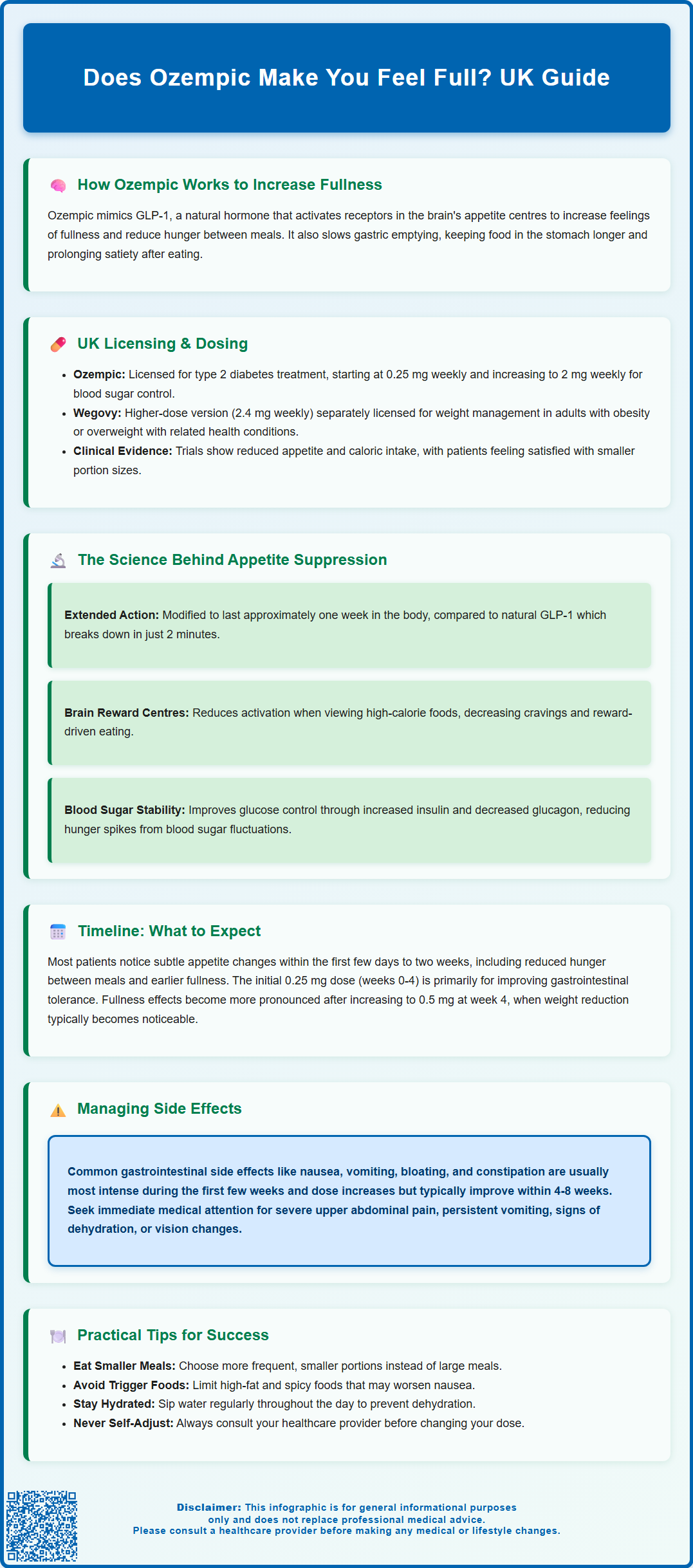
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus. Does Ozempic make you feel full? Yes—one of its key mechanisms is enhancing satiety, the sensation of fullness after eating, which often leads to reduced food intake. By mimicking the natural hormone GLP-1, Ozempic influences appetite centres in the brain and slows gastric emptying, helping patients feel satisfied with smaller portions. Understanding how this medication affects fullness can help set realistic expectations and support effective diabetes management.
Summary: Ozempic increases feelings of fullness by mimicking GLP-1 hormone, which slows gastric emptying and influences brain appetite centres to reduce hunger and enhance satiety.
- Semaglutide is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus treatment
- The medication delays gastric emptying and acts on hypothalamic appetite centres to promote fullness
- Satiety effects typically begin within days to two weeks, becoming more pronounced as doses increase from 0.25 mg to maintenance levels
- Common gastrointestinal side effects include nausea, vomiting, and abdominal discomfort, usually improving within 4-8 weeks
- Patients should monitor for hypoglycaemia when used with insulin or sulfonylureas, and report severe abdominal pain or persistent vomiting promptly
Table of Contents
How Ozempic Works to Increase Feelings of Fullness
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. One of its notable effects is the enhancement of satiety—the feeling of fullness after eating—which often leads to reduced food intake and subsequent weight reduction. This mechanism contributes to both its glucose-lowering properties and its impact on body weight.
The drug works by mimicking the action of naturally occurring GLP-1, a hormone released by the intestines in response to food intake. GLP-1 receptors are found throughout the body, including in brain regions that regulate appetite and satiety, particularly the hypothalamus and brainstem. When semaglutide binds to these receptors, it triggers signals that promote feelings of fullness and reduce hunger between meals.
Key mechanisms through which Ozempic increases fullness include:
-
Delayed gastric emptying – Ozempic slows the rate at which food leaves the stomach and enters the small intestine, prolonging the sensation of fullness after meals. This effect tends to be most pronounced early in treatment and may diminish over time with continued use.
-
Central appetite regulation – The medication influences appetite centres in the brain to reduce hunger signals and increase satiety signals
-
Enhanced post-meal satisfaction – Patients typically report feeling satisfied with smaller portion sizes
Clinical trials have demonstrated that patients taking semaglutide experience reductions in appetite and caloric intake. The MHRA-approved prescribing information notes that decreased appetite and reduced body weight are observed in patients treated with Ozempic. The dosing schedule begins with 0.25 mg once weekly for four weeks (to improve tolerability), then increases to 0.5 mg weekly. If additional glycaemic control is needed, the dose may be increased to 1 mg weekly after at least four weeks, and to 2 mg weekly if further improvement is required.
It is important to note that whilst Ozempic is licensed for type 2 diabetes in the UK, a higher-dose formulation (Wegovy, 2.4 mg weekly) is specifically licensed for weight management in adults with obesity or overweight with weight-related comorbidities, within specialist weight management services and according to NICE criteria (TA875).
The Science Behind Ozempic and Appetite Suppression
Understanding the scientific basis of how Ozempic suppresses appetite involves examining the complex interplay between gut hormones, neural pathways, and metabolic signalling. GLP-1 receptor agonists like semaglutide have enhanced our understanding of appetite regulation and provided new therapeutic options for managing both diabetes and obesity.
Naturally produced GLP-1 has a very short half-life in the body—approximately 2 minutes—as it is rapidly broken down by the enzyme dipeptidyl peptidase-4 (DPP-4). Semaglutide has been structurally modified to resist this enzymatic degradation, resulting in a half-life of approximately one week. This extended duration of action allows for once-weekly dosing and provides sustained appetite suppression throughout the dosing interval.
The appetite-suppressing effects of Ozempic involve several interconnected pathways:
Neurological pathways: Semaglutide appears to exert effects on key appetite-regulating regions in the brain. This may occur through direct central actions or via indirect pathways such as vagal signalling. Functional MRI studies have shown that GLP-1 receptor agonists can reduce activation in brain reward centres when patients view images of high-calorie foods, suggesting a reduction in food cravings and reward-driven eating.
Gastrointestinal effects: Beyond slowing gastric emptying, Ozempic may influence the secretion of other gut hormones involved in satiety signalling. Research suggests possible effects on hormones such as peptide YY (PYY) and ghrelin (often called the 'hunger hormone'), though evidence is mixed and these mechanisms remain under investigation.
Metabolic signalling: GLP-1 receptor activation stimulates glucose-dependent insulin secretion and reduces glucagon release, which helps control blood glucose levels. Better glycaemic control may indirectly influence appetite regulation by reducing the hunger spikes associated with blood sugar fluctuations.
Clinical studies have shown that semaglutide can reduce energy intake in controlled settings, with the effect varying by dose and individual factors. These effects appear to persist with continued treatment in clinical trials, though individual responses vary considerably. The NICE guidance on type 2 diabetes (NG28) acknowledges the role of GLP-1 receptor agonists in promoting weight reduction alongside glycaemic control in appropriate patient populations.
What to Expect: Timeline of Fullness Effects with Ozempic
Patients beginning Ozempic treatment often wonder when they will notice changes in appetite and fullness. The timeline of satiety effects varies between individuals, but general patterns have emerged from clinical experience and trial data. Understanding this timeline can help set realistic expectations and support treatment adherence.
Initial weeks (0-4 weeks): Many patients begin to notice subtle changes in appetite within the first few days to two weeks of starting Ozempic. The initial dose is 0.25 mg once weekly for the first four weeks—this is a dose-escalation period designed primarily to improve gastrointestinal tolerability rather than achieve maximum therapeutic effect. During this phase, some patients report:
-
Reduced hunger between meals
-
Earlier feelings of fullness when eating
-
Decreased interest in snacking
-
Mild nausea, which may temporarily reduce appetite further
Weeks 4-8: After the first month, the dose is usually increased to 0.5 mg weekly. At this stage, fullness effects typically become more pronounced and consistent. Patients often find they are satisfied with significantly smaller portions than previously. This is when weight reduction, if it occurs, usually becomes noticeable. The gastrointestinal system is also adapting to the medication during this period.
Weeks 8 and beyond: For some patients requiring enhanced glycaemic control, the dose may be increased to 1 mg weekly after at least four weeks on 0.5 mg. If additional glycaemic control is needed, the dose may be further increased to 2 mg weekly after at least four weeks on 1 mg. The satiety effects generally stabilise with continued treatment.
Important considerations: Individual responses vary considerably based on factors including baseline weight, dietary habits, concurrent medications, and metabolic factors. Some patients experience pronounced fullness immediately, whilst others notice more gradual changes. Regular review appointments with your healthcare provider are important to assess both the effectiveness of treatment (through HbA1c measurements and weight monitoring) and any side effects you may experience. The NHS recommends that diabetes treatments should be reviewed regularly to ensure they remain appropriate for your individual circumstances.
Managing Side Effects Related to Fullness and Satiety
Whilst the increased fullness from Ozempic is therapeutically beneficial, it can sometimes lead to uncomfortable side effects, particularly gastrointestinal symptoms. Effective management of these effects is crucial for treatment adherence and quality of life. Most side effects are most pronounced during dose escalation and tend to improve over time as the body adapts.
Common gastrointestinal side effects include:
-
Nausea (very common according to the SmPC) – typically mild to moderate and most common in the first few weeks
-
Vomiting – less common than nausea but can occur, especially if eating large portions
-
Abdominal discomfort or bloating – related to delayed gastric emptying
-
Constipation – may result from reduced food and fluid intake
-
Diarrhoea – affects some patients, though less commonly than constipation
Important safety considerations:
-
Hypoglycaemia risk – When Ozempic is used with insulin or sulfonylureas (e.g., gliclazide), there is an increased risk of low blood sugar. Your doctor may reduce your insulin or sulfonylurea dose when starting Ozempic. Monitor your blood glucose levels carefully and know the symptoms of hypoglycaemia.
-
Gallbladder problems – Semaglutide has been associated with an increased risk of gallstones. Contact your doctor if you experience severe pain in your upper abdomen, often radiating to your back, with or without fever or jaundice (yellowing of skin/eyes).
-
Diabetic retinopathy – If you have diabetic eye disease, rapid improvements in blood glucose can sometimes temporarily worsen eye problems. Report any vision changes promptly to your healthcare provider.
Practical strategies for managing fullness-related side effects:
Dietary modifications: Eat smaller, more frequent meals rather than large portions. Avoid lying down immediately after eating, as delayed gastric emptying can worsen reflux symptoms. Choose bland, easily digestible foods if experiencing nausea—ginger tea or dry crackers may help. Reduce intake of high-fat and spicy foods, which can exacerbate gastrointestinal symptoms.
Hydration: Maintain adequate fluid intake throughout the day, sipping water regularly rather than drinking large amounts at once. Dehydration can worsen nausea and constipation.
When to seek medical advice: Contact your GP or diabetes specialist nurse if you experience:
-
Persistent vomiting preventing adequate fluid or medication intake
-
Severe abdominal pain, especially if accompanied by fever
-
Signs of dehydration (dark urine, dizziness, reduced urination)
-
Inability to tolerate even small amounts of food or fluid
-
Symptoms of pancreatitis (severe upper abdominal pain radiating to the back)
The MHRA advises that patients should be counselled about the risk of gastrointestinal side effects before starting treatment. Most symptoms are self-limiting and resolve within 4-8 weeks. If side effects remain intolerable despite management strategies, dose reduction or treatment discontinuation may be necessary. Never adjust your dose without consulting your healthcare provider.
Patients are encouraged to report any suspected adverse reactions to medicines via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics (SmPC).
- Ozempic - European Public Assessment Report (EPAR).
- Type 2 diabetes in adults: management. NICE guideline NG28.
- Semaglutide for managing overweight and obesity. NICE technology appraisal guidance TA875.
- Once-Weekly Semaglutide in Adults with Overweight or Obesity.
- GLP-1 receptor activation modulates appetite- and reward-related brain areas in humans.
Frequently Asked Questions
How quickly does Ozempic make you feel full?
Many patients notice subtle changes in appetite within the first few days to two weeks of starting Ozempic. Fullness effects typically become more pronounced after the dose increases to 0.5 mg weekly at week four, with individual responses varying considerably.
Why does Ozempic reduce appetite?
Ozempic mimics the natural GLP-1 hormone, binding to receptors in the brain's appetite centres and slowing gastric emptying. This dual action reduces hunger signals, increases satiety, and prolongs the feeling of fullness after meals.
What should I do if Ozempic makes me feel too full or nauseous?
Eat smaller, more frequent meals, avoid lying down immediately after eating, and choose bland, easily digestible foods. If nausea or vomiting persists or prevents adequate fluid intake, contact your GP or diabetes specialist nurse for advice.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










