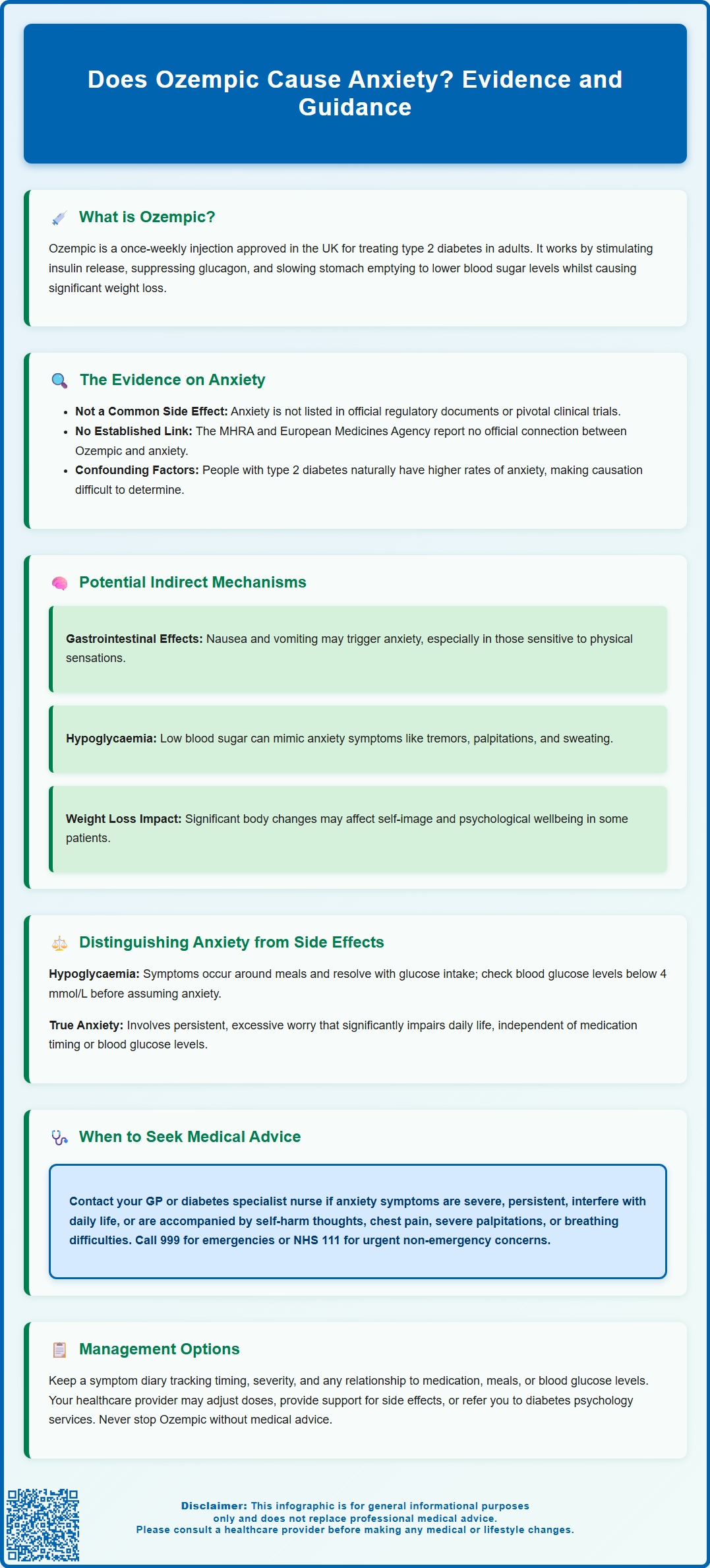
Ozempic (semaglutide) is a widely prescribed GLP-1 receptor agonist for type 2 diabetes management in the UK, but some patients wonder: does Ozempic cause anxiety? Whilst anxiety is not listed as a recognised side effect in official regulatory data from the MHRA or clinical trials, occasional patient reports have raised questions about this potential link. Understanding the evidence, distinguishing anxiety from other medication effects, and knowing when to seek medical advice are essential for anyone taking Ozempic. This article examines the current evidence, explores possible mechanisms, and provides practical guidance for patients and healthcare professionals.
Summary: Ozempic (semaglutide) is not officially recognised as causing anxiety based on current UK regulatory data and clinical trials, though occasional patient reports exist without established causation.
- Ozempic is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment, administered as a once-weekly subcutaneous injection.
- Anxiety does not appear in the MHRA-approved Summary of Product Characteristics or SUSTAIN clinical trial data as a significant adverse event.
- Gastrointestinal side effects and hypoglycaemia symptoms may mimic or indirectly contribute to anxiety-like experiences in some patients.
- Patients with type 2 diabetes have higher baseline rates of anxiety, making it difficult to distinguish medication effects from underlying psychological comorbidity.
- Report suspected side effects through the MHRA Yellow Card scheme and seek medical review if anxiety symptoms are severe, persistent, or accompanied by thoughts of self-harm.
Table of Contents
- Understanding Ozempic and Its Primary Uses
- Can Ozempic Cause Anxiety? Examining the Evidence
- Potential Mechanisms Linking Ozempic to Anxiety Symptoms
- Distinguishing Anxiety from Other Ozempic Side Effects
- When to Seek Medical Advice About Anxiety on Ozempic
- Scientific References
- Frequently Asked Questions
Understanding Ozempic and Its Primary Uses
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus in adults. Administered as a once-weekly subcutaneous injection, Ozempic works by mimicking the action of the naturally occurring hormone GLP-1, which plays a crucial role in glucose regulation and appetite control.
The medication's primary mechanism of action involves stimulating insulin secretion in a glucose-dependent manner, suppressing glucagon release, and slowing gastric emptying. These combined effects help to lower blood glucose levels and improve glycaemic control in people with type 2 diabetes. The Medicines and Healthcare products Regulatory Agency (MHRA) approved Ozempic for use alongside diet and exercise modifications, either as monotherapy when metformin is inappropriate or in combination with other glucose-lowering medications.
Treatment typically begins with a 0.25 mg weekly dose for 4 weeks, then increases to 0.5 mg weekly. If additional glycaemic control is needed, the dose may be increased to 1 mg weekly and up to a maximum of 2 mg weekly.
Beyond its glucose-lowering properties, Ozempic has gained considerable attention for its weight loss effects. Clinical trials have demonstrated significant reductions in body weight, which has led to increased prescribing for patients with type 2 diabetes who are also overweight or obese. The National Institute for Health and Care Excellence (NICE) recognises semaglutide's role in diabetes management, particularly for patients requiring additional glycaemic control or those who would benefit from weight reduction.
It is important to emphasise that Ozempic is indicated solely for type 2 diabetes treatment in the UK. While a higher-dose formulation of semaglutide (Wegovy) is specifically licensed for weight management, Ozempic should not be prescribed for weight loss alone. Understanding the medication's intended use provides essential context when evaluating potential side effects, including psychological symptoms such as anxiety.
Can Ozempic Cause Anxiety? Examining the Evidence
The question of whether Ozempic directly causes anxiety remains an area where clinical evidence is limited and somewhat inconclusive. Anxiety is not listed among the common adverse reactions in the official Summary of Product Characteristics (SmPC) approved by the MHRA, nor does it feature prominently in the pivotal clinical trials that led to the medication's approval.
In the SUSTAIN clinical trial programme, which evaluated semaglutide's efficacy and safety in thousands of patients with type 2 diabetes, anxiety was not reported as a statistically significant adverse event compared to placebo or active comparators. The most frequently documented side effects were gastrointestinal in nature, including nausea, vomiting, diarrhoea, and constipation. However, post-marketing surveillance and patient reports have occasionally mentioned anxiety-like symptoms, though establishing a definitive causal relationship remains challenging.
It is crucial to recognise that there is no official established link between Ozempic and anxiety based on current regulatory data. The European Medicines Agency (EMA) and MHRA continue to monitor adverse event reports, but anxiety has not been identified as a recognised side effect requiring specific labelling or warnings. Recent EMA Pharmacovigilance Risk Assessment Committee reviews of GLP-1 receptor agonists found no causal association with suicidal thoughts or self-harm, though monitoring continues.
Several factors complicate the assessment of this relationship. People with type 2 diabetes have higher baseline rates of anxiety and depression compared to the general population, making it difficult to distinguish medication effects from underlying psychological comorbidity. Additionally, the lifestyle changes, dietary modifications, and health concerns associated with diabetes management may independently contribute to anxiety symptoms, regardless of medication use.
Patients and healthcare professionals who suspect Ozempic may be causing anxiety or other side effects should report this through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Potential Mechanisms Linking Ozempic to Anxiety Symptoms
Whilst direct causation has not been established, several theoretical mechanisms might explain why some individuals report anxiety-like symptoms whilst taking Ozempic. Understanding these potential pathways can help patients and healthcare professionals contextualise such experiences.
Gastrointestinal side effects represent the most common adverse reactions to Ozempic and may indirectly contribute to anxiety. Persistent nausea, vomiting, or abdominal discomfort can be distressing and may trigger or exacerbate anxious feelings, particularly in individuals with pre-existing health anxiety or those sensitive to bodily sensations. The physical discomfort associated with these symptoms might be misinterpreted as anxiety or may genuinely provoke worry about one's health.
Hypoglycaemia can occur, though it is uncommon with Ozempic monotherapy. The risk increases significantly when Ozempic is used in combination with insulin or sulfonylureas. According to the SmPC, dose reductions of these medications should be considered when initiating Ozempic to reduce hypoglycaemia risk. Low blood glucose levels can produce symptoms that closely mimic anxiety, including tremor, palpitations, sweating, and feelings of apprehension. Patients may experience these physical sensations as anxiety when they are actually manifestations of hypoglycaemia.
The weight loss experienced by some patients on Ozempic may theoretically have psychological implications, though this remains speculative. Significant body composition changes could potentially affect self-image, energy levels, and overall wellbeing. Some individuals might find weight reduction unsettling or experience concerns about their changing appearance, though there is limited evidence directly linking this to anxiety symptoms.
Additionally, GLP-1 receptors are present in the central nervous system, including areas involved in mood regulation. Whilst the precise neuropsychiatric effects of GLP-1 receptor agonists remain under investigation, it is theoretically possible that modulation of these pathways could influence emotional states in susceptible individuals. This mechanism remains entirely speculative and requires further research before any conclusions can be drawn.
Distinguishing Anxiety from Other Ozempic Side Effects
Accurately identifying anxiety and differentiating it from other medication-related symptoms is essential for appropriate management. Several Ozempic side effects can mimic or overlap with anxiety symptoms, making clinical assessment important.
Hypoglycaemia symptoms warrant particular attention, as they can closely resemble anxiety. Both conditions may present with:
-
Trembling or shakiness
-
Rapid heartbeat or palpitations
-
Sweating
-
Feelings of nervousness or unease
-
Difficulty concentrating
The key distinction lies in timing and context. Hypoglycaemia typically occurs in relation to meals, physical activity, or medication timing, and symptoms resolve rapidly with glucose intake. Patients should check their blood glucose levels when experiencing these symptoms to rule out hypoglycaemia before attributing them to anxiety. In the UK, a reading below 4 mmol/L indicates hypoglycaemia and should be treated with 15-20g of fast-acting carbohydrate (e.g., glucose tablets, fruit juice), followed by rechecking after 10-15 minutes and a starchy snack if the next meal is not soon.
Gastrointestinal disturbances are the most common side effects of Ozempic and may contribute to general discomfort that patients describe as anxiety. Nausea, in particular, can create a sense of unease or worry about vomiting, especially in social situations. These symptoms typically emerge or worsen during treatment initiation and dose escalation, and often improve as the body adjusts to the medication over several weeks.
Cardiovascular symptoms such as increased heart rate have been observed with GLP-1 receptor agonists. A modest increase in resting heart rate (typically 2-3 beats per minute) is documented in clinical trials. Some patients may become aware of their heartbeat or experience palpitations, which can be misinterpreted as anxiety or may trigger health-related worry.
True anxiety disorders are characterised by persistent, excessive worry that is disproportionate to circumstances, often accompanied by physical symptoms, and significantly impairs daily functioning. If symptoms are genuinely anxiety-related rather than medication side effects, they typically persist beyond the immediate post-injection period and occur independently of blood glucose levels or gastrointestinal symptoms.
When to Seek Medical Advice About Anxiety on Ozempic
Patients experiencing anxiety-like symptoms whilst taking Ozempic should be encouraged to contact their GP or diabetes specialist nurse for assessment, particularly in certain circumstances that warrant prompt medical attention.
Immediate medical review is advisable if:
-
Anxiety symptoms are severe, persistent, or significantly impair daily activities, work, or relationships
-
Symptoms are accompanied by thoughts of self-harm or suicide
-
Physical symptoms such as chest pain, severe palpitations, or breathing difficulties occur
-
Suspected hypoglycaemia episodes are frequent or severe
-
Gastrointestinal side effects are intolerable or lead to dehydration
-
New or worsening depression accompanies anxiety symptoms
For severe symptoms or imminent risk, call 999 or attend A&E. For urgent but non-emergency concerns, contact NHS 111 or your local NHS mental health crisis service.
Routine discussion with healthcare professionals should occur if anxiety symptoms are mild to moderate but persistent beyond the initial adjustment period (typically 4-8 weeks). The prescribing clinician can assess whether symptoms might be related to the medication, underlying diabetes-related distress, or a separate anxiety disorder requiring specific treatment.
During consultations, patients should be prepared to discuss the timing, severity, and nature of symptoms, including any relationship to medication administration, meals, or blood glucose levels. Keeping a symptom diary can be helpful. Healthcare professionals may recommend blood glucose monitoring to exclude hypoglycaemia, review concomitant medications that might contribute to anxiety, and assess for other medical causes.
If recurrent hypoglycaemia occurs, review and consider reducing insulin or sulfonylurea doses under clinician guidance.
Management options may include dose adjustment, additional support for managing gastrointestinal side effects, referral to diabetes psychology services, or consideration of alternative diabetes medications if symptoms are genuinely medication-related and problematic. The NICE guideline on type 2 diabetes management emphasises individualised treatment approaches, and medication changes should always be made in consultation with the prescribing team.
Patients should not stop Ozempic without medical advice, as this may lead to deterioration in glycaemic control. A collaborative approach between patient and healthcare team ensures optimal diabetes management whilst addressing any psychological concerns that arise during treatment.
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Type 2 diabetes in adults: management.
- Ozempic - European Public Assessment Report.
- Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes (SUSTAIN-6).
- Low blood sugar (hypoglycaemia).
- Mechanisms of GLP-1 Receptor Agonist-Induced Weight Loss: A Review.
Frequently Asked Questions
Is anxiety a recognised side effect of Ozempic?
No, anxiety is not listed as a recognised side effect in the MHRA-approved product information or pivotal clinical trials for Ozempic. The most common adverse reactions are gastrointestinal, including nausea, vomiting, and diarrhoea.
Can Ozempic side effects mimic anxiety symptoms?
Yes, hypoglycaemia and gastrointestinal disturbances associated with Ozempic can produce symptoms that resemble anxiety, such as trembling, palpitations, sweating, and nervousness. Checking blood glucose levels helps distinguish hypoglycaemia from true anxiety.
When should I contact my GP about anxiety whilst taking Ozempic?
Contact your GP if anxiety symptoms are severe, persistent, impair daily functioning, or are accompanied by thoughts of self-harm, chest pain, severe palpitations, or frequent hypoglycaemia. For emergencies, call 999 or attend A&E.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript