Wegovy®
Similar to Ozempic, Wegovy also contains semaglutide but is licensed for weight management. It helps reduce hunger and supports meaningful, long-term fat loss.
- Supports clinically proven weight reduction
- Weekly injection, easy to use

Does Ozempic make you thirsty? Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst increased thirst is not listed amongst common adverse effects in the MHRA-approved Summary of Product Characteristics, some patients do report this symptom during treatment. Thirst may arise from dehydration secondary to gastrointestinal side effects such as nausea, vomiting, or diarrhoea, or may signal hyperglycaemia or, rarely, diabetic ketoacidosis. Understanding the cause and knowing when to seek medical advice is essential for safe and effective diabetes management.
Summary: Ozempic (semaglutide) does not commonly cause thirst, but some patients report it due to dehydration from gastrointestinal side effects or as a sign of hyperglycaemia.
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Increased thirst is not listed amongst the common adverse effects in the Summary of Product Characteristics (SmPC) approved by the MHRA, though some patients do report experiencing thirst during treatment. Understanding whether this symptom is related to the medication or indicates another issue is essential for safe and effective management.
Ozempic works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite. These mechanisms help lower blood glucose levels and often lead to weight loss. Thirst can arise through several pathways when taking Ozempic: it may reflect dehydration secondary to gastrointestinal side effects such as nausea, vomiting, or diarrhoea—common reactions, particularly during dose titration. The SmPC warns that these effects can lead to dehydration and potentially acute kidney injury in some cases. Alternatively, thirst may signal hyperglycaemia if diabetes control is suboptimal.
It is also important to recognise that thirst is a hallmark symptom of diabetic ketoacidosis (DKA), a rare but serious complication. While DKA is rare with GLP-1 receptor agonists, cases have been reported, particularly when concomitant insulin is rapidly reduced or discontinued. The MHRA advises that insulin dose adjustments should be gradual with close monitoring. Patients should be educated to distinguish between mild, manageable thirst and symptoms requiring urgent medical attention. This article provides evidence-based guidance on recognising, managing, and escalating concerns about thirst whilst taking Ozempic.
Mild to moderate thirst during Ozempic therapy is often benign and may result from common gastrointestinal side effects. Nausea, vomiting, and diarrhoea—reported in clinical trials and listed in the SmPC—can lead to fluid loss and subsequent dehydration. This type of thirst typically improves with adequate oral hydration and tends to resolve as the body adjusts to the medication, usually within the first few weeks of treatment or following dose escalation. Patients may also experience a dry mouth, which can contribute to the sensation of thirst without necessarily indicating systemic dehydration.
However, persistent or severe thirst warrants careful evaluation to exclude more serious underlying causes. If thirst is accompanied by polyuria (excessive urination), this may indicate poor glycaemic control or hyperglycaemia. Patients should be advised to monitor their blood glucose levels if they have access to home testing equipment. If experiencing symptoms such as sweating, tremor, palpitations, confusion, or dizziness, patients should check their blood glucose as these may indicate hypoglycaemia, particularly in those taking concomitant insulin or sulphonylureas.
Red flag symptoms that require urgent medical assessment include:
Severe, unquenchable thirst combined with excessive urination
Nausea and vomiting that prevents oral fluid intake
Abdominal pain, particularly if severe or persistent
Rapid breathing or shortness of breath
Fruity-smelling breath
Confusion, drowsiness, or altered consciousness
These features may indicate diabetic ketoacidosis (DKA), a medical emergency. If hyperglycaemic and unwell, patients should check blood or urine ketones if available and seek urgent care if positive or symptomatic. The MHRA has highlighted that DKA can occur when concomitant insulin is rapidly reduced or discontinued when starting a GLP-1 receptor agonist. Any insulin dose changes should be gradual with close monitoring. Patients should never abruptly reduce or stop insulin without medical supervision.
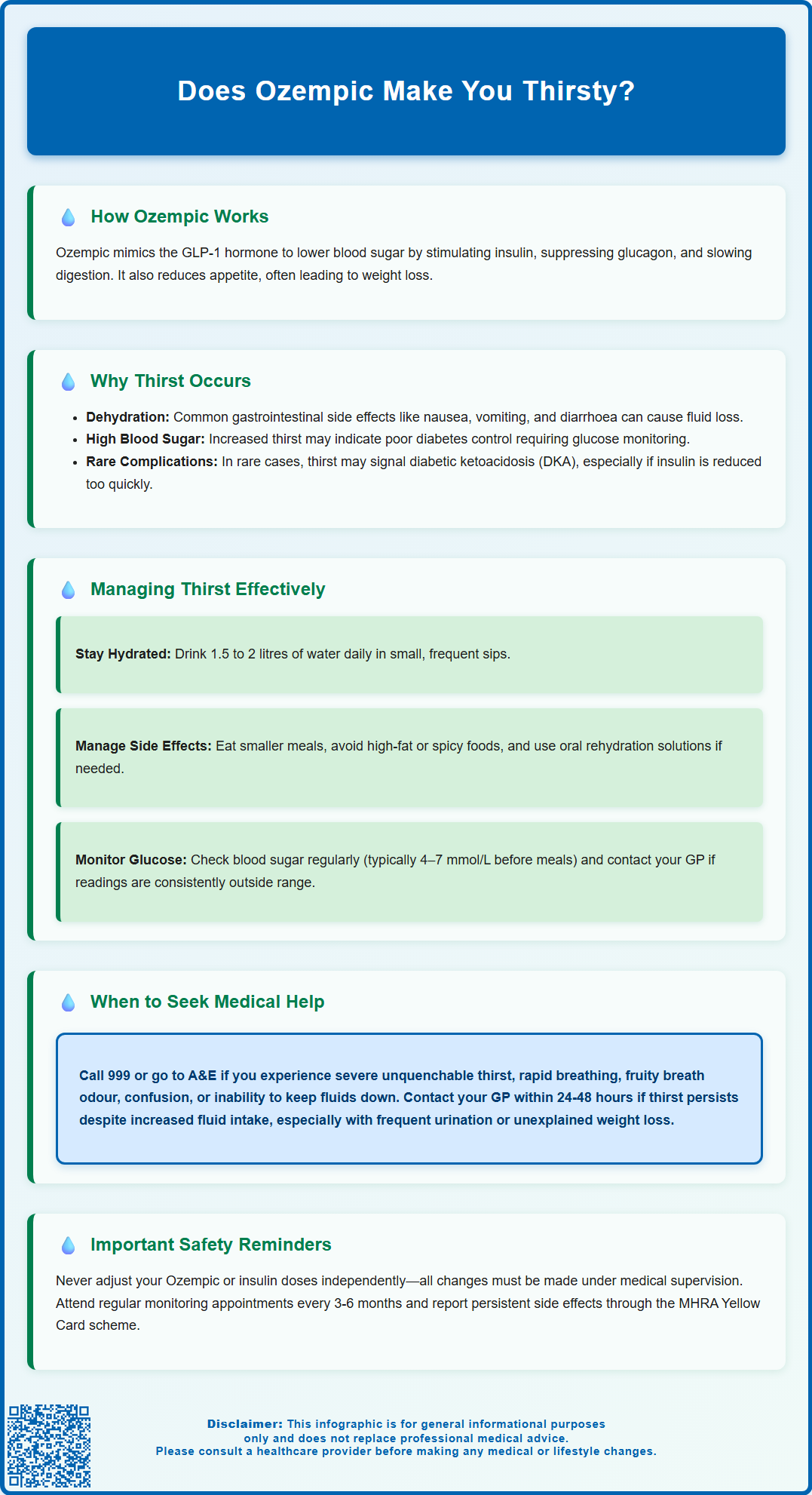
Adequate hydration is the cornerstone of managing mild thirst associated with Ozempic therapy. Patients should be encouraged to drink water regularly throughout the day, aiming for approximately 1.5 to 2 litres daily, adjusted for individual needs, activity levels, and climate. Sipping water frequently, rather than consuming large volumes at once, may help, particularly for those experiencing nausea or delayed gastric emptying—a known pharmacological effect of semaglutide.
For patients experiencing gastrointestinal side effects, practical strategies can minimise fluid loss and associated thirst:
Eat smaller, more frequent meals to reduce nausea
Avoid high-fat, spicy, or heavily seasoned foods that may exacerbate gastrointestinal symptoms
Consider oral rehydration solutions if diarrhoea is problematic
Take Ozempic as prescribed, following the recommended dose escalation schedule to allow the body to adjust gradually
If unable to keep fluids down or experiencing ongoing vomiting or diarrhoea, seek clinical advice promptly as there is a risk of dehydration and acute kidney injury. Some medicines may need temporary review during illness, but patients should not alter insulin doses without medical advice.
Monitoring blood glucose levels is essential, as hyperglycaemia can manifest with thirst. Patients should be educated on their individualised glucose targets as advised by their diabetes care team. According to Diabetes UK, typical self-monitoring targets for adults with type 2 diabetes are 4–7 mmol/L before meals and less than 8.5 mmol/L two hours after meals, but these should be personalised. If blood glucose readings are consistently outside target range, patients should contact their GP or diabetes specialist nurse for medication review.
Lifestyle modifications can also support overall diabetes management. Maintaining a balanced diet rich in fibre, lean protein, and vegetables helps stabilise blood glucose levels. Regular physical activity improves insulin sensitivity and glycaemic control. Patients should be advised to drink water and sugar-free fluids, while avoiding excessive caffeine, alcohol, and sugar-sweetened beverages that can raise glucose levels and contribute to dehydration.
It is important to note that dose adjustments should only be made under medical supervision. The standard titration schedule for Ozempic begins at 0.25 mg once weekly for four weeks, increasing to 0.5 mg weekly, with further escalation to 1 mg or 2 mg if additional glycaemic control is required. Patients should never alter their dose independently in response to side effects without consulting their healthcare provider.
Routine follow-up with your GP or diabetes care team is an integral part of Ozempic therapy. However, certain symptoms associated with thirst require more urgent attention. Patients should contact their GP within 24 to 48 hours if they experience persistent thirst that does not improve with increased fluid intake, particularly if accompanied by frequent urination, unexplained weight loss, or fatigue. These symptoms may indicate inadequate diabetes control and warrant blood glucose monitoring and possible medication adjustment.
Immediate medical attention is required if thirst is accompanied by any of the following:
Severe or persistent vomiting or diarrhoea leading to inability to maintain hydration
Signs of dehydration such as dizziness, reduced urine output, dark-coloured urine, or dry mucous membranes
Symptoms suggestive of hypoglycaemia (blood glucose below 4 mmol/L) that do not resolve with standard treatment
Severe abdominal pain, which may indicate pancreatitis—a rare but serious adverse effect of GLP-1 receptor agonists
Symptoms of DKA, including rapid breathing, fruity breath odour, confusion, or loss of consciousness
If pancreatitis is suspected (severe, persistent abdominal pain, possibly radiating to the back), stop taking semaglutide and seek urgent medical assessment.
Patients should be advised to attend A&E or call 999 if they develop signs of DKA or severe dehydration, particularly if they are unable to keep fluids down or if they feel increasingly unwell. For urgent clinical advice when the situation is not immediately life-threatening, NHS 111 is also available. Healthcare professionals should provide clear safety-netting advice at initiation of therapy and during follow-up consultations.
Regular monitoring as recommended by NICE includes HbA1c measurement every 3 to 6 months, renal function tests, and assessment for adverse effects. Patients should be encouraged to maintain open communication with their diabetes care team and report any new or concerning symptoms promptly. Suspected side effects can be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app). For those experiencing persistent side effects, alternative GLP-1 receptor agonists or other glucose-lowering therapies may be considered. Shared decision-making between patient and clinician ensures that treatment remains both effective and tolerable, optimising long-term diabetes management and quality of life.
Thirst is not listed as a common side effect in the MHRA-approved Summary of Product Characteristics for Ozempic, but some patients report it, often due to dehydration from gastrointestinal side effects such as nausea, vomiting, or diarrhoea.
Seek urgent medical attention if thirst is accompanied by severe vomiting, persistent abdominal pain, rapid breathing, fruity-smelling breath, confusion, or signs of diabetic ketoacidosis. These symptoms require immediate assessment.
Drink 1.5 to 2 litres of water daily, sip fluids regularly, eat smaller meals to reduce nausea, and monitor blood glucose levels. If thirst persists or worsens, contact your GP or diabetes care team for advice.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
Unordered list
Bold text
Emphasis
Superscript
Subscript