Many patients taking Ozempic (semaglutide) notice changes in their urine colour and wonder whether the medication is responsible. Whilst Ozempic does not directly cause yellow urine as a documented side effect, the medication's impact on appetite, fluid intake, and gastrointestinal function can indirectly affect hydration status—the primary determinant of urine colour. Yellow urine typically reflects normal physiology, with colour intensity indicating how concentrated your urine is. Understanding the relationship between Ozempic's common side effects and hydration can help you distinguish between benign changes and those requiring medical attention. This article examines why urine colour changes occur, how Ozempic may indirectly influence urine appearance, and when to seek professional advice.
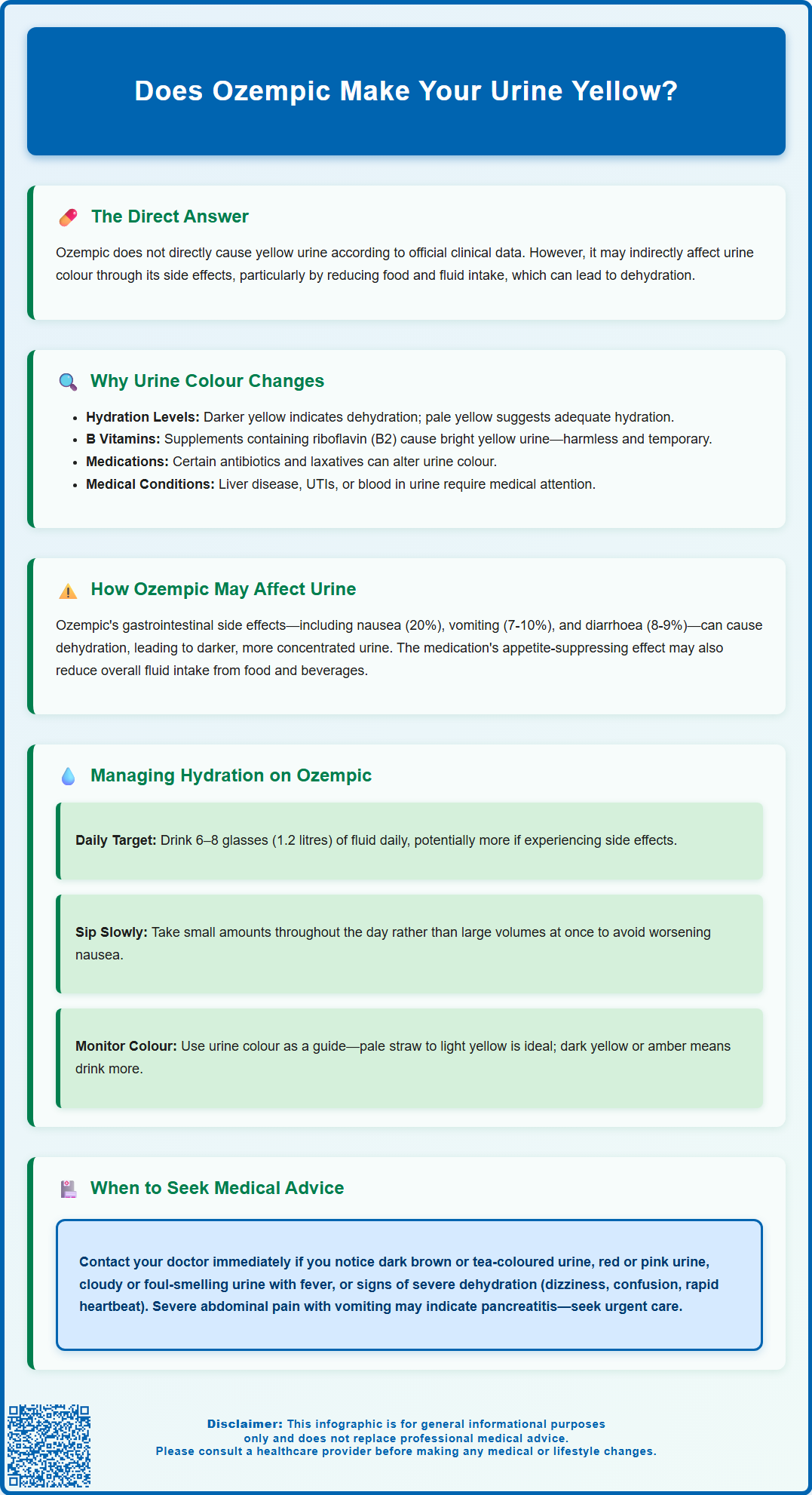
Summary: Ozempic does not directly cause yellow urine, but its gastrointestinal side effects may lead to dehydration, which can make urine appear darker yellow.
- Semaglutide (Ozempic) is a GLP-1 receptor agonist licensed for type 2 diabetes treatment that works by enhancing insulin secretion, suppressing glucagon, and slowing gastric emptying.
- Common gastrointestinal side effects including nausea, vomiting, and diarrhoea can reduce fluid intake and increase fluid losses, leading to dehydration and darker urine.
- Yellow urine colour primarily reflects hydration status and urochrome pigment concentration—darker yellow indicates more concentrated, dehydrated urine.
- Seek urgent medical attention for dark brown, red, or cola-coloured urine, or if experiencing severe dehydration symptoms alongside persistent gastrointestinal side effects.
- Maintaining adequate hydration (6–8 glasses daily) through regular fluid intake is essential when taking Ozempic, particularly during dose initiation or escalation.
Table of Contents
Does Ozempic Make Your Urine Yellow?
Ozempic (semaglutide) is not directly known to cause yellow urine as a documented side effect. There is no official link established in the Summary of Product Characteristics (SmPC) or clinical trial data indicating that semaglutide itself alters urine colour to yellow. However, patients taking Ozempic may notice changes in their urine appearance for reasons indirectly related to the medication's effects on the body.
Yellow urine is typically a normal physiological occurrence and most commonly reflects your hydration status. The colour of urine ranges from pale straw to deep amber, depending primarily on the concentration of urochrome (a pigment produced from the breakdown of haemoglobin) and your fluid intake. When you are well-hydrated, urine appears lighter; when dehydrated, it becomes more concentrated and darker yellow.
The connection between Ozempic and urine colour changes is more likely indirect, stemming from the medication's gastrointestinal side effects rather than a direct pharmacological action. Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes. It works by enhancing insulin secretion, suppressing glucagon release, slowing gastric emptying, and reducing appetite. These mechanisms can lead to reduced food and fluid intake, as well as gastrointestinal symptoms that may affect hydration status.
If you notice persistently dark or unusually coloured urine whilst taking Ozempic, it is important to consider other factors such as hydration levels, dietary changes, other medications, or underlying health conditions. Whilst yellow urine alone is rarely concerning, significant changes in urine colour warrant attention and may require medical assessment to rule out other causes.
Why Urine Colour Changes Occur
Urine colour is primarily determined by concentration and the presence of various substances filtered by the kidneys. Normal urine contains water, urea, electrolytes, and urochrome pigments. The intensity of yellow colouration directly correlates with urine concentration—the less water present, the more concentrated the pigments become, resulting in darker yellow or amber urine.
Several physiological and pathological factors influence urine colour:
-
Hydration status: Dehydration is the most common cause of dark yellow urine. When fluid intake is insufficient or fluid losses are excessive (through sweating, vomiting, or diarrhoea), the kidneys conserve water by producing more concentrated urine.
-
Dietary factors: Certain foods and beverages can temporarily alter urine colour. B vitamins, particularly riboflavin (vitamin B2), commonly cause bright yellow urine. Beetroot, blackberries, and rhubarb can produce reddish tones.
-
Medications and supplements: Many medications affect urine colour. Multivitamins, particularly those high in B vitamins, frequently cause bright yellow urine. Antibiotics such as nitrofurantoin can produce brown urine, whilst some laxatives containing senna may cause reddish-brown discolouration.
-
Medical conditions: Liver disease can cause dark brown or tea-coloured urine due to excess bilirubin. Urinary tract infections may produce cloudy or foul-smelling urine. Haematuria (blood in urine) can range from pink to red or brown, depending on the amount and whether the blood is fresh or oxidised.
Understanding these factors helps distinguish between benign changes and those requiring medical investigation. When taking medications like Ozempic, it is particularly important to consider how the drug's side effects—especially those affecting appetite, food intake, and gastrointestinal function—might indirectly influence hydration and, consequently, urine appearance.
Common Side Effects of Ozempic That May Affect Urine
Ozempic's most frequent side effects involve the gastrointestinal system, and these can indirectly impact urine colour through effects on hydration status. The medication's mechanism of slowing gastric emptying and reducing appetite commonly leads to gastrointestinal symptoms, particularly during dose initiation and escalation.
Gastrointestinal side effects and fluid balance:
-
Nausea: Very common, affecting approximately 20% of patients. This can reduce fluid intake, leading to dehydration and consequently darker, more concentrated urine.
-
Vomiting: Common, affecting approximately 7-10% of patients. This can cause fluid losses, contributing to dehydration risk.
-
Diarrhoea: Common, occurring in approximately 8-9% of patients. Diarrhoea increases fluid losses through the gastrointestinal tract. If not adequately replaced, this can result in dehydration and darker yellow urine.
-
Reduced appetite and food intake: Ozempic's appetite-suppressing effects may lead to decreased overall fluid consumption, as people often obtain significant hydration from foods and beverages consumed with meals.
Other relevant considerations:
Ozempic improves glycaemic control in people with type 2 diabetes by lowering blood glucose levels. Better glucose control may actually reduce polyuria (excessive urination) that some people experience with poorly controlled diabetes. This change in urination patterns might make patients more aware of their urine's appearance.
The medication is not known to cause direct renal toxicity or to be nephrotoxic at therapeutic doses. However, as noted in the SmPC, there have been post-marketing reports of acute kidney injury in patients experiencing severe gastrointestinal side effects leading to dehydration. Maintaining adequate hydration is therefore essential for patients taking Ozempic, particularly during the initial weeks of treatment or following dose increases.
It is worth noting that if you are taking other medications alongside Ozempic—such as diuretics or vitamin supplements—these may also contribute to changes in urine colour or concentration.
When to Seek Medical Advice About Urine Changes
Whilst yellow urine is typically benign, certain changes warrant prompt medical assessment. Understanding when urine colour changes signal a potential problem is important for patient safety, particularly when taking medications that affect fluid balance.
Seek urgent medical attention if you experience:
-
Dark brown or tea-coloured urine: This may indicate liver dysfunction, severe dehydration, or rhabdomyolysis (muscle breakdown). If accompanied by jaundice (yellowing of skin or eyes), pale stools, or abdominal pain, contact your GP immediately or attend A&E.
-
Red, pink, or cola-coloured urine: Whilst sometimes caused by foods like beetroot, this can indicate haematuria (blood in urine). If you are 45 or older with unexplained visible haematuria, or if symptoms persist or recur after treatment, you should be urgently referred to a specialist to rule out cancer. Haematuria with pain, fever, or difficulty urinating may indicate a urinary tract infection, kidney stones, or other urological conditions requiring assessment.
-
Cloudy or foul-smelling urine with symptoms: Combined with fever, burning sensation during urination, increased frequency, or lower abdominal pain, this suggests a possible urinary tract infection requiring medical assessment and potentially antibiotic treatment.
-
Signs of severe dehydration: Including dark yellow urine alongside dizziness, confusion, rapid heartbeat, reduced urine output, or inability to keep fluids down due to persistent vomiting or diarrhoea.
-
Severe, persistent abdominal pain radiating to the back, especially with vomiting: This could indicate acute pancreatitis, a rare but serious side effect associated with GLP-1 receptor agonists like Ozempic that requires immediate medical attention.
Contact your GP or diabetes specialist nurse if:
-
Urine colour changes persist despite adequate hydration
-
You experience ongoing gastrointestinal side effects from Ozempic that affect your ability to maintain fluid intake
-
You notice any unexplained changes in urination patterns, such as significantly increased or decreased frequency
-
You have concerns about medication side effects or interactions
According to NICE guidance, patients starting GLP-1 receptor agonists like Ozempic should be monitored for tolerability, and dose adjustments or treatment discontinuation may be necessary if side effects are severe or persistent. If you suspect you're experiencing side effects from Ozempic, you can report these through the MHRA Yellow Card Scheme.
Managing Hydration While Taking Ozempic
Maintaining adequate hydration is essential for patients taking Ozempic, particularly given the medication's gastrointestinal side effects. Proper fluid management can help prevent dehydration-related complications and may reduce the intensity of some side effects.
Practical hydration strategies:
-
Aim for consistent fluid intake: The NHS Eatwell Guide recommends 6–8 glasses (approximately 1.2 litres) of fluid daily, though individual needs vary based on activity level, climate, and health status. When taking Ozempic, you may need to consciously increase intake if experiencing nausea or reduced appetite.
-
Monitor urine colour: Use your urine as a hydration indicator. Pale straw to light yellow suggests adequate hydration; dark yellow or amber indicates you need more fluids. This simple self-monitoring tool can help you adjust intake throughout the day.
-
Sip fluids regularly: Rather than drinking large volumes at once (which may worsen nausea), take small, frequent sips throughout the day. Keep water readily accessible.
-
Choose appropriate beverages: Water is ideal, but sugar-free squash, herbal teas, and clear broths also contribute to hydration. Tea and coffee count towards your fluid intake, though moderation is advised with caffeinated drinks and alcohol due to their mild diuretic effects.
Managing gastrointestinal side effects:
-
Eat smaller, more frequent meals: This approach, recommended for managing Ozempic-related nausea, also provides more opportunities to consume fluids with food.
-
Avoid triggers: Identify and avoid foods or smells that worsen nausea, as this can help maintain better overall intake.
-
Follow dosing instructions: Administer Ozempic as prescribed. The SmPC notes that it can be taken at any time of day, with or without food. If you're struggling with side effects, discuss timing options with your healthcare provider.
When to seek additional support:
If persistent side effects prevent adequate hydration despite these strategies, consult your healthcare team. They may recommend anti-emetic medications, temporary dose reduction, or slower dose escalation. In cases of severe dehydration with inability to tolerate oral fluids, intravenous rehydration may be necessary. Your diabetes specialist nurse or GP can provide personalised guidance to help you successfully manage treatment whilst maintaining optimal hydration status.
Frequently Asked Questions
Can Ozempic directly change the colour of my urine?
No, Ozempic (semaglutide) does not directly alter urine colour according to clinical trial data and the Summary of Product Characteristics. Any changes in urine appearance are typically indirect, resulting from the medication's gastrointestinal side effects that may affect hydration status.
Why might my urine be darker yellow whilst taking Ozempic?
Darker yellow urine whilst taking Ozempic usually indicates dehydration, which can occur due to the medication's common side effects such as nausea, vomiting, diarrhoea, or reduced appetite leading to decreased fluid intake. Maintaining adequate hydration by drinking 6–8 glasses of fluid daily can help prevent this.
When should I contact my doctor about urine colour changes on Ozempic?
Seek urgent medical attention if you notice dark brown, red, or cola-coloured urine, or if you experience signs of severe dehydration such as dizziness, confusion, or inability to keep fluids down. Contact your GP if urine colour changes persist despite adequate hydration or if you have ongoing gastrointestinal side effects affecting fluid intake.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












