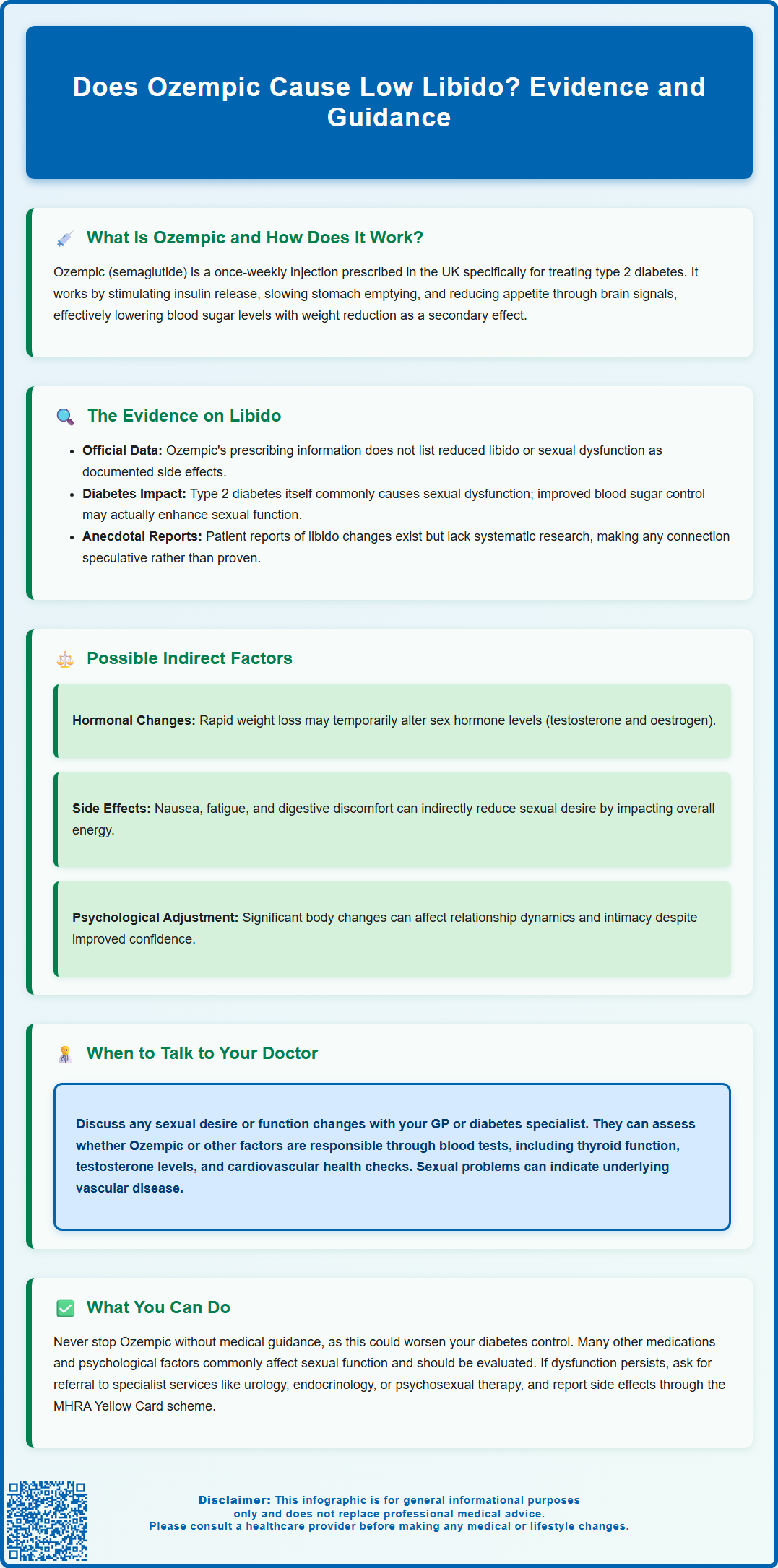
Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, administered as a weekly injection to improve blood glucose control. Some patients have questioned whether Ozempic causes low libido, though this side effect is not documented in official prescribing information or clinical trial data. Sexual function is influenced by multiple factors including diabetes itself, metabolic changes, hormonal fluctuations, and psychological wellbeing. Understanding the relationship between Ozempic and libido requires careful consideration of both direct pharmacological effects and indirect mechanisms. This article examines the available evidence and provides guidance for patients experiencing sexual health concerns during treatment.
Summary: Ozempic is not established to directly cause low libido, as sexual dysfunction is not listed among documented side effects in clinical trials or UK prescribing information.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed for type 2 diabetes, administered weekly by subcutaneous injection.
- Sexual dysfunction including reduced libido is not documented in the MHRA-approved Summary of Product Characteristics or clinical trial data.
- Indirect mechanisms such as rapid weight loss, hormonal changes, gastrointestinal side effects, and psychological adjustment may theoretically influence sexual function.
- Type 2 diabetes itself is strongly associated with sexual dysfunction; improved glycaemic control may enhance rather than impair sexual health over time.
- Patients experiencing libido changes should discuss concerns with their GP, undergo appropriate assessment including blood tests, and not discontinue treatment without medical guidance.
- Suspected side effects should be reported through the MHRA Yellow Card scheme to support ongoing medication safety monitoring.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic is the brand name for semaglutide, a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a class of medicines called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone in the body that regulates blood glucose levels and appetite.
The medication is administered as a once-weekly subcutaneous injection, typically into the abdomen, thigh, or upper arm. Semaglutide works through several complementary mechanisms: it stimulates insulin secretion from the pancreas when blood glucose levels are elevated, suppresses the release of glucagon (a hormone that raises blood sugar), slows gastric emptying to reduce post-meal glucose spikes, and acts on appetite centres in the brain to promote satiety and reduce food intake.
Ozempic has been shown in clinical trials to effectively lower HbA1c levels and support weight reduction in people with type 2 diabetes, though it's important to note that weight loss is an observed effect rather than the licensed indication in the UK. The Medicines and Healthcare products Regulatory Agency (MHRA) approved semaglutide for diabetes management, and NICE guidelines (NG28) recommend GLP-1 receptor agonists as part of a comprehensive treatment strategy for appropriate patients. The medication is typically initiated at a low dose of 0.25 mg weekly, with gradual titration to therapeutic doses of 0.5 mg, 1 mg, or 2 mg weekly, depending on individual response and tolerability. This gradual dose escalation helps minimise common gastrointestinal side effects such as nausea and vomiting, which are most pronounced during the initial treatment phase.
Can Ozempic Cause Low Libido or Sexual Side Effects?
There is currently no established direct link between Ozempic and reduced libido in the official prescribing information or clinical trial data. Sexual dysfunction, including decreased libido, is not listed among the common or uncommon adverse effects in the Summary of Product Characteristics (SmPC) approved by the MHRA. The primary side effects documented in clinical trials predominantly involve gastrointestinal symptoms, including nausea, vomiting, diarrhoea, and constipation.
However, it is important to recognise that sexual function is influenced by multiple interconnected factors, and changes in libido can occur through indirect mechanisms. Type 2 diabetes itself is strongly associated with sexual dysfunction in both men and women, with studies indicating that improved glycaemic control and metabolic health may actually enhance sexual function over time. The substantial weight loss that many patients experience whilst taking Ozempic could theoretically influence hormone levels, body image, and overall wellbeing, all of which play roles in sexual desire.
Anecdotal reports from some patients have suggested changes in libido during treatment with GLP-1 receptor agonists, though these observations have not been systematically studied or confirmed in controlled research. It remains unclear whether such reports reflect a direct pharmacological effect, consequences of rapid metabolic changes, psychological adjustments to weight loss, or coincidental factors. The absence of robust clinical evidence means that any potential connection between Ozempic and libido changes remains speculative. Patients experiencing concerning symptoms should discuss them with their healthcare provider rather than assuming a causal relationship, and consider reporting suspected side effects through the MHRA Yellow Card scheme. It's also worth noting that erectile dysfunction in people with diabetes can be an indicator of cardiovascular disease risk and warrants appropriate assessment.
Why Might Ozempic Affect Sexual Function?
Whilst there is no confirmed direct mechanism by which Ozempic causes sexual dysfunction, several theoretical pathways warrant consideration. Rapid weight loss, which is common with semaglutide treatment, may temporarily alter sex hormone levels, particularly in individuals with significant adipose tissue loss. Adipose tissue plays a role in hormone metabolism, and substantial changes in body composition may influence testosterone and oestrogen levels, potentially affecting libido in both men and women. Some studies suggest that weight loss in obese men can lead to increased testosterone levels, though these changes vary considerably between individuals.
The gastrointestinal side effects associated with Ozempic, particularly nausea, fatigue, and reduced appetite, may indirectly impact sexual desire by affecting overall wellbeing and energy levels. When patients feel unwell or experience persistent digestive discomfort, it is not uncommon for sexual interest to diminish as a secondary consequence. Additionally, the psychological adjustment to significant body changes can be complex; whilst many people experience improved confidence and body image with weight loss, others may find the transition challenging or experience relationship dynamics shifts that affect intimacy.
Type 2 diabetes itself is a well-established risk factor for sexual dysfunction through multiple mechanisms, including vascular damage, neuropathy, and hormonal imbalances. Improved diabetes control achieved through Ozempic treatment might be expected to enhance rather than impair sexual function over time. However, the timeline of metabolic improvement may not align with immediate symptomatic relief, and some patients may experience a temporary dip in wellbeing during the adjustment period. It is also worth noting that many individuals with type 2 diabetes take multiple medications, and polypharmacy can complicate the attribution of any particular symptom to a single agent. No causal mechanism between GLP-1 receptor agonists and reduced libido has been demonstrated in clinical research to date.
What to Do If You Experience Low Libido on Ozempic
If you notice a reduction in sexual desire or function after starting Ozempic, it is important to discuss this openly with your GP or diabetes specialist nurse. Sexual health is an integral component of overall wellbeing, and healthcare professionals are accustomed to addressing these concerns in a sensitive, confidential manner. Your clinician will want to explore the timeline of symptom onset, the severity of changes, and any other concurrent symptoms or life circumstances that might be contributing factors.
A thorough assessment should include consideration of alternative explanations for reduced libido. Your doctor may wish to check relevant blood tests, including thyroid function, morning total testosterone levels in men (with repeat testing if low, and possibly SHBG, LH/FSH, and prolactin where indicated), and markers of diabetes control such as HbA1c. For erectile dysfunction specifically, cardiovascular risk assessment (including blood pressure, lipid profile, and QRISK calculation) is recommended, as sexual problems can be an early indicator of vascular disease. Other medications you are taking should be reviewed, as numerous drugs commonly prescribed for diabetes-related conditions—including certain antihypertensives, antidepressants, and lipid-lowering agents—are known to affect sexual function. Psychological factors, including stress, depression, anxiety, and relationship issues, are common contributors to changes in libido and should be explored.
Do not discontinue Ozempic without medical guidance, as this could compromise your diabetes management and potentially lead to deterioration in glycaemic control. Your healthcare team can help you weigh the benefits of continued treatment against any troublesome side effects. In some cases, adjusting the dose, allowing more time for adaptation, or addressing contributing factors may resolve the issue. If sexual dysfunction persists and is significantly affecting quality of life, your doctor may discuss alternative diabetes treatment options or refer you to specialist services, such as urology (for persistent erectile dysfunction), endocrinology (for hormonal abnormalities), or psychosexual therapy via NHS services. Consider reporting any suspected side effects to the MHRA through the Yellow Card scheme, which helps monitor medication safety. Remember that effective diabetes management and sexual health are both achievable goals, and open communication with your healthcare team is essential to finding the right balance for your individual circumstances.
Scientific References
- Type 2 diabetes in adults: management.
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Erectile dysfunction: avanafil - Full evidence summary (ESNM45).
- Erectile dysfunction (impotence).
- Prescribing semaglutide for weight loss in non-diabetic, obese patients.
- Weight loss response to semaglutide in postmenopausal women.
Frequently Asked Questions
Is low libido a documented side effect of Ozempic?
No, reduced libido is not listed among the documented side effects in Ozempic's MHRA-approved prescribing information or clinical trial data. The primary side effects are gastrointestinal, including nausea, vomiting, and diarrhoea.
Can weight loss from Ozempic affect sexual function?
Rapid weight loss may theoretically influence sex hormone levels and body image, which could indirectly affect libido. However, no direct causal mechanism has been established in clinical research, and improved metabolic health often enhances sexual function over time.
What should I do if I experience reduced libido whilst taking Ozempic?
Discuss your concerns openly with your GP or diabetes specialist, who can assess alternative causes, review blood tests including hormone levels, and evaluate other medications. Do not stop Ozempic without medical guidance, and consider reporting the symptom through the MHRA Yellow Card scheme.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript