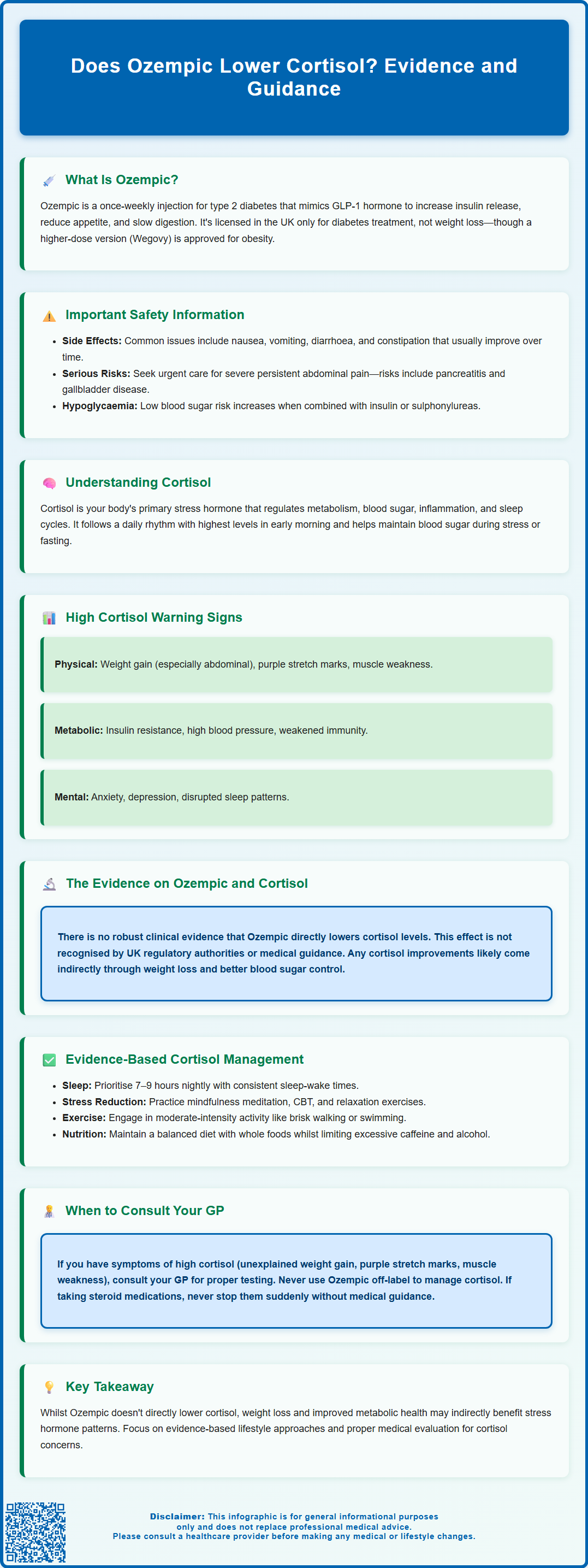
Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, known for its glucose-lowering and weight loss effects. Many patients wonder whether Ozempic lowers cortisol, the body's primary stress hormone. Whilst cortisol plays essential roles in metabolism, stress response, and immune function, chronic elevation can contribute to weight gain and metabolic disturbances. Currently, there is no robust clinical evidence or UK regulatory guidance indicating that semaglutide directly reduces cortisol levels. This article examines the relationship between Ozempic, weight loss, and cortisol regulation, alongside evidence-based approaches to managing stress hormones.
Summary: There is no robust clinical evidence or UK regulatory guidance showing that Ozempic (semaglutide) directly lowers cortisol levels.
- Ozempic is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, not for cortisol reduction.
- Weight loss from any method may indirectly influence cortisol metabolism and HPA axis function.
- Cortisol is regulated by the hypothalamic-pituitary-adrenal axis and responds to stress, sleep, and metabolic factors.
- Elevated cortisol concerns require GP evaluation, including screening tests such as late-night salivary cortisol or 24-hour urinary free cortisol.
- Evidence-based cortisol management includes stress reduction, sleep hygiene, regular physical activity, and balanced nutrition.
- Patients taking steroid medicines must never stop abruptly and should discuss any dose changes with their prescriber.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medication with a UK marketing authorisation for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists. Ozempic is administered as a once-weekly subcutaneous injection and has gained considerable attention not only for its glucose-lowering effects but also for its associated weight loss benefits.
The mechanism of action of Ozempic centres on mimicking the naturally occurring hormone GLP-1, which is released by the intestines in response to food intake. By binding to GLP-1 receptors, semaglutide enhances insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it stimulates insulin release only when blood glucose levels are elevated. This reduces the risk of hypoglycaemia, though this risk increases significantly when used in combination with insulin or sulfonylureas, which may require dose reduction of these medications. Additionally, Ozempic suppresses glucagon secretion, slows gastric emptying, and acts on appetite centres in the brain to promote satiety and reduce food intake.
In the UK, Ozempic is recommended by the National Institute for Health and Care Excellence (NICE) as a treatment option for adults with type 2 diabetes who meet specific criteria. Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, which are typically mild to moderate and often diminish over time. Important safety considerations include the risk of acute pancreatitis (seek urgent medical attention for severe, persistent abdominal pain), gallbladder disease, and potential worsening of diabetic retinopathy, particularly in patients with pre-existing retinopathy who experience rapid improvement in blood glucose control.
While clinical trials have shown cardiovascular benefits with semaglutide, it is not licensed in the UK for cardiovascular risk reduction. Similarly, Ozempic is not licensed in the UK for weight management outside the context of diabetes, although a higher-dose formulation (Wegovy) has a specific licence for obesity treatment. Patients should report any suspected side effects via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Understanding Cortisol and Its Role in the Body
Cortisol is a steroid hormone produced by the adrenal glands, which sit atop each kidney. Often referred to as the body's primary 'stress hormone', cortisol plays a vital role in numerous physiological processes. It is released in response to stress and low blood glucose levels, following a circadian rhythm with peak levels typically occurring in the early morning and declining throughout the day.
Cortisol has several essential functions in the body. It helps regulate metabolism by influencing how the body uses carbohydrates, fats, and proteins for energy. During periods of stress or fasting, cortisol promotes gluconeogenesis (the production of glucose from non-carbohydrate sources) in the liver, ensuring adequate blood sugar levels. It also has anti-inflammatory and immunosuppressive properties, which is why synthetic corticosteroids are used therapeutically to treat inflammatory conditions. Furthermore, cortisol affects blood pressure regulation, mood, and the sleep-wake cycle.
Whilst cortisol is essential for health, chronic elevation of cortisol levels can have detrimental effects. Prolonged exposure to high cortisol is associated with weight gain (particularly central obesity), insulin resistance, hypertension, mood disturbances including anxiety and depression, impaired immune function, and bone density loss. The most common cause of Cushing's syndrome (a condition of excess cortisol) is long-term or high-dose steroid medication use. Importantly, patients taking prescribed steroids should never stop them abruptly and should always discuss any dose changes with their prescriber. Conversely, insufficient cortisol production (as seen in Addison's disease) can lead to fatigue, low blood pressure, and metabolic disturbances.
Cortisol levels can be measured through various methods, including blood tests, salivary samples, and 24-hour urine collections. Common screening tests for suspected high cortisol include late-night salivary cortisol, 24-hour urinary free cortisol, and the overnight dexamethasone suppression test. For suspected low cortisol, a morning (9 am) cortisol test or short Synacthen test may be used. The hypothalamic-pituitary-adrenal (HPA) axis tightly regulates cortisol production, and disruptions to this system can result from chronic stress, certain medications, tumours, or autoimmune conditions.
How Weight Loss Medications May Affect Stress Hormones
The relationship between weight loss medications such as Ozempic and stress hormones like cortisol is an area of emerging interest, though current evidence remains limited. There is no robust human clinical evidence or regulatory guidance showing that semaglutide (Ozempic) directly lowers cortisol. UK regulatory sources, including the Summary of Product Characteristics (SmPC), NICE guidance, and European Medicines Agency assessment reports, do not list any cortisol-lowering effect or indication for semaglutide. However, several indirect mechanisms warrant consideration.
Weight loss itself, regardless of the method achieved, may influence cortisol levels. Obesity is associated with dysregulation of the HPA axis, and some studies suggest that individuals with excess weight may have altered cortisol metabolism. When significant weight loss occurs—whether through lifestyle modification, bariatric surgery, or pharmacotherapy—there may be improvements in HPA axis function. Some research indicates that weight reduction can lead to normalisation of cortisol patterns, though findings are inconsistent and depend on individual factors such as the degree of weight loss, baseline metabolic health, and psychological stress levels.
GLP-1 receptor agonists like Ozempic may also have indirect effects on stress and mood. Improved glycaemic control and weight loss can enhance overall wellbeing, potentially reducing psychological stress and, consequently, stress-related cortisol secretion. Additionally, animal studies have suggested that GLP-1 receptors are present in brain regions involved in stress response, though the clinical significance of this in humans remains unclear.
It is important to note that patients should not expect Ozempic to function as a cortisol-lowering agent. If you have concerns about elevated cortisol or symptoms suggestive of Cushing's syndrome (such as unexplained weight gain, purple striae, or muscle weakness), it is essential to consult your GP for appropriate investigation, which may include cortisol testing and referral to an endocrinologist. If you are taking steroid medicines, remember that these are the most common cause of high cortisol levels; never stop taking them suddenly, and always discuss any concerns with your prescriber. Self-medicating or using Ozempic off-label for cortisol management is not advised and could pose safety risks.
Managing Cortisol Levels: Evidence-Based Approaches
For individuals concerned about elevated cortisol levels, there are several evidence-based strategies that can help promote healthy stress hormone regulation. These approaches focus on lifestyle modifications and, where appropriate, medical intervention.
Stress management techniques are fundamental. Chronic psychological stress is a primary driver of sustained cortisol elevation. Practices such as mindfulness meditation, cognitive behavioural therapy (CBT), and relaxation exercises have been shown in studies to reduce perceived stress and may help normalise cortisol patterns. The NHS offers resources and referrals for psychological support, including NHS Talking Therapies for anxiety and depression.
Sleep hygiene is equally important. Poor sleep quality and insufficient sleep duration can disrupt the natural circadian rhythm of cortisol secretion. Adults should aim for 7–9 hours of quality sleep per night, maintaining consistent sleep and wake times. Avoiding caffeine and electronic screens before bedtime can support better sleep.
Regular physical activity has been demonstrated to help regulate cortisol levels, though the relationship is complex. Moderate-intensity exercise such as brisk walking, swimming, or cycling can reduce stress and improve overall metabolic health. However, excessive high-intensity training without adequate recovery may temporarily elevate cortisol, so balance is key.
Nutritional considerations also play a role. A balanced diet rich in whole foods, adequate protein, healthy fats, and complex carbohydrates supports metabolic health. Excessive caffeine and alcohol intake should be limited, as both can influence cortisol secretion.
If lifestyle measures are insufficient or if there is clinical suspicion of a pathological cause of elevated cortisol (such as Cushing's syndrome), medical evaluation is essential. Your GP may arrange appropriate investigations, including first-line screening tests such as late-night salivary cortisol, 24-hour urinary free cortisol, or an overnight dexamethasone suppression test, before referring to an endocrinologist if necessary. If you're taking steroid medicines, do not stop them suddenly as this can be dangerous; always discuss dose changes with your prescriber. Treatment for genuine hypercortisolism depends on the underlying cause and may involve medication, surgery, or radiotherapy. Never attempt to self-diagnose or self-treat suspected cortisol imbalances—professional medical guidance is crucial for safe and effective management.
Frequently Asked Questions
Can Ozempic be used to lower cortisol levels?
No, Ozempic is not licensed or indicated for lowering cortisol. There is no robust clinical evidence showing that semaglutide directly reduces cortisol levels, and it should not be used for this purpose.
How can I tell if my cortisol levels are too high?
Symptoms of high cortisol may include unexplained weight gain (especially around the abdomen), purple stretch marks, muscle weakness, and mood changes. Your GP can arrange screening tests such as late-night salivary cortisol or 24-hour urinary free cortisol if clinically indicated.
What are evidence-based ways to manage cortisol levels?
Evidence-based approaches include stress management techniques (mindfulness, CBT), maintaining good sleep hygiene (7–9 hours nightly), regular moderate-intensity exercise, and a balanced diet. If pathological causes are suspected, consult your GP for appropriate investigation and referral.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript