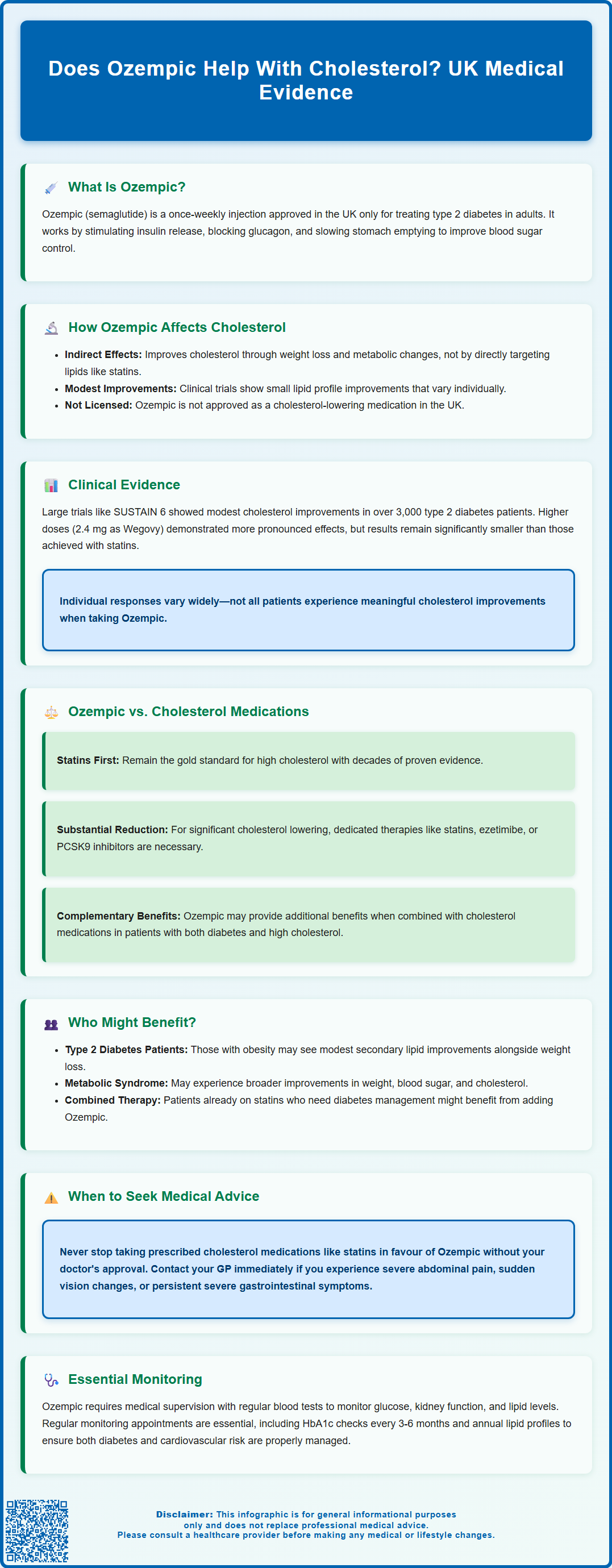
Does Ozempic help with cholesterol? Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, not cholesterol reduction. Whilst clinical trials have shown modest improvements in lipid profiles as secondary outcomes, these effects are indirect and primarily linked to weight loss. Ozempic is not a substitute for dedicated cholesterol-lowering medications such as statins. This article examines the evidence for Ozempic's effects on cholesterol, how it compares with established lipid therapies, and important considerations for patients with both diabetes and dyslipidaemia.
Summary: Ozempic may lead to modest improvements in cholesterol levels as a secondary effect, primarily through weight loss, but it is not licensed or recommended as a cholesterol-lowering medication in the UK.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed for type 2 diabetes treatment, not cholesterol management.
- Any cholesterol improvements occur indirectly through weight reduction and improved metabolic health rather than direct lipid-lowering mechanisms.
- Clinical trials show modest lipid profile improvements, but these are considerably smaller than reductions achieved with statins or dedicated cholesterol therapies.
- Patients requiring cholesterol reduction should follow NICE-recommended lipid-lowering treatments such as statins, not rely on Ozempic alone.
- Regular monitoring of lipid profiles and HbA1c is essential for patients taking Ozempic, with treatment decisions guided by comprehensive cardiovascular risk assessment.
Table of Contents
- Understanding Ozempic and Its Primary Uses
- How Ozempic May Affect Cholesterol Levels
- Clinical Evidence on Ozempic and Lipid Profiles
- Comparing Ozempic with Dedicated Cholesterol Medications
- Who Might Benefit from Ozempic's Cholesterol Effects
- Important Considerations and When to Seek Medical Advice
- Frequently Asked Questions
Understanding Ozempic and Its Primary Uses
Ozempic (semaglutide) is a prescription medication primarily licensed for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medicines called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that regulates blood sugar levels.
The medication is administered as a once-weekly subcutaneous injection and functions through several mechanisms. Semaglutide stimulates insulin secretion when blood glucose levels are elevated, suppresses the release of glucagon (a hormone that raises blood sugar), and slows gastric emptying. These combined actions help improve glycaemic control in people with type 2 diabetes. Additionally, Ozempic affects appetite regulation centres in the brain, often leading to reduced food intake and subsequent weight loss.
In the UK, Ozempic is approved for diabetes management, not weight management. According to NICE guideline NG28, GLP-1 receptor agonists like Ozempic may be considered for adults with type 2 diabetes who have specific criteria, including a BMI of 35 kg/m² or higher (adjusted for ethnicity) and specific problems associated with high weight, or a BMI lower than 35 kg/m² where insulin would have significant occupational implications or weight loss would benefit other significant obesity-related comorbidities.
It's important to note that while Ozempic may lead to weight reduction, it is not licensed for weight management in the UK. A higher dose of semaglutide (2.4 mg) is available under the brand name Wegovy specifically for weight management under specialist supervision.
Whilst Ozempic's primary indication remains diabetes treatment, clinical trials have revealed additional metabolic effects beyond glucose control. These secondary benefits have generated considerable interest amongst healthcare professionals and patients alike, particularly regarding cardiovascular risk factors such as cholesterol levels.
How Ozempic May Affect Cholesterol Levels
The relationship between Ozempic and cholesterol is indirect rather than direct. Unlike statins, which specifically target cholesterol synthesis, semaglutide influences lipid profiles through multiple interconnected metabolic pathways. The most significant mechanism appears to be weight reduction, which commonly occurs during Ozempic treatment and can lead to improvements in various cardiovascular risk markers, including cholesterol.
Clinical observations suggest that Ozempic may lead to modest improvements in lipid profiles in some patients, though individual responses vary considerably. These effects are generally observed as secondary outcomes in clinical trials, with the primary improvements in lipid parameters appearing to correlate with the degree of weight loss achieved.
The mechanisms underlying these lipid changes are multifactorial. Weight loss itself improves insulin sensitivity and reduces hepatic fat accumulation, both of which influence lipid metabolism. Additionally, improved glycaemic control may contribute to better overall metabolic health. Changes in dietary patterns that often accompany Ozempic treatment may further contribute to improved lipid profiles.
It is important to emphasise that Ozempic is not licensed as a cholesterol-lowering medication in the UK. Any effects on cholesterol should be considered secondary benefits rather than primary therapeutic targets. Patients with elevated cholesterol requiring specific lipid management should not rely on Ozempic alone but should follow evidence-based cholesterol treatment protocols as recommended by their healthcare team.
Clinical Evidence on Ozempic and Lipid Profiles
The evidence base for Ozempic's effects on cholesterol comes primarily from large-scale cardiovascular outcome trials conducted as part of the medication's development programme. The landmark SUSTAIN clinical trial series evaluated semaglutide in thousands of patients with type 2 diabetes, providing data on various metabolic parameters including lipid profiles.
In the SUSTAIN 6 trial (published in the New England Journal of Medicine, 2016), which examined cardiovascular outcomes in over 3,000 patients with type 2 diabetes at high cardiovascular risk, participants receiving semaglutide demonstrated statistically significant reductions in major adverse cardiovascular events. Secondary analyses revealed modest improvements in lipid parameters, though these were not primary endpoints of the study.
It's important to note that the STEP clinical trial programme investigated higher doses of semaglutide (2.4 mg, marketed as Wegovy) specifically for weight management, not the lower doses used in Ozempic for diabetes. These studies showed that greater weight loss was generally associated with more pronounced improvements in metabolic markers, including lipid profiles. However, these findings relate to the weight-management dose of semaglutide rather than standard Ozempic dosing for diabetes.
However, it is crucial to contextualise these findings. The cholesterol reductions observed with Ozempic are considerably smaller than those achieved with dedicated lipid-lowering therapies such as statins. Furthermore, the lipid effects of semaglutide show considerable individual variation, and not all patients experience meaningful improvements. The European Medicines Agency (EMA) assessment reports acknowledge these lipid effects but emphasise that they represent secondary benefits rather than primary therapeutic outcomes for which the medication should be prescribed.
Comparing Ozempic with Dedicated Cholesterol Medications
When considering cholesterol management, it is essential to understand how Ozempic compares with established lipid-lowering therapies recommended by NICE and other UK clinical guidelines. Statins remain the first-line treatment for elevated cholesterol and cardiovascular risk reduction, with decades of robust evidence demonstrating significant reductions in cardiovascular events and mortality.
Statins work by inhibiting HMG-CoA reductase, an enzyme crucial for cholesterol synthesis in the liver, typically achieving substantial reductions in non-HDL cholesterol. In contrast, Ozempic's effects on cholesterol are modest and inconsistent across individuals. For patients requiring substantial cholesterol reduction to meet NICE-recommended targets (typically a 40% reduction in non-HDL cholesterol from baseline), statins or other dedicated lipid therapies would be necessary.
Ezetimibe, another commonly prescribed cholesterol medication, reduces cholesterol absorption in the intestine and can lower non-HDL cholesterol by approximately 15-20%. For patients with high cardiovascular risk, additional options include PCSK9 inhibitors and newer agents such as inclisiran (NICE TA733) and bempedoic acid (NICE TA694). These medications have specific, predictable effects on lipid profiles that far exceed the secondary benefits observed with Ozempic.
That said, Ozempic may offer complementary benefits when used alongside dedicated cholesterol medications in patients with both type 2 diabetes and dyslipidaemia. The combination of improved glycaemic control, weight reduction, and modest lipid improvements may contribute to overall cardiovascular risk reduction. However, clinical decisions should be guided by comprehensive cardiovascular risk assessment (e.g., QRISK3) and adherence to NICE guideline NG238 for cardiovascular disease risk assessment and reduction, which provides clear guidance on lipid modification based on individual risk profiles. Ozempic should never be considered a replacement for evidence-based cholesterol therapy when such treatment is clinically indicated.
Who Might Benefit from Ozempic's Cholesterol Effects
Whilst Ozempic is not prescribed specifically for cholesterol management, certain patient groups may experience secondary benefits on their lipid profiles. Individuals with type 2 diabetes and concurrent obesity represent the primary population who might benefit from these effects, particularly when weight reduction could improve multiple cardiovascular risk factors simultaneously.
Patients with mildly elevated cholesterol who are already taking Ozempic for diabetes management may find that the medication contributes to modest improvements in their lipid profile. However, this should only be assessed through regular monitoring and in consultation with healthcare professionals. It is important to note that Ozempic should not be initiated solely for cholesterol management in patients without type 2 diabetes.
For weight management in non-diabetic patients, the higher dose of semaglutide (2.4 mg, brand name Wegovy) may be prescribed under specialist supervision according to NICE guidance, but this is distinct from Ozempic's use in diabetes care.
Individuals with metabolic syndrome—a cluster of conditions including abdominal obesity, elevated blood pressure, raised blood sugar, and abnormal cholesterol levels—may experience broader metabolic improvements with Ozempic treatment. The medication's effects on weight, glucose metabolism, and lipids may collectively contribute to reducing cardiovascular risk in this population, though dedicated treatments for each component of metabolic syndrome remain important.
Patients already taking statins who require additional diabetes management might benefit from Ozempic's complementary effects. The combination of proven lipid-lowering therapy with the metabolic benefits of GLP-1 receptor agonists may provide additive cardiovascular protection. However, treatment decisions should always be individualised based on comprehensive risk assessment, existing comorbidities, and alignment with current NICE guidance for both diabetes (NG28) and cardiovascular disease management (NG238). Regular monitoring of lipid profiles through blood tests remains essential to ensure therapeutic targets are being achieved.
Important Considerations and When to Seek Medical Advice
Patients considering or currently taking Ozempic should understand several important safety considerations and monitoring requirements. Ozempic is a prescription-only medication that requires proper medical supervision, including regular blood tests to monitor glucose control, kidney function, and lipid profiles. Self-medication or obtaining Ozempic through unregulated sources poses significant health risks and should be avoided.
Common side effects of Ozempic include nausea, vomiting, diarrhoea, constipation, and abdominal pain, particularly when initiating treatment or increasing doses. These gastrointestinal effects usually diminish over time but can be troublesome for some patients. More serious but rare adverse effects include pancreatitis and gallbladder problems.
Important safety information from the UK product information includes:
-
Diabetic retinopathy complications: Patients with a history of diabetic retinopathy should be monitored closely, and any sudden vision changes require urgent medical attention
-
Hypoglycaemia risk: Increased risk when used with sulfonylureas or insulin; dose adjustments of these medications may be needed
-
Pregnancy and breastfeeding: Ozempic should not be used during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception. A 2-month washout period is recommended before planned pregnancy
Regarding cholesterol management specifically, patients should never discontinue prescribed cholesterol medications in favour of Ozempic without explicit guidance from their GP or specialist. Stopping statins or other lipid-lowering therapies could significantly increase cardiovascular risk, particularly in patients with established cardiovascular disease or high-risk profiles.
You should contact your GP or healthcare team if you:
-
Experience persistent or severe gastrointestinal symptoms that affect your quality of life
-
Develop severe abdominal pain that could indicate pancreatitis
-
Notice unexplained weight loss beyond expected therapeutic effects
-
Experience any sudden changes in vision
-
Have concerns about your cholesterol levels or cardiovascular risk
-
Are planning pregnancy or become pregnant while taking Ozempic
-
Experience any unexpected symptoms or side effects during treatment
Suspected side effects should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Regular review appointments are essential for patients taking Ozempic, typically including HbA1c monitoring every 3-6 months and annual lipid profile assessments as part of comprehensive diabetes care. Your healthcare team can interpret these results in the context of your overall health and adjust treatment strategies accordingly, ensuring that both diabetes management and cardiovascular risk reduction are optimally addressed through evidence-based approaches aligned with current UK clinical guidelines.
Frequently Asked Questions
Can Ozempic replace statins for cholesterol management?
No, Ozempic cannot replace statins for cholesterol management. Statins remain the first-line treatment for elevated cholesterol with decades of robust evidence, whilst Ozempic's effects on cholesterol are modest, indirect, and secondary to its diabetes indication.
How does Ozempic affect cholesterol levels?
Ozempic may lead to modest improvements in lipid profiles indirectly through weight loss, improved insulin sensitivity, and reduced hepatic fat accumulation. These effects vary considerably between individuals and are not the primary therapeutic purpose of the medication.
Should I stop taking my cholesterol medication if I start Ozempic?
No, you should never discontinue prescribed cholesterol medications without explicit guidance from your GP or specialist. Stopping statins or other lipid-lowering therapies could significantly increase cardiovascular risk, particularly in high-risk patients.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript