Wegovy®
A weekly GLP-1 treatment proven to reduce hunger and support meaningful, long-term fat loss.
- ~16.9% average body weight loss
- Boosts metabolic & cardiovascular health
- Proven, long-established safety profile
- Weekly injection, easy to use

Many people starting Ozempic (semaglutide) wonder whether it will affect their bowel habits. As a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, Ozempic works by slowing gastric emptying and influencing gut motility, which can lead to changes in how often you need to use the bathroom. Gastrointestinal side effects—including diarrhoea, constipation, and altered bowel frequency—are amongst the most commonly reported reactions. Understanding how Ozempic affects your digestive system, what symptoms to expect, and when to seek medical advice can help you manage treatment more confidently and safely.
Summary: Ozempic commonly affects bowel habits, causing diarrhoea in more than 1 in 10 patients, though some experience constipation instead.
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by mimicking the action of naturally occurring GLP-1, a hormone released by the intestine in response to food intake. By binding to GLP-1 receptors throughout the body—including those in the pancreas, brain, and importantly, the gastrointestinal tract—Ozempic enhances insulin secretion, suppresses glucagon release, and slows gastric emptying.
This slowing of gastric emptying is central to understanding how Ozempic affects your digestive system. When food moves more slowly from your stomach into your small intestine, you feel fuller for longer, which helps reduce appetite. However, this mechanism also means that the normal transit of food and waste through your digestive tract can be altered, leading to various gastrointestinal symptoms.
The presence of GLP-1 receptors in the gut wall means that Ozempic directly influences intestinal motility and secretion. Some patients experience increased bowel frequency or looser stools, whilst others may notice constipation. These effects are particularly common during the initial weeks of treatment or following dose escalation, as your digestive system adapts to the medication's influence on gut function.
According to the MHRA/EMC Summary of Product Characteristics, gastrointestinal side effects are among the most frequently reported adverse reactions to Ozempic. Clinical trials have demonstrated that nausea, diarrhoea, vomiting, and constipation occur in a significant proportion of patients. While these symptoms often improve over time as tolerance develops, rarely more serious gastrointestinal complications can occur that require prompt medical assessment.
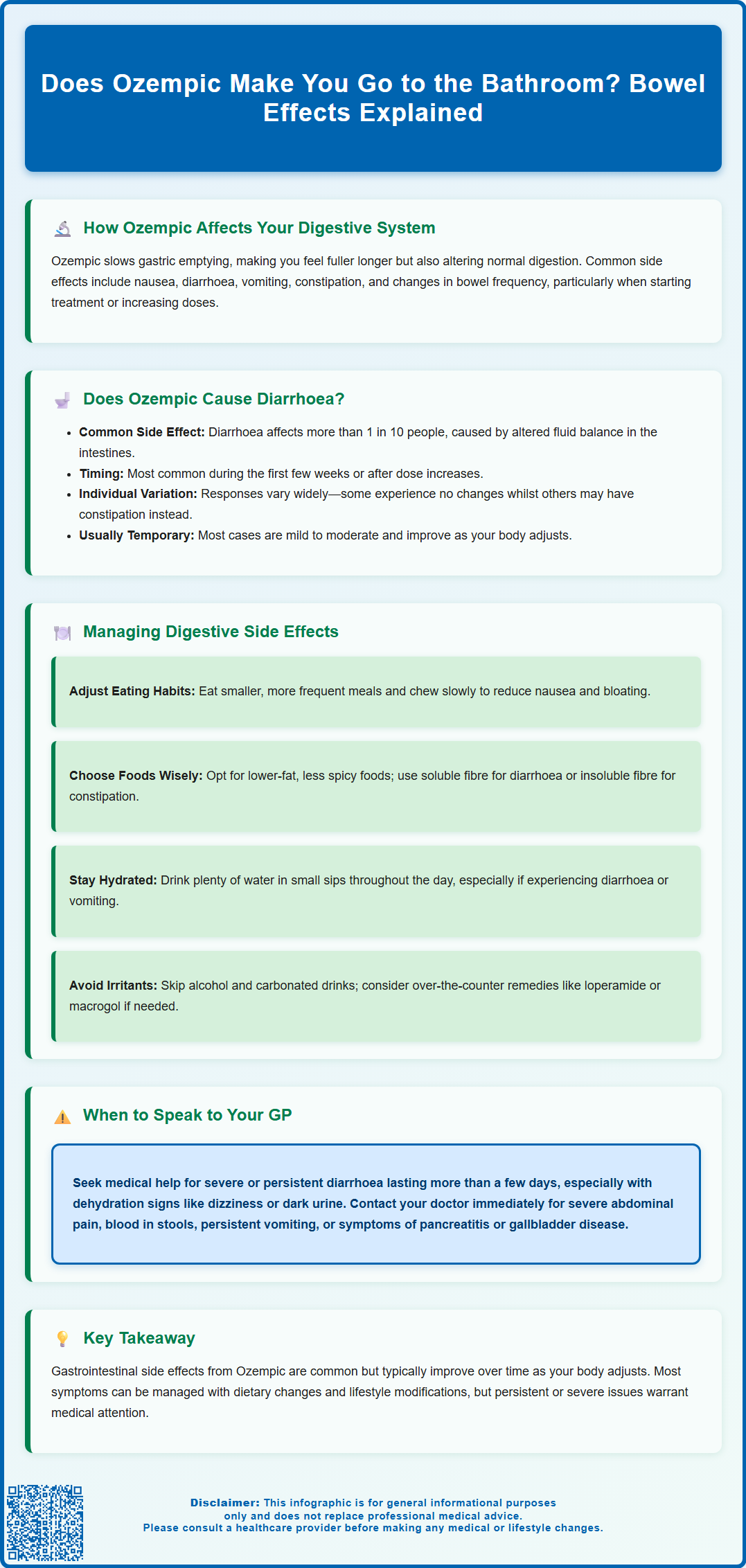
Diarrhoea is a very common side effect of Ozempic. According to the UK product information, diarrhoea occurs in more than 1 in 10 people taking semaglutide, making it one of the more frequent gastrointestinal adverse effects alongside nausea and vomiting. The mechanism behind this relates to the drug's effect on gut motility and fluid secretion within the intestines.
When Ozempic activates GLP-1 receptors in the gastrointestinal tract, it can alter the balance of fluid absorption and secretion, potentially leading to looser or more frequent stools. Some patients describe needing to use the bathroom more urgently or more often than usual, particularly in the first few weeks after starting treatment or increasing their dose. This is generally a transient effect that improves as your body adjusts to the medication.
It is worth noting that not everyone experiences diarrhoea on Ozempic—individual responses vary considerably. Some patients have no change in bowel habits, whilst others may actually experience constipation instead. The likelihood of developing diarrhoea appears to be dose-dependent, with higher doses potentially associated with more pronounced gastrointestinal effects, as observed in clinical trials.
If you do experience diarrhoea whilst taking Ozempic, it is typically mild to moderate in severity and self-limiting. However, persistent or severe diarrhoea warrants medical attention, as it can lead to dehydration, electrolyte imbalances and potentially acute kidney injury, especially in people with diabetes. Rarely, more serious gastrointestinal complications such as intestinal obstruction or gallbladder disease can occur. Any significant change in bowel habits should be discussed with your healthcare provider to ensure appropriate management.
Practical dietary and lifestyle modifications can significantly help manage digestive side effects whilst taking Ozempic. Starting with smaller, more frequent meals rather than large portions can reduce the burden on your already-slowed digestive system. Eating slowly and chewing food thoroughly allows your stomach to process meals more comfortably, potentially reducing nausea and bloating.
Dietary composition matters considerably. Foods high in fat can exacerbate nausea and delayed gastric emptying, so opting for lower-fat options may improve tolerance. Similarly, avoiding spicy, heavily seasoned, or very rich foods during the initial adjustment period can help. Adequate fibre intake is important—if you're experiencing diarrhoea, soluble fibre from sources like oats and bananas may help firm stools, whilst those with constipation may benefit from gradually increasing insoluble fibre alongside fluid intake.
Hydration is essential, particularly if you're experiencing diarrhoea or vomiting. Aim to drink plenty of water throughout the day, taking small, frequent sips if large amounts cause discomfort. Oral rehydration solutions may be beneficial if diarrhoea is persistent, helping to replace lost electrolytes.
Timing your Ozempic injection consistently on the same day each week is important, as recommended in the product information. Some patients find that injecting at a particular time of day helps them manage side effects better, though evidence for this is limited and based mainly on patient preference. Additionally, avoiding alcohol and carbonated beverages can reduce gastrointestinal irritation.
If you experience diarrhoea, your pharmacist may recommend short-term use of loperamide, while constipation might be managed with an osmotic laxative such as macrogol. If you take other diabetes medications, particularly insulin or sulfonylureas, monitor your blood glucose more frequently during episodes of significant gastrointestinal upset, as your absorption of food and medications may be affected.
If symptoms persist beyond the first few weeks or significantly impact your quality of life, your GP may consider adjusting your dose escalation schedule. Slower titration—staying at a lower dose for longer—can sometimes improve tolerability whilst still providing therapeutic benefit.
Whilst mild digestive changes are common with Ozempic, certain symptoms require prompt medical attention. You should contact your GP or healthcare provider if you experience severe or persistent diarrhoea lasting more than a few days, particularly if accompanied by signs of dehydration such as dizziness, reduced urination, dark urine, or excessive thirst. Dehydration can be serious and may require medical intervention.
Severe abdominal pain is another important warning sign. Whilst some mild cramping or discomfort can occur with bowel changes, intense, persistent, or worsening abdominal pain—especially if localised to the upper abdomen and radiating to the back—could indicate pancreatitis, a rare but serious potential side effect of GLP-1 receptor agonists. If pancreatitis is suspected, you should stop taking semaglutide immediately and seek urgent medical assessment.
You should also seek medical advice if you notice blood in your stools, black tarry stools, or persistent vomiting, as these symptoms may indicate gastrointestinal bleeding or other serious conditions that require investigation. Similarly, if you develop severe constipation with abdominal distension, inability to pass wind, or vomiting, this could suggest bowel obstruction and needs urgent evaluation.
Be alert for symptoms of gallbladder disease, such as severe pain in the right upper abdomen, fever, or yellowing of the skin or eyes (jaundice), as GLP-1 receptor agonists have been associated with an increased risk of gallstone formation.
According to NICE guidance, patients on GLP-1 receptor agonists should have regular monitoring and review. If gastrointestinal side effects are significantly impacting your quality of life, preventing adequate nutrition, or causing weight loss beyond what is therapeutically intended, your GP may need to reassess whether Ozempic remains the most appropriate treatment option for you.
For urgent concerns outside of GP hours, contact NHS 111 for advice. For severe symptoms such as signs of shock, severe dehydration, or suspected bowel obstruction, call 999 or go to your nearest Emergency Department. Any suspected side effects can be reported through the MHRA Yellow Card scheme, which helps monitor the safety of medicines.
Finally, if you have pre-existing gastrointestinal conditions such as inflammatory bowel disease, gastroparesis, or a history of pancreatitis, any new or worsening symptoms whilst on Ozempic should be discussed with your healthcare provider promptly.
Diarrhoea is a very common side effect of Ozempic, occurring in more than 1 in 10 people taking the medication. It typically occurs during the first few weeks of treatment or after dose increases and often improves as your body adjusts.
Yes, some patients experience constipation rather than diarrhoea whilst taking Ozempic. Individual responses to the medication vary considerably, with some people having no change in bowel habits at all.
Contact your GP if you experience severe or persistent diarrhoea lasting more than a few days, signs of dehydration, severe abdominal pain, blood in stools, persistent vomiting, or severe constipation with abdominal distension. These symptoms may indicate complications requiring medical assessment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
Unordered list
Bold text
Emphasis
Superscript
Subscript