Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus in adults. Whilst this once-weekly injectable medication is associated with various side effects—predominantly gastrointestinal—photosensitivity is not recognised as an established adverse reaction in UK regulatory guidance or clinical trial data. Understanding the actual side effect profile of Ozempic, alongside general sun safety principles for people with diabetes, helps patients make informed decisions about their treatment and skin care practices.
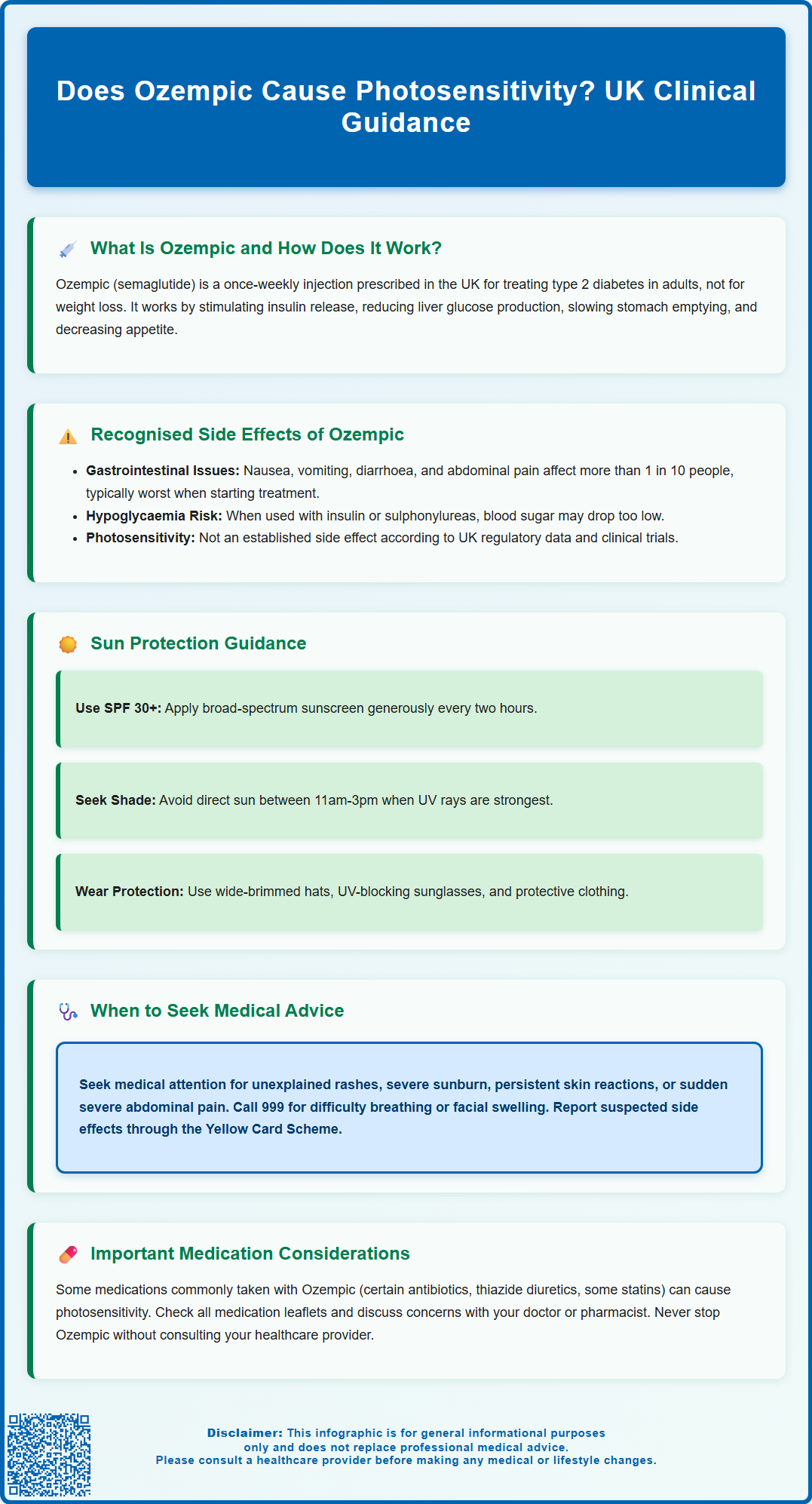
Summary: Ozempic (semaglutide) is not recognised as causing photosensitivity according to UK regulatory guidance, clinical trials, or the Summary of Product Characteristics.
- Ozempic is a GLP-1 receptor agonist licensed for type 2 diabetes treatment, administered as a once-weekly subcutaneous injection.
- The most common side effects are gastrointestinal (nausea, vomiting, diarrhoea, abdominal pain), typically diminishing over time.
- Photosensitivity is not listed among known adverse effects in UK product information or MHRA guidance.
- People with diabetes should maintain good sun protection practices regardless, as diabetes itself can affect skin health and healing.
- Any unusual skin reactions whilst taking Ozempic should be reported to a healthcare professional and documented via the Yellow Card Scheme.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that helps regulate blood sugar levels.
The mechanism of action involves several complementary effects:
-
Stimulating insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released only when blood sugar levels are elevated
-
Suppressing glucagon release, which reduces glucose production by the liver
-
Slowing gastric emptying, which helps moderate the rise in blood sugar after meals
-
Reducing appetite through effects on brain centres that regulate hunger
Ozempic is administered as a once-weekly subcutaneous injection using a pre-filled pen device. The usual starting dose is 0.25 mg once weekly for four weeks as an initiation dose only (not for glycaemic control). The maintenance dose begins at 0.5 mg weekly. Depending on glycaemic control and tolerability, the dose may be further increased to 1 mg weekly, with a maximum dose of 2 mg weekly available if needed.
According to NICE guidance (NG28), GLP-1 receptor agonists like Ozempic are typically considered for people with type 2 diabetes who have inadequate glycaemic control despite treatment with metformin and other oral medications, or when other treatment options are contraindicated or not tolerated. The medication has demonstrated significant benefits in reducing HbA1c levels and can promote weight loss as a secondary effect, though it's important to note that Ozempic is not licensed for weight management in the UK (Wegovy is the semaglutide product licensed for weight management).
Ozempic is not indicated for patients with type 1 diabetes or for the treatment of diabetic ketoacidosis.
Recognised Side Effects of Ozempic in the UK
Like all medications, Ozempic can cause side effects, though not everyone experiences them. The Medicines and Healthcare products Regulatory Agency (MHRA) and the Summary of Product Characteristics (SmPC) for Ozempic list a comprehensive range of potential adverse reactions based on clinical trial data and post-marketing surveillance.
The most commonly reported side effects (affecting more than 1 in 10 people) are gastrointestinal in nature and include:
-
Nausea and vomiting
-
Diarrhoea
-
Abdominal pain
-
Constipation
These effects are typically most pronounced when starting treatment or increasing the dose, and often diminish over time as the body adjusts to the medication.
Important safety warnings include:
-
Acute pancreatitis: Seek urgent medical care if you experience sudden, severe and persistent abdominal pain (which may radiate to your back), with or without vomiting
-
Diabetic retinopathy complications: Patients with pre-existing retinopathy should be monitored closely, especially during rapid improvement in blood glucose control
-
Dehydration risk: The gastrointestinal side effects may cause dehydration, potentially leading to acute kidney injury; maintaining adequate fluid intake is important
When Ozempic is used with insulin or sulphonylureas, there is an increased risk of hypoglycaemia, and doses of these medications may need to be reduced when starting Ozempic.
Regarding photosensitivity specifically—an increased sensitivity of the skin to sunlight that can result in exaggerated sunburn, rashes, or other skin reactions—there is no official link established between Ozempic and photosensitivity in the UK product information or regulatory guidance. Photosensitivity is not listed among the known adverse effects in the SmPC, and clinical trials have not identified this as a significant concern.
However, it is important to note that diabetes itself can affect skin health, and people with diabetes may be more susceptible to various skin conditions. Additionally, individual responses to medications can vary, and any unusual skin reactions should be reported to a healthcare professional for proper assessment and documentation.
Managing Sun Exposure While Taking Ozempic
Although photosensitivity is not a recognised side effect of Ozempic, good sun protection practices remain important for everyone, particularly for people with diabetes who may already have compromised skin integrity or delayed wound healing.
General sun safety recommendations that apply to all patients include:
-
Using broad-spectrum sunscreen with SPF 30 or higher and UVA protection (4-5 star rating) on exposed skin, applied generously and reapplied every two hours or after swimming or sweating
-
Seeking shade during peak sun intensity hours (typically 11am to 3pm in the UK)
-
Wearing protective clothing such as wide-brimmed hats, long-sleeved shirts, and sunglasses with UV protection
-
Being particularly cautious during holidays abroad or at higher altitudes where UV exposure is more intense
For people with diabetes specifically, additional skin care considerations include:
-
Maintaining good glycaemic control, as elevated blood sugar levels can impair skin health and healing
-
Keeping skin well-moisturised to prevent dryness and cracking
-
Inspecting skin regularly for any changes, cuts, or infections
-
Ensuring adequate hydration, particularly in hot weather
If you notice any unusual skin reactions whilst taking Ozempic—whether related to sun exposure or not—it is advisable to document when they occur, their appearance, and any potential triggers. Taking photographs can be helpful for showing your healthcare provider at your next appointment.
Patients should also be aware that some other medications commonly used alongside Ozempic for diabetes or related conditions may cause photosensitivity. These include certain antibiotics (such as tetracyclines), thiazide diuretics, and rarely, some statins. Always check the patient information leaflet for all your medications and discuss any concerns with your GP or pharmacist.
When to Seek Medical Advice About Skin Reactions
Whilst Ozempic is not known to cause photosensitivity, any new or concerning skin changes warrant medical attention, particularly for people with diabetes who may be at increased risk of skin complications.
You should contact your GP or diabetes specialist nurse if you experience:
-
Unexplained rashes, blistering, or skin discolouration
-
Severe sunburn that seems disproportionate to sun exposure
-
Skin reactions that appear shortly after sun exposure and persist
-
Any skin changes accompanied by fever, malaise, or feeling generally unwell
-
Injection site reactions that worsen, spread, or do not resolve within a few days
-
Signs of skin infection such as increasing redness, warmth, swelling, or pus
Seek urgent medical attention if you develop:
-
Call 999 for symptoms of severe allergic reaction (anaphylaxis) including difficulty breathing, swelling of the face, tongue or throat
-
Contact 111 or attend A&E for blistering or peeling skin affecting large areas of the body
-
Skin changes accompanied by severe pain or systemic symptoms
For other serious Ozempic side effects, seek urgent medical care if you experience sudden, severe and persistent abdominal pain (which may radiate to your back), with or without vomiting, as this could indicate acute pancreatitis.
It is important to remember that the Yellow Card Scheme, operated by the MHRA, allows patients and healthcare professionals to report suspected side effects from medications. You can report via the website (yellowcard.mhra.gov.uk) or the Yellow Card app. If you believe you are experiencing an adverse reaction to Ozempic that is not listed in the patient information leaflet, reporting it helps regulatory authorities monitor medication safety and identify previously unrecognised effects.
Your healthcare team can assess whether skin symptoms are related to Ozempic, diabetes itself, another medication, or an unrelated dermatological condition. They may adjust your treatment, provide symptomatic relief, or refer you to a dermatologist if specialist assessment is needed. Never stop taking Ozempic without consulting your doctor, as abrupt discontinuation could affect your diabetes control. Any concerns about side effects should be discussed with your healthcare provider, who can help weigh the benefits and risks of continuing treatment and explore alternative management strategies if necessary.
Frequently Asked Questions
Is photosensitivity a recognised side effect of Ozempic in the UK?
No, photosensitivity is not listed as a known adverse effect of Ozempic (semaglutide) in UK regulatory guidance, the Summary of Product Characteristics, or clinical trial data. The most common side effects are gastrointestinal in nature.
What are the most common side effects of Ozempic?
The most common side effects of Ozempic affect more than 1 in 10 people and are gastrointestinal, including nausea, vomiting, diarrhoea, abdominal pain, and constipation. These typically diminish as the body adjusts to the medication.
Should I report unusual skin reactions whilst taking Ozempic?
Yes, any new or unusual skin reactions should be reported to your GP or diabetes specialist nurse for proper assessment. You can also report suspected side effects via the MHRA Yellow Card Scheme to help monitor medication safety.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












