Does Ozempic help PCOS? This question has gained attention as women with polycystic ovary syndrome (PCOS) seek effective treatments for metabolic and reproductive symptoms. Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, not PCOS. However, emerging research suggests potential benefits for weight loss and insulin sensitivity in women with PCOS. While evidence remains limited and prescribing would be off-label, understanding the relationship between Ozempic and PCOS can help inform discussions with healthcare providers about appropriate, evidence-based treatment options tailored to individual needs.
Summary: Ozempic is not licensed for PCOS in the UK, though emerging research suggests potential benefits for weight loss and insulin sensitivity when used off-label.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed only for type 2 diabetes in the UK, not for PCOS treatment.
- Limited research shows GLP-1 agonists may improve weight, insulin sensitivity, and menstrual regularity in women with PCOS.
- Off-label use requires specialist assessment, effective contraception, and discontinuation at least 2 months before planned pregnancy.
- NHS-approved PCOS treatments include lifestyle modification, combined oral contraceptive pill, metformin, and anti-androgen therapy.
- Common side effects include gastrointestinal symptoms; rare risks include pancreatitis and gallbladder disease requiring monitoring.
Table of Contents
What Is Ozempic and How Does It Work?
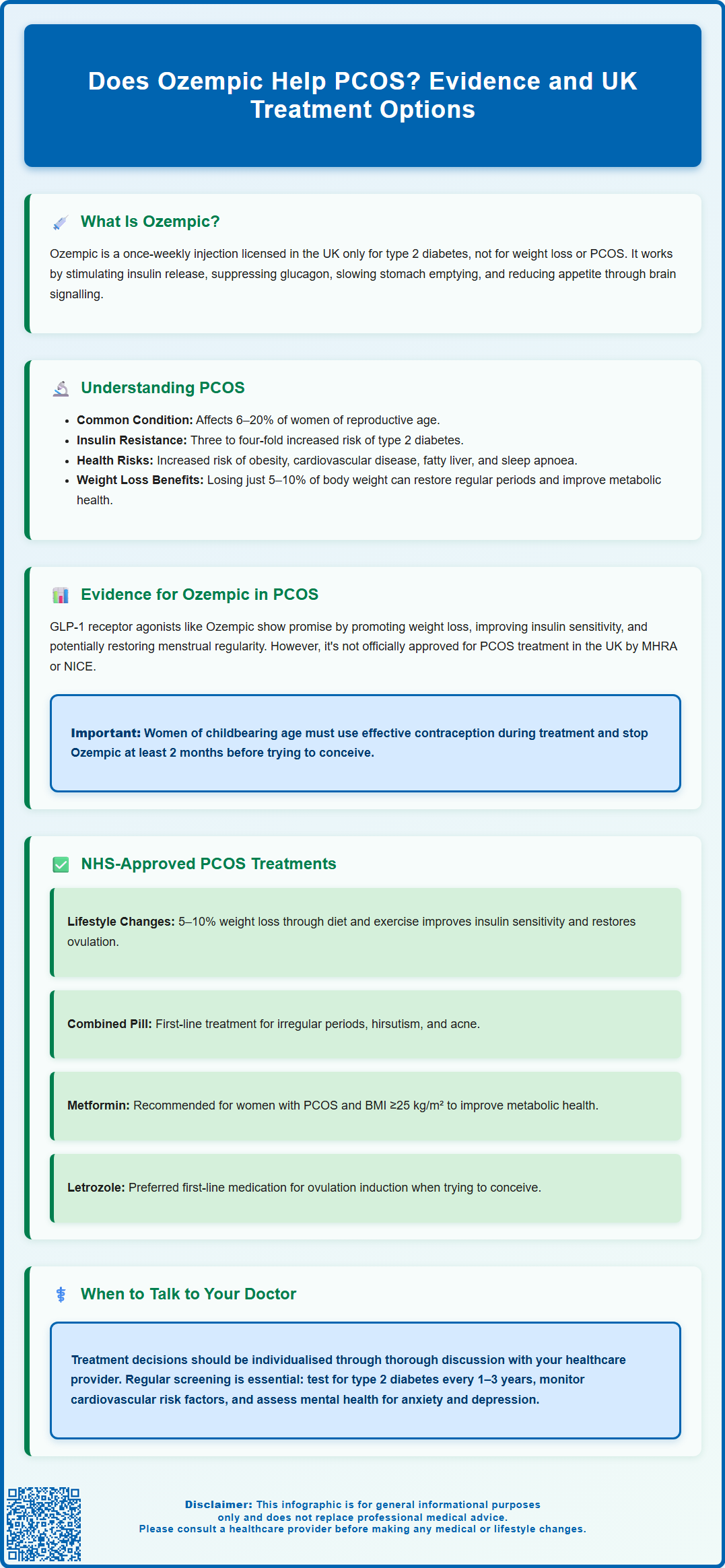
Ozempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists. Ozempic is administered as a once-weekly subcutaneous injection and works by mimicking the action of a naturally occurring hormone called GLP-1, which is released by the intestines in response to food intake.
The primary mechanism of action involves several complementary effects. Ozempic stimulates insulin secretion from the pancreas in a glucose-dependent manner, meaning it only promotes insulin release when blood sugar levels are elevated. This reduces the risk of hypoglycaemia when used alone, though this risk increases if combined with insulin or sulfonylureas. Additionally, it suppresses glucagon secretion, a hormone that raises blood glucose levels, thereby helping to maintain more stable blood sugar control throughout the day.
Beyond its effects on glucose regulation, Ozempic also slows gastric emptying, which means food moves more slowly from the stomach into the small intestine. This contributes to increased feelings of fullness and satiety, though this effect may attenuate with continued use. Furthermore, semaglutide acts on appetite centres in the brain, reducing hunger and food intake. These combined effects often result in weight loss, which has led to considerable interest in its potential applications beyond diabetes management.
It is important to note that in the UK, Ozempic is licensed specifically for type 2 diabetes and is not currently approved by the MHRA for weight management alone or for polycystic ovary syndrome (PCOS). A related medication, Wegovy (also semaglutide but at a higher dose), has separate licensing for weight management in specific circumstances.
Women of childbearing age should be aware that Ozempic is not recommended during pregnancy or breastfeeding. Effective contraception should be used during treatment, and Ozempic should be discontinued at least 2 months before a planned pregnancy.
Understanding PCOS and Its Metabolic Effects
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorders affecting women of reproductive age, with an estimated prevalence of 6–20% depending on diagnostic criteria used. PCOS is characterised by a combination of reproductive, metabolic, and psychological features that can significantly impact quality of life and long-term health outcomes.
The hallmark features of PCOS include irregular or absent menstrual periods (oligomenorrhoea or amenorrhoea), clinical or biochemical signs of excess androgens (male hormones) such as hirsutism, acne, and male-pattern hair loss, and polycystic ovarian morphology visible on ultrasound scanning. Diagnosis typically requires the presence of at least two of these three features, according to the Rotterdam criteria commonly used in UK clinical practice.
A critical aspect of PCOS is its strong association with metabolic dysfunction. Many women with PCOS exhibit insulin resistance, meaning their body's cells do not respond effectively to insulin, leading to compensatory hyperinsulinaemia (elevated insulin levels). This insulin resistance contributes to difficulties with weight management and increases the risk of developing type 2 diabetes—women with PCOS have approximately a three to four-fold increased risk compared to the general population.
Furthermore, PCOS is associated with an increased prevalence of obesity, dyslipidaemia (abnormal cholesterol levels), non-alcoholic fatty liver disease, obstructive sleep apnoea, and cardiovascular risk factors including hypertension. The metabolic disturbances in PCOS create a complex interplay between reproductive dysfunction and cardiometabolic health. Weight loss of just 5–10% can significantly improve both metabolic and reproductive outcomes in women with PCOS, including restoration of ovulation and menstrual regularity, which is why lifestyle modification remains a cornerstone of management.
Women with prolonged amenorrhoea are at risk of endometrial hyperplasia due to unopposed oestrogen action. Therefore, regular assessment and management of menstrual health is essential, with induction of withdrawal bleeds recommended at least every 3–4 months in women who are not menstruating regularly. Screening for type 2 diabetes (using HbA1c or oral glucose tolerance test), lipid abnormalities, and blood pressure should be performed at diagnosis and periodically thereafter, according to individual risk factors.
Evidence for Ozempic Use in PCOS Management
While Ozempic is not licensed for PCOS treatment in the UK, there is growing research interest in GLP-1 receptor agonists for managing the metabolic aspects of this condition. Several clinical studies have investigated semaglutide and related medications in women with PCOS, primarily focusing on weight loss, insulin sensitivity, and metabolic parameters.
Emerging evidence suggests that GLP-1 receptor agonists may offer benefits in PCOS management. Research studies have demonstrated that these medications can promote significant weight reduction in women with PCOS who are overweight or obese—often achieving greater weight loss than lifestyle modification alone. Additionally, improvements in insulin sensitivity, glycaemic control, and lipid profiles have been observed in some trials. Some studies have also reported improvements in menstrual regularity and ovulation rates, likely secondary to the metabolic improvements and weight loss achieved.
However, it is crucial to emphasise that the evidence base remains limited compared to established PCOS treatments. Most studies have been relatively small, short-term, or have used liraglutide (a different GLP-1 agonist) rather than semaglutide specifically. There is currently no official MHRA or NICE endorsement for using Ozempic in PCOS management, and it would be considered off-label prescribing in this context.
Potential adverse effects of Ozempic include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, which are particularly common when initiating treatment or increasing doses. The risk of hypoglycaemia is low when Ozempic is used alone but increases when combined with insulin or sulfonylureas. More serious but rare risks include pancreatitis, gallbladder disease, and potential thyroid effects.
Women considering GLP-1 therapy should have a thorough discussion with their healthcare provider about the balance of potential benefits and risks, particularly given the off-label nature of such use. Any prescribing decision should be individualised and based on comprehensive assessment of metabolic status, weight, and PCOS-related symptoms.
Importantly, women of childbearing age should use effective contraception during treatment with semaglutide, as it is not recommended during pregnancy or breastfeeding. The medication should be discontinued at least 2 months before a planned pregnancy. Weight loss may also restore ovulation in previously anovulatory women, potentially increasing fertility.
Patients should report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app). It is also worth noting that there are currently supply constraints for GLP-1 receptor agonists in the UK, and off-label prescribing should follow local NHS policies and specialist guidance.
NHS-Approved Treatments for PCOS
The NHS and NICE provide clear guidance on evidence-based treatments for PCOS, with management tailored to individual symptoms and priorities. The cornerstone of PCOS management remains lifestyle modification, including dietary changes and increased physical activity aimed at achieving modest weight loss. Even a 5–10% reduction in body weight can significantly improve insulin sensitivity, restore ovulatory function, and reduce cardiovascular risk factors.
For menstrual irregularity and contraception, the combined oral contraceptive pill (COCP) is typically first-line treatment. The COCP helps regulate menstrual cycles, reduces androgen levels, and can improve hirsutism and acne. For women who cannot take oestrogen-containing contraceptives, cyclical progestogen therapy (such as medroxyprogesterone acetate) can be used to induce regular withdrawal bleeds and protect the endometrium from prolonged oestrogen exposure. Women with oligomenorrhoea or amenorrhoea should have a withdrawal bleed induced at least every 3–4 months to reduce the risk of endometrial hyperplasia.
Metformin, an insulin-sensitising medication, is recommended by NICE for women with PCOS who have a BMI ≥25 kg/m² (or lower in certain ethnic groups), particularly when the COCP is contraindicated or not tolerated, or for those with metabolic features such as impaired glucose tolerance. Metformin can improve metabolic parameters and may help with weight management and menstrual regularity, though it is not licensed specifically for PCOS in the UK. Common side effects include gastrointestinal upset, which can often be minimised by gradual dose escalation and taking the medication with food.
For hirsutism and acne, treatment options include the COCP, topical eflornithine cream for facial hair, and anti-androgen medications such as spironolactone or cyproterone acetate (often combined with oestrogen as co-cyprindiol). Effective contraception is essential with anti-androgens due to their potential teratogenicity. Spironolactone requires monitoring of potassium and renal function, while co-cyprindiol carries a small increased risk of venous thromboembolism. Physical treatments like laser hair removal or electrolysis may also be considered.
For women seeking fertility treatment, ovulation induction is typically managed by specialists. Letrozole is generally recommended as first-line therapy for ovulation induction in PCOS, with clomifene citrate as an alternative if letrozole is unsuitable or unavailable. Referral to specialist fertility services is appropriate if initial treatments are unsuccessful after 6-12 months.
Women with PCOS should undergo regular screening for type 2 diabetes (HbA1c or oral glucose tolerance test at diagnosis and every 1-3 years depending on risk factors), cardiovascular risk factors including lipids and blood pressure, and mental health concerns including anxiety and depression.
When to contact your GP: seek medical advice if you experience very irregular or heavy periods, prolonged amenorrhoea, difficulty conceiving after 12 months of trying, rapid-onset or worsening hirsutism, signs of virilisation (deepening voice, increased muscle mass, clitoral enlargement), or concerns about weight gain or metabolic health. Urgent referral is needed for suspected virilisation, rapid-onset hirsutism, or heavy abnormal bleeding. Early intervention and ongoing monitoring can significantly improve both short-term symptoms and long-term health outcomes in PCOS.
Frequently Asked Questions
Is Ozempic approved for PCOS treatment in the UK?
No, Ozempic is not approved by the MHRA for PCOS treatment in the UK. It is licensed only for type 2 diabetes, and any use for PCOS would be considered off-label prescribing requiring specialist assessment.
What are the NHS-recommended treatments for PCOS?
NHS-recommended PCOS treatments include lifestyle modification for weight loss, the combined oral contraceptive pill for menstrual regulation, metformin for metabolic features, and anti-androgen therapy for hirsutism. Treatment is tailored to individual symptoms and priorities.
Can Ozempic improve fertility in women with PCOS?
Weight loss from Ozempic may restore ovulation in some women with PCOS, potentially improving fertility. However, effective contraception is essential during treatment, and Ozempic must be stopped at least 2 months before planned pregnancy as it is not recommended during pregnancy.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript