotective benefit is thought to result from multiple mechanisms, including improved glycaemic control, weight reduction, blood pressure lowering, and favourable effects on lipid profiles.
Small reductions in blood pressure are typically observed with Ozempic treatment. While symptomatic low blood pressure is not listed as a common adverse reaction in the SmPC, it may occur in some patients, particularly those taking concurrent antihypertensive medications or diuretics, or those experiencing dehydration due to gastrointestinal side effects.
Some patients report experiencing palpitations — an awareness of their heartbeat that may feel rapid, strong, or irregular. While arrhythmias are not listed as adverse reactions in the SmPC, palpitations should always be evaluated to exclude other cardiac conditions. It is worth noting that weight loss itself, which commonly occurs with Ozempic treatment, can lead to changes in cardiovascular parameters and may contribute to the sensation of palpitations in some individuals.
When to Seek Medical Advice About Heart Rate Changes
Whilst most patients tolerate Ozempic well without significant cardiovascular concerns, certain symptoms warrant prompt medical evaluation. You should contact your GP or healthcare professional urgently if you experience any of the following:
-
Persistent rapid heart rate (tachycardia) at rest, particularly if your resting heart rate exceeds 100 beats per minute consistently
-
Palpitations accompanied by chest pain, shortness of breath, or dizziness, which could indicate a more serious cardiac condition
-
Irregular heartbeat or sensation of skipped beats, especially if this is new or persistent
-
Syncope (fainting) or pre-syncope (feeling like you might faint), which may suggest significant hypotension or cardiac arrhythmia
-
Chest discomfort or pressure, particularly if associated with exertion, sweating, or radiation to the arm or jaw
Seek immediate emergency care (call 999) if you experience severe chest pain, difficulty breathing, or symptoms suggestive of a heart attack or stroke.
If you have urgent concerns but cannot reach your GP, contact NHS 111 for advice. For less urgent concerns, such as mild, intermittent palpitations without other symptoms, schedule a routine appointment with your GP. They can perform a thorough cardiovascular assessment, including blood pressure measurement, heart rate monitoring, and potentially an electrocardiogram (ECG) to evaluate your heart rhythm. Your doctor may also review your other medications, as drug interactions or the cumulative effect of multiple cardiovascular medications may contribute to symptoms.
It is particularly important to report heart rate changes if you have pre-existing cardiovascular disease, a history of arrhythmias, or other significant cardiac risk factors. Patients with these conditions require closer monitoring when initiating or adjusting doses of Ozempic. NICE guidance emphasises the importance of individualised risk assessment and regular review for patients with type 2 diabetes, particularly those with established cardiovascular disease.
How Ozempic Affects Your Cardiovascular System
Understanding the mechanism of action of Ozempic helps explain its cardiovascular effects. Semaglutide is a long-acting GLP-1 receptor agonist that mimics the action of the naturally occurring incretin hormone GLP-1. It works primarily by enhancing glucose-dependent insulin secretion, suppressing inappropriate glucagon release, slowing gastric emptying, and reducing appetite through central nervous system effects.
From a cardiovascular perspective, Ozempic has several effects. Clinical trials have demonstrated small mean reductions in systolic blood pressure (typically 3-5 mmHg), which may contribute to overall cardiovascular risk reduction. The medication also promotes weight loss — typically 3-6 kg in patients with type 2 diabetes at the doses used for diabetes treatment — which itself may confer cardiovascular benefits through reduced cardiac workload and improved metabolic parameters.
GLP-1 receptors are present in various cardiovascular tissues, including the heart, blood vessels, and autonomic nervous system. Some research suggests that activation of these receptors may potentially have cardioprotective effects. Preclinical studies have explored possible mechanisms including improved endothelial function, reduced inflammation, and potential anti-atherosclerotic properties, though these effects require further investigation in humans before definitive conclusions can be drawn.
The small increase in heart rate observed with semaglutide (approximately 2-3 beats per minute on average) is documented in the SmPC. The exact mechanism for this is not fully established, but hypotheses include compensatory responses to blood pressure reduction or direct effects on autonomic tone.
NICE guidance (NG28) recommends GLP-1 receptor agonists like Ozempic as part of a treatment strategy for type 2 diabetes, particularly in patients who would benefit from weight loss. For patients with established cardiovascular disease, SGLT2 inhibitors with proven cardiovascular benefit are often considered first-line, with GLP-1 receptor agonists as an alternative option. Regular monitoring of cardiovascular parameters, including blood pressure and heart rate, forms part of routine diabetes care. Patients should continue with lifestyle modifications, including a balanced diet and regular physical activity, to maximise cardiovascular health alongside pharmacological treatment.
If you experience any side effects while taking Ozempic, you can report them directly to the MHRA through the Yellow Card Scheme at yellowcard.mhra.gov.uk.
Frequently Asked Questions
Is the heart rate increase from Ozempic dangerous?
The small increase in heart rate (2–3 beats per minute on average) associated with Ozempic is generally not clinically significant for most patients and does not usually require treatment modification. Large-scale trials have demonstrated overall cardiovascular benefits.
What cardiovascular side effects should I watch for on Ozempic?
Contact your GP urgently if you experience persistent rapid heart rate at rest, palpitations with chest pain or breathlessness, irregular heartbeat, fainting, or chest discomfort. Call 999 for severe chest pain or difficulty breathing.
Does Ozempic have cardiovascular benefits?
Yes, the SUSTAIN-6 trial showed that Ozempic significantly reduced major adverse cardiovascular events, including non-fatal heart attack and stroke, in patients with type 2 diabetes and established cardiovascular disease or multiple risk factors.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












