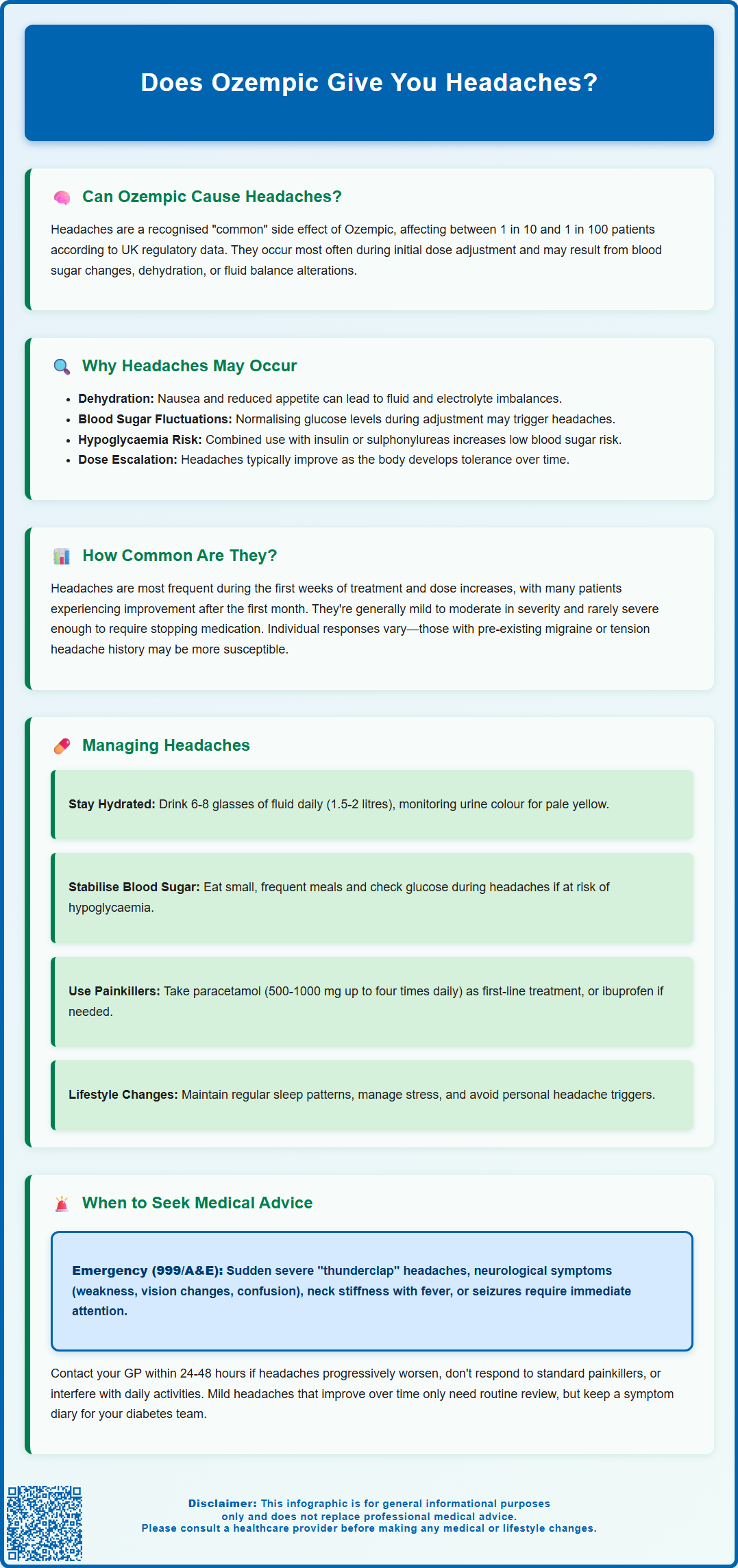
Does Ozempic give you headaches? This is a common concern for patients prescribed semaglutide for type 2 diabetes. Ozempic, a GLP-1 receptor agonist licensed in the UK, is recognised for its effectiveness in glycaemic control, but headaches are listed as a known adverse effect in the MHRA-approved Summary of Product Characteristics. Classified as 'common', headaches affect between 1 in 10 and 1 in 100 patients. Understanding why they occur, how frequently, and how to manage them can help patients continue treatment safely whilst minimising discomfort. This article examines the evidence, mechanisms, and practical management strategies for Ozempic-related headaches.
Summary: Ozempic can cause headaches, classified as a 'common' adverse effect affecting between 1 in 10 and 1 in 100 patients according to MHRA-approved prescribing information.
- Semaglutide is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus treatment.
- Headaches may result from gastrointestinal effects causing dehydration, blood glucose fluctuations, or dose escalation during initial treatment phases.
- Most headaches are mild to moderate, often transient, and typically diminish after the first month of therapy as tolerance develops.
- Management includes adequate hydration, stable blood glucose levels, simple analgesics like paracetamol, and lifestyle modifications.
- Seek immediate medical attention for sudden severe headache, neurological symptoms, altered consciousness, neck stiffness with fever, or persistent severe vomiting.
- Routine monitoring and open communication with diabetes care teams allow for treatment adjustments if headaches significantly impact quality of life.
Table of Contents
Can Ozempic Cause Headaches?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Whilst it has demonstrated significant efficacy in glycaemic control, patients and healthcare professionals frequently enquire about its adverse effect profile, particularly regarding headaches.
Headaches are listed as a recognised adverse effect of Ozempic in the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA). According to the SmPC, headaches are classified as a 'common' adverse reaction (affecting between 1 in 10 and 1 in 100 patients). Clinical trial data and post-marketing surveillance have documented headaches occurring in patients receiving semaglutide, though the relationship is not always straightforward. It is important to note that headaches are common in the general population, and establishing a definitive causal link to any medication requires careful consideration of timing, pattern, and alternative explanations.
The mechanism by which Ozempic may contribute to headaches is not fully elucidated, but several plausible pathways exist. These include changes in blood glucose levels, alterations in fluid balance, and gastrointestinal effects leading to dehydration. The risk of hypoglycaemia-related headaches is generally low with Ozempic monotherapy but increases when used in combination with sulfonylureas or insulin, as noted in the SmPC. Patients starting Ozempic should be aware that headaches may occur, particularly during the initial titration phase, but this does not necessarily mean the medication is unsuitable for continued use. A thorough assessment of headache characteristics, frequency, and severity is essential to determine whether they are likely related to semaglutide therapy or represent an independent condition requiring separate investigation.
Why Headaches May Occur with Ozempic
Understanding the potential mechanisms behind Ozempic-related headaches can help both patients and clinicians manage this adverse effect more effectively. GLP-1 receptor agonists like semaglutide exert multiple physiological effects that may contribute to headache development through various pathways.
Gastrointestinal effects represent one of the most common and well-documented mechanisms. Ozempic frequently causes nausea, vomiting, and reduced appetite—effects that are central to its therapeutic action but may lead to inadequate fluid and food intake. Dehydration and electrolyte imbalances resulting from these gastrointestinal symptoms can trigger headaches. Additionally, nausea itself is often accompanied by headache as part of a broader symptom complex.
Changes in blood glucose levels may also play a role. Whilst Ozempic is designed to improve glycaemic control, the adjustment period as glucose levels normalise can sometimes be associated with headaches, particularly in patients whose blood sugar has been chronically elevated. Rapid changes in glucose can affect cerebral function. Patients taking Ozempic with insulin or sulfonylureas should be particularly vigilant about hypoglycaemia, which can manifest with headache among other symptoms.
Some research suggests that GLP-1 receptor agonists may have modest effects on blood pressure, typically causing small reductions. The MHRA SmPC notes that semaglutide may cause a small decrease in systolic blood pressure. While it is hypothesised that such changes could potentially contribute to headaches in some individuals, this relationship has not been firmly established in clinical studies.
Finally, the dose escalation schedule itself may be relevant. According to the SmPC, Ozempic is initiated at 0.25 mg weekly for 4 weeks, then increased to 0.5 mg weekly, with further increases to 1 mg or 2 mg weekly if needed. Headaches reported during titration may reflect the body's adjustment to the medication, and symptoms often improve as tolerance develops over subsequent weeks.
How Common Are Headaches When Taking Ozempic?
Quantifying the precise incidence of headaches associated with Ozempic requires examination of clinical trial data and real-world evidence. In the pivotal SUSTAIN clinical trial programme that supported Ozempic's licensing, headaches were reported as an adverse event, though they were not among the most frequently occurring side effects.
According to the MHRA-approved SmPC, headaches are classified as a 'common' adverse reaction, meaning they affect between 1 in 10 and 1 in 100 patients taking semaglutide. The European Medicines Agency's European Public Assessment Report (EPAR) for Ozempic provides additional context from the clinical development programme. Importantly, headaches also occurred in placebo groups, which complicates the attribution of causality. The background rate of headache in the general population is substantial—tension-type headaches affect up to 40% of adults annually—making it challenging to definitively link every headache to medication use.
The frequency appears highest during the initial weeks of treatment and during dose escalation periods. Many patients report that headaches diminish or resolve completely after the first month of therapy, suggesting an adaptation effect. Headaches severe enough to cause treatment discontinuation are uncommon.
Post-marketing surveillance through the MHRA's Yellow Card scheme has collected additional real-world data, though it's important to note that spontaneous reporting systems cannot determine true incidence rates. Whilst headaches are reported, they remain less common than gastrointestinal adverse effects such as nausea, vomiting, and diarrhoea, which the SmPC lists as 'very common' (affecting more than 1 in 10 patients). It is worth noting that individual susceptibility varies considerably—some patients experience no headaches whatsoever, whilst others may find them troublesome, particularly if they have a pre-existing history of migraine or tension headaches. Healthcare professionals should counsel patients that whilst headaches can occur, they are generally mild to moderate in severity and often transient.
Managing Headaches While on Ozempic
Effective management of headaches during Ozempic therapy involves both preventative strategies and symptomatic treatment. A systematic approach can help patients continue benefiting from the medication whilst minimising discomfort.
Ensuring adequate hydration is important. Patients should be advised to:
-
Aim for 6-8 glasses of fluid daily (approximately 1.5-2 litres), adjusting based on individual needs and medical conditions
-
Be cautious with higher fluid intake if you have heart failure or kidney disease—discuss appropriate targets with your healthcare provider
-
Monitor urine colour as a hydration indicator (pale yellow suggests adequate hydration)
-
Consider oral rehydration solutions if gastrointestinal symptoms are prominent
-
Avoid excessive caffeine, which can contribute to both dehydration and headaches
Maintaining stable blood glucose levels helps prevent headaches related to glycaemic fluctuations. Patients should continue regular meals even if appetite is reduced, focusing on small, frequent portions of easily digestible foods. Blood glucose monitoring should follow your individualised care plan—it's particularly important if you're taking Ozempic with insulin or sulfonylureas, or if you develop symptoms that could indicate hypoglycaemia (including headache). Check your glucose levels during headaches if you're at risk of hypoglycaemia.
Simple analgesics can provide symptomatic relief when needed. Paracetamol (500-1000 mg up to four times daily, maximum 4g in 24 hours, with at least 4 hours between doses) is generally the first-line option and is safe to use alongside Ozempic. Ibuprofen or other NSAIDs (200-400 mg up to three times daily with food) may be used if paracetamol is insufficient, provided there are no contraindications such as renal impairment, peptic ulcer disease, asthma, pregnancy, cardiovascular disease, or concomitant use of anticoagulants. Patients should avoid overuse of analgesics (more than 10-15 days per month) to prevent medication-overuse headache.
Lifestyle modifications can also help:
-
Maintaining regular sleep patterns
-
Managing stress through relaxation techniques
-
Avoiding known headache triggers (certain foods, alcohol, strong odours)
-
Ensuring adequate rest during the adjustment period
If headaches persist beyond the first month or worsen despite these measures, patients should consult their prescribing clinician. Following the SmPC guidance, Ozempic is initiated at 0.25 mg weekly for 4 weeks, then increased to 0.5 mg weekly, with further increases to 1 mg or 2 mg if needed. Your clinician may consider a slower titration schedule, temporary dose reduction, or other strategies. In some cases, switching to an alternative GLP-1 receptor agonist with a different pharmacokinetic profile may be considered.
When to Seek Medical Advice About Headaches
Whilst most headaches associated with Ozempic are benign and self-limiting, certain features warrant prompt medical assessment. Patients and healthcare professionals should be alert to warning signs that may indicate a more serious underlying condition requiring urgent evaluation.
Seek immediate medical attention (call 999 or attend A&E) if headaches are accompanied by:
-
Sudden onset of severe headache ("thunderclap" pattern) reaching maximum intensity within seconds to minutes
-
Neurological symptoms including weakness, numbness, visual disturbances, speech difficulties, or confusion
-
Altered consciousness or difficulty staying awake
-
Neck stiffness with fever, which may suggest meningitis
-
Seizures or loss of consciousness
-
Severe, persistent vomiting that prevents oral intake and medication
-
Severe, persistent abdominal pain with or without vomiting, which could indicate pancreatitis (a rare but serious adverse effect noted in the Ozempic SmPC)
For patients over 50, new-onset headache with scalp tenderness, jaw pain when chewing, or visual symptoms requires urgent same-day assessment to exclude giant cell arteritis.
If you feel unwell with headache, check your blood glucose and ketones if you have testing equipment, especially if you take insulin or sulfonylureas alongside Ozempic, or if you also take an SGLT2 inhibitor. Seek urgent medical advice if you have signs of hypoglycaemia or diabetic ketoacidosis.
Contact your GP or diabetes specialist nurse within 24-48 hours if:
-
Headaches are progressively worsening over days or weeks despite simple measures
-
The pattern of headaches changes significantly from your usual experience
-
Headaches are severe enough to interfere with daily activities or are not responding to standard analgesics
-
You experience persistent visual disturbances, even without other neurological symptoms (note that the Ozempic SmPC warns about potential worsening of diabetic retinopathy, particularly with rapid improvement in glucose control)
-
Headaches are accompanied by unexplained weight loss, night sweats, or fever
-
You have a history of migraine and the character of headaches has changed substantially
Routine review is appropriate if headaches are mild, improving over time, and responding to simple analgesia and hydration. However, patients should maintain open communication with their diabetes care team, as persistent headaches may occasionally necessitate treatment modification. NICE guidance (NG28) on type 2 diabetes management emphasises individualised treatment approaches, and if adverse effects significantly impact quality of life, alternative therapeutic options should be explored. Documentation of headache frequency, severity, and associated symptoms in a diary can provide valuable information for clinical decision-making.
If you experience side effects from Ozempic or any medication, you can report them through the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk.
Scientific References
- Ozempic | European Public Assessment Report.
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Type 2 diabetes in adults: management (NG28).
- Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes (SUSTAIN-6).
- GLP-1 receptor agonists: reminder of the potential side effects and to be aware of the potential for misuse.
Frequently Asked Questions
How long do Ozempic headaches typically last?
Most Ozempic-related headaches occur during the initial weeks of treatment and dose escalation periods, with many patients reporting improvement or complete resolution after the first month as the body adapts to the medication.
Can I take paracetamol for headaches whilst on Ozempic?
Yes, paracetamol is safe to use alongside Ozempic and is generally the first-line option for headache relief. The standard dose is 500-1000 mg up to four times daily, with a maximum of 4g in 24 hours and at least 4 hours between doses.
Should I stop taking Ozempic if I develop headaches?
Most headaches are mild and transient, so stopping Ozempic is not usually necessary. However, if headaches are severe, persistent beyond the first month, or accompanied by warning signs such as neurological symptoms, you should consult your prescribing clinician for assessment and potential treatment adjustment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript