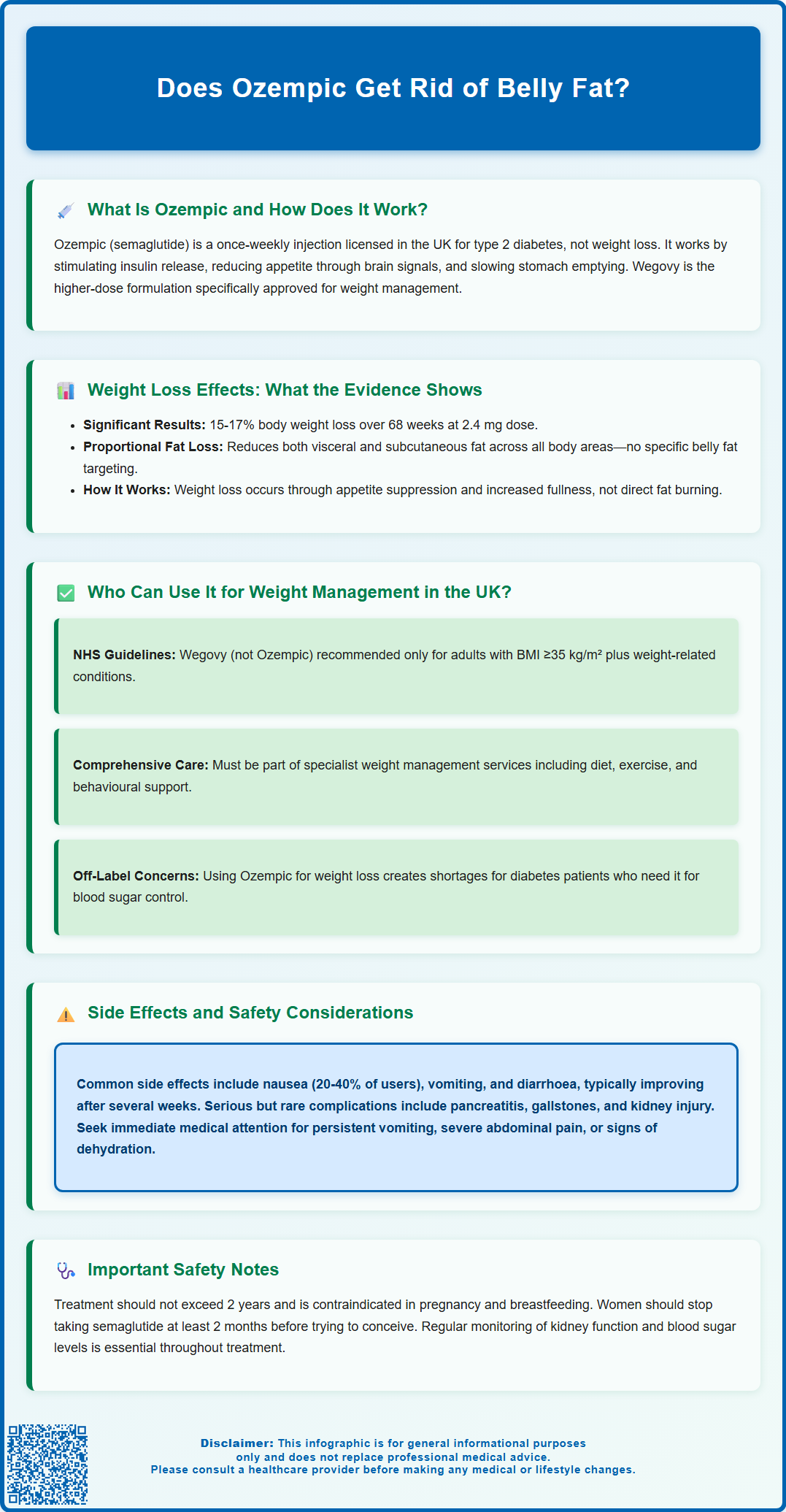
Many people wonder whether Ozempic can specifically target belly fat. Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for type 2 diabetes management, though it has gained attention for its weight loss effects. Whilst clinical evidence confirms that semaglutide reduces overall body weight—including abdominal fat—it does not selectively eliminate belly fat over other areas. Weight loss occurs proportionally across the body through appetite suppression and reduced caloric intake. Understanding how Ozempic works, who can appropriately use it, and what realistic outcomes to expect is essential for anyone considering this treatment.
Summary: Ozempic reduces overall body weight including abdominal fat, but does not selectively target belly fat over other body areas.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, not primarily for weight loss.
- Clinical trials show semaglutide reduces both visceral and subcutaneous fat proportionally across the body through appetite suppression.
- Wegovy (higher-dose semaglutide) is the MHRA-approved formulation for weight management in specialist services under NICE guidance.
- Common side effects include nausea, vomiting, and gastrointestinal symptoms, particularly during dose escalation.
- Serious but rare risks include pancreatitis, gallbladder disease, and hypoglycaemia when combined with other diabetes medications.
- Treatment requires regular monitoring of renal function and glycaemic control, with specialist oversight for weight management indications.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic is the brand name for semaglutide, a prescription medicine licensed in the UK by the Medicines and Healthcare products Regulatory Agency (MHRA) primarily for the treatment of type 2 diabetes mellitus. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which mimic the action of a naturally occurring hormone in the body.
The mechanism of action involves several physiological processes. Semaglutide works by:
-
Stimulating insulin secretion when blood glucose levels are elevated, helping to lower blood sugar
-
Suppressing glucagon release, which reduces glucose production by the liver
-
Slowing gastric emptying, meaning food stays in the stomach longer, promoting feelings of fullness
-
Acting on appetite centres in the brain, particularly in the hypothalamus, to reduce hunger and food intake
Ozempic is administered as a once-weekly subcutaneous injection, typically starting at a low dose (0.25 mg) for initiation only, then gradually increasing to therapeutic doses of 0.5 mg, 1 mg, or 2 mg, depending on individual response and tolerability. The slow titration helps minimise gastrointestinal side effects.
If planning pregnancy, semaglutide should be discontinued at least 2 months before a planned conception. It is contraindicated during pregnancy and not recommended during breastfeeding.
Weight Loss Effects: What the Evidence Shows
Clinical trial evidence demonstrates that semaglutide does lead to significant weight reduction, though it is important to clarify what this means for body composition, particularly abdominal or 'belly' fat. The landmark STEP (Semaglutide Treatment Effect in People with obesity) trials showed that participants using semaglutide 2.4 mg weekly (Wegovy) achieved average weight loss of approximately 15-17% of their initial body weight over 68 weeks, compared to 2-3% with placebo. The lower doses used in Ozempic for diabetes (0.5-2 mg) typically result in less weight loss than the 2.4 mg dose.
Regarding fat distribution specifically, research indicates that weight loss with GLP-1 receptor agonists results in reductions across multiple fat compartments, including:
-
Visceral adipose tissue (fat surrounding internal organs in the abdomen)
-
Subcutaneous fat (fat beneath the skin, including abdominal areas)
-
Overall body fat percentage
Imaging studies using MRI and CT scans have confirmed that semaglutide treatment leads to meaningful reductions in visceral fat, which is metabolically significant as this type of fat is associated with increased cardiovascular and metabolic risk. However, there is no official evidence that semaglutide selectively targets belly fat over other areas—weight loss occurs proportionally across the body.
The weight reduction observed is primarily attributed to decreased caloric intake resulting from appetite suppression and increased satiety, rather than any direct fat-burning mechanism. Patients typically report feeling fuller sooner during meals and experiencing reduced food cravings between meals. It is worth noting that individual responses vary considerably, and not all patients achieve the average weight loss seen in clinical trials. Lifestyle factors, including diet quality and physical activity, continue to play important roles in overall outcomes.
Who Can Use Ozempic for Weight Management in the UK?
In the UK, prescribing guidelines are clear regarding who can appropriately receive semaglutide for weight management. Ozempic itself is licensed only for type 2 diabetes, not for weight loss as a primary indication. For weight management specifically, Wegovy (the higher-dose semaglutide formulation) is the appropriate licensed product.
According to NICE guidance (TA875), Wegovy is recommended for weight management only within specialist weight management services, and specifically for adults with:
-
BMI ≥35 kg/m² with at least one weight-related comorbidity
-
Lower BMI thresholds (typically by 2.5 kg/m²) may apply for people from some minority ethnic groups
Treatment should be initiated only as part of a comprehensive weight management programme that includes dietary modification, increased physical activity, and behavioural support. NICE recommends that treatment should be provided for a maximum of 2 years.
While the product licence for Wegovy is broader (including BMI ≥30 kg/m² with comorbidities), NHS commissioning follows the more specific NICE criteria above.
Ozempic or Wegovy should not be used in individuals with:
-
Pregnancy or breastfeeding
-
Severe gastrointestinal disease
-
History of pancreatitis (requires careful assessment)
The UK product information notes that animal studies have shown an increased incidence of thyroid C-cell tumours with semaglutide, though the human relevance of this finding is unknown. Patients should report any symptoms such as a lump in the neck, persistent hoarseness, or difficulty swallowing.
It is important to note that obtaining Ozempic through private prescriptions solely for weight loss, when not indicated for diabetes, raises ethical and supply concerns. The NHS has experienced significant shortages of diabetes medications due to off-label demand for weight loss, potentially affecting patients who genuinely require these medicines for glycaemic control. Patients interested in medical weight management should consult their GP to discuss appropriate, evidence-based options within licensed indications.
Side Effects and Safety Considerations
Like all medications, semaglutide carries a risk of adverse effects, which patients should understand before starting treatment. The most commonly reported side effects are gastrointestinal in nature and include:
-
Nausea (affecting up to 20-40% of users, particularly during dose escalation)
-
Vomiting and diarrhoea
-
Constipation
-
Abdominal pain and bloating
-
Reduced appetite (which, whilst therapeutically desired, can be excessive in some individuals)
-
Headache and dizziness
-
Injection site reactions (redness, swelling or itching)
These effects are typically most pronounced when initiating therapy or increasing doses, which is why gradual titration is recommended. Most gastrointestinal symptoms improve over several weeks as the body adjusts, though some patients find them intolerable and discontinue treatment.
More serious but less common adverse effects include:
-
Pancreatitis: Patients should seek immediate medical attention if experiencing severe, persistent abdominal pain radiating to the back
-
Gallbladder disease: Rapid weight loss can increase the risk of gallstones
-
Hypoglycaemia: Particularly when used alongside other diabetes medications such as sulphonylureas or insulin
-
Diabetic retinopathy complications: Rapid improvement in blood glucose control may temporarily worsen retinopathy in susceptible individuals
-
Acute kidney injury: Usually in the context of dehydration from vomiting or diarrhoea
Animal studies have shown an increased incidence of thyroid C-cell tumours with semaglutide, though the human relevance of this finding is unknown. Patients should report any symptoms such as a lump in the neck, persistent hoarseness, or difficulty swallowing.
Patients should contact their GP if they experience:
-
Persistent vomiting preventing fluid intake
-
Severe abdominal pain
-
Signs of dehydration (dark urine, dizziness, reduced urination)
-
Symptoms of hypoglycaemia (tremor, sweating, confusion)
-
Visual changes
-
Symptoms of pancreatitis or gallbladder inflammation
Regular monitoring is essential, including renal function tests and, for those with diabetes, ongoing assessment of glycaemic control and adjustment of other diabetes medications as needed. Patients should report any suspected side effects to their healthcare professional or directly to the MHRA through the Yellow Card Scheme at yellowcard.mhra.gov.uk.
Frequently Asked Questions
Can I get Ozempic on the NHS for weight loss?
Ozempic is licensed only for type 2 diabetes on the NHS. For weight management, Wegovy (higher-dose semaglutide) is available through specialist weight management services under NICE guidance for adults with BMI ≥35 kg/m² and weight-related comorbidities.
How much weight can you lose with Ozempic?
Clinical trials show that higher-dose semaglutide (Wegovy 2.4 mg) results in average weight loss of approximately 15-17% of initial body weight over 68 weeks. Lower Ozempic doses for diabetes typically produce less weight loss, with individual responses varying considerably.
What are the most common side effects of Ozempic?
The most common side effects are gastrointestinal, including nausea (affecting 20-40% of users), vomiting, diarrhoea, constipation, and abdominal pain. These symptoms are typically most pronounced during dose escalation and often improve over several weeks.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript