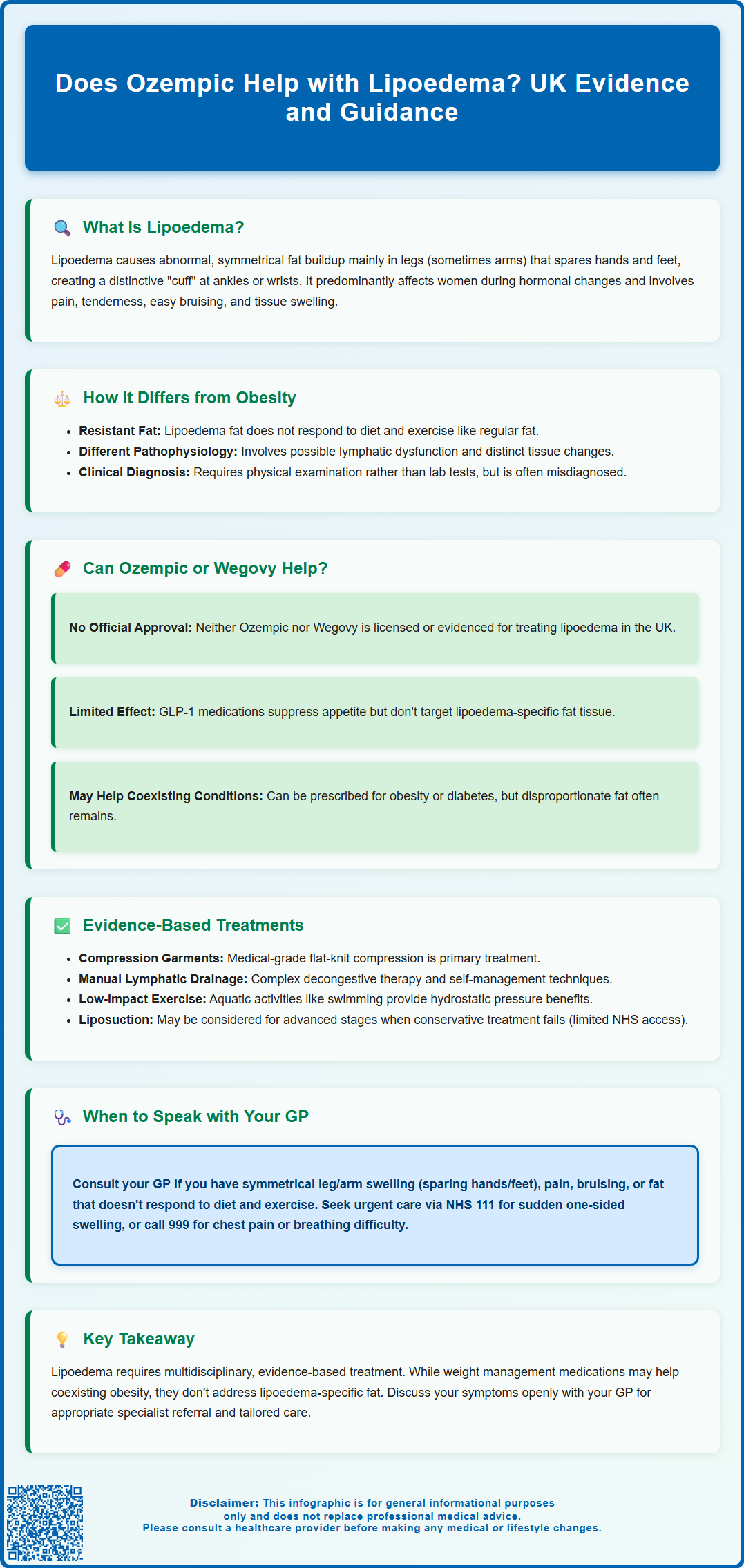
Lipoedema is a chronic condition causing abnormal, symmetrical fat accumulation, predominantly in the legs and arms, affecting mainly women. Unlike general obesity, lipoedema tissue is resistant to diet and exercise, often causing pain and disproportionate body shape. Many patients explore whether medications like Ozempic (semaglutide), a GLP-1 receptor agonist used for type 2 diabetes, might help manage lipoedema. However, there is currently no licensed indication or robust clinical evidence supporting Ozempic for lipoedema treatment. This article examines the relationship between Ozempic and lipoedema, evidence-based management options, and when to seek medical advice.
Summary: Ozempic (semaglutide) is not licensed for lipoedema and there is no clinical evidence demonstrating its effectiveness in treating this condition.
- Ozempic is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, not lipoedema
- Lipoedema fat is resistant to conventional weight loss methods including appetite-suppressing medications
- Evidence-based lipoedema management includes compression therapy, manual lymphatic drainage, and exercise
- Liposuction may be considered for advanced lipoedema under NICE guidance with special arrangements
- Patients should consult their GP for proper lipoedema diagnosis and multidisciplinary management
Table of Contents
What Is Lipoedema and How Does It Differ from Obesity?
Lipoedema is a chronic condition characterised by the abnormal and symmetrical accumulation of subcutaneous adipose tissue, predominantly affecting the lower limbs and sometimes the arms. Unlike generalised obesity, lipoedema typically spares the hands and feet, creating a distinct 'cuff' appearance at the ankles or wrists. The condition affects predominantly women, often manifesting or worsening during periods of hormonal change such as puberty, pregnancy, or menopause.
The key distinguishing features of lipoedema include:
-
Symmetrical distribution of fat deposits, usually from hips to ankles
-
Disproportionate appearance between upper and lower body
-
Pain and tenderness in affected areas, often described as bruising easily
-
Resistance to diet and exercise – the affected tissue does not respond well to conventional weight loss methods
-
Non-pitting tissue swelling and a feeling of heaviness in the legs
Clinically, lipoedema differs from obesity in its pathophysiology. Whilst obesity involves generalised excess adipose tissue that typically responds to caloric restriction and increased physical activity, lipoedema represents a disorder of adipose tissue distribution with possible microvascular and lymphatic involvement. Research suggests there may be differences in the adipose tissue and impaired lymphatic function in lipoedema, though the exact mechanisms remain under investigation.
Diagnosis is primarily clinical, based on history and physical examination. There is currently no definitive laboratory test for lipoedema, though imaging such as ultrasound or MRI may help exclude other conditions including lymphoedema, chronic venous disease, lipohypertrophy and hypothyroidism. Many patients with lipoedema experience delayed diagnosis, often being told simply to 'lose weight', which can be both ineffective and demoralising.
It's important to note that obesity and lipoedema can co-exist, and weight management remains beneficial for overall health even if the disproportionate fat distribution persists.
Does Ozempic Help with Lipoedema?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Semaglutide is also available as Wegovy, which is specifically licensed for weight management in adults with obesity or overweight with weight-related comorbidities. The medication works by mimicking the action of the naturally occurring hormone GLP-1, which enhances insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways.
Currently, there is no official evidence or MHRA-licensed indication for Ozempic or Wegovy in the treatment of lipoedema. The effect of GLP-1 receptor agonists on lipoedema-specific adipose tissue is unknown. Because lipoedema fat is often resistant to dietary restriction and exercise, medications that primarily work through appetite suppression and metabolic effects may have different impacts on lipoedema tissue compared to general adiposity.
Some patients with lipoedema who also have concurrent obesity or type 2 diabetes may be prescribed GLP-1 receptor agonists for those licensed indications. In such cases, whilst overall body weight may decrease, the disproportionate fat distribution characteristic of lipoedema often persists. Anecdotal reports exist within patient communities, but robust clinical trial data specifically examining semaglutide's efficacy in lipoedema are lacking.
Common side effects of semaglutide include nausea, vomiting, diarrhoea, constipation and abdominal pain. Rarer but serious side effects can include pancreatitis and gallbladder problems. Semaglutide should not be used during pregnancy or breastfeeding. If you experience any side effects, report them via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Access to Wegovy for weight management in the UK is via specialist weight management services according to NICE guidance (TA875), with specific eligibility criteria including BMI thresholds and weight-related conditions.
It is important to note that lipoedema requires a multidisciplinary approach, and any medication should be considered only as part of a comprehensive management plan. Patients should discuss their individual circumstances, including any diagnosis of lipoedema, with their GP or specialist to ensure appropriate, evidence-based care.
Evidence-Based Treatments for Lipoedema in the UK
Management of lipoedema in the UK focuses on symptom control, preventing progression, and improving quality of life. The cornerstone of treatment is conservative management, which typically includes:
-
Compression therapy: Medical-grade compression garments individually prescribed by a lymphoedema specialist. Flat-knit compression is often preferred over circular-knit for lipoedema due to the tissue characteristics.
-
Complex Decongestive Therapy (CDT): A comprehensive approach including specialist-prescribed compression, skin care, manual lymphatic drainage (MLD) performed by trained therapists, and self-management techniques.
-
Exercise: Low-impact activities such as swimming, walking, and cycling are encouraged. Aquatic exercise is particularly beneficial due to the hydrostatic pressure supporting tissue health.
-
Healthy nutrition: Whilst lipoedema fat does not typically respond to caloric restriction alone, maintaining a balanced diet helps manage any concurrent obesity and supports overall metabolic health.
For patients with advanced lipoedema (stages 2–3) who have not responded adequately to conservative measures, liposuction may be considered. According to NICE Interventional Procedures Guidance, liposuction for chronic lipoedema has limited evidence and should only be used with special arrangements for clinical governance, consent, and audit or research. Tumescent liposuction and water-assisted liposuction (WAL) may reduce tissue volume and improve symptoms, but ongoing compression and conservative management remain essential post-surgery. Access to liposuction for lipoedema on the NHS is limited and varies by region, often requiring individual funding requests.
Psychological support is also important, as lipoedema can significantly impact body image, mental health, and quality of life. Referral to counselling or support groups may be beneficial.
Patients should be under the care of a multidisciplinary team, ideally including a GP with an interest in lipoedema, lymphoedema specialists, dietitians, and physiotherapists. The Lymphoedema Support Network and Lipoedema UK provide valuable resources and support for patients. Early intervention and consistent management can help slow progression and maintain mobility and function.
When to Speak with Your GP About Lipoedema and Weight Loss
If you suspect you have lipoedema, or if you have been struggling with disproportionate fat distribution that does not respond to diet and exercise, it is important to seek medical advice. Early consultation with your GP can facilitate timely diagnosis and access to appropriate management strategies. Consider booking an appointment if you experience:
-
Symmetrical swelling in your legs or arms that spares the hands and feet
-
Pain, tenderness, or easy bruising in the affected areas
-
Heaviness or aching in the limbs, particularly worsening throughout the day
-
Lack of response to conventional weight loss efforts in specific areas
-
Impact on mobility or quality of life due to limb size or discomfort
During your consultation, be prepared to describe your symptoms in detail, including when they started, any family history of similar issues, and how they affect your daily activities. Your GP may perform a physical examination and may refer you to a specialist lymphoedema service or vascular specialist for further assessment.
Seek urgent medical attention if you develop:
-
Sudden unilateral (one-sided) leg swelling, which could indicate deep vein thrombosis (DVT) – contact NHS 111 or seek same-day assessment
-
Chest pain or shortness of breath with leg swelling – call 999 as this could indicate a pulmonary embolism
If you are considering medications for weight management, discuss your lipoedema diagnosis or suspicion openly with your GP. This ensures that any treatment plan is tailored to your specific needs and that realistic expectations are set regarding outcomes. Your GP can advise whether you meet the criteria for referral to specialist weight management services where treatments such as Wegovy (semaglutide) might be considered under NICE guidance (TA875). Note that Ozempic is not licensed for weight management and should not be requested for this purpose.
Additionally, if you experience sudden worsening of swelling, skin changes (such as redness, warmth, or ulceration), or signs of infection, seek medical attention promptly. These may indicate complications such as cellulitis or progression to lipolymphoedema, which require urgent management.
The Lymphoedema Support Network and Lipoedema UK provide valuable resources, including service finders to help locate specialist care in your area. Your GP can help coordinate a comprehensive, individualised care plan and provide appropriate referrals.
Scientific References
- Semaglutide for managing overweight and obesity.
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Rybelsus 3 mg - Summary of Product Characteristics.
- Discussing results and referral | Overweight and obesity management (NG246).
- The effects of GLP-1 receptor agonists on visceral fat and liver and nonalcoholic fatty liver disease: A systematic review and meta-analysis.
- Liposuction for chronic lipoedema.
Frequently Asked Questions
Can Ozempic be prescribed for lipoedema in the UK?
No, Ozempic (semaglutide) is not licensed by the MHRA for lipoedema treatment. It is only licensed for type 2 diabetes, and there is no clinical trial evidence supporting its use specifically for lipoedema.
What are the recommended treatments for lipoedema?
Evidence-based lipoedema management includes compression therapy with medical-grade garments, complex decongestive therapy, manual lymphatic drainage, low-impact exercise, and healthy nutrition. For advanced cases, specialist liposuction may be considered under NICE guidance.
When should I see my GP about lipoedema?
Consult your GP if you experience symmetrical leg or arm swelling sparing hands and feet, pain or tenderness in affected areas, heaviness in limbs, or disproportionate fat distribution that does not respond to diet and exercise. Early diagnosis enables timely access to specialist lymphoedema services.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript