Glucagon-like peptide-1 (GLP-1) receptor agonists, such as semaglutide (Ozempic, Wegovy) and liraglutide (Victoza, Saxenda), are widely prescribed for type 2 diabetes and weight management. Whilst these medications effectively reduce appetite and improve blood glucose control, some people report changes in taste perception and food preferences during treatment. Does GLP-1 change your taste? Emerging evidence suggests that GLP-1 therapy may alter how certain foods taste or appeal to you, though individual experiences vary considerably. Understanding these potential effects helps patients and clinicians manage treatment more effectively and maintain adequate nutrition throughout therapy.
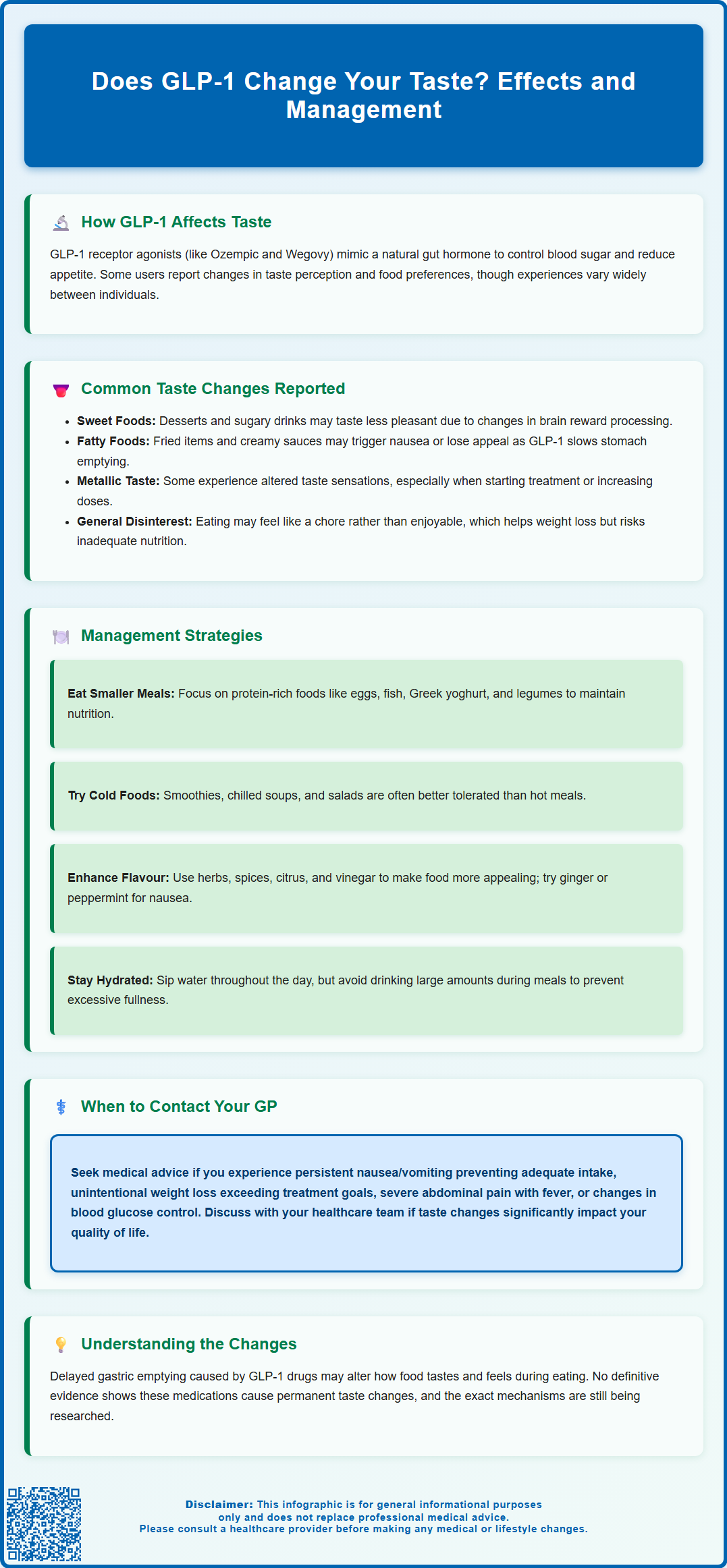
Summary: GLP-1 receptor agonists may alter taste perception and food preferences in some individuals, though experiences vary and mechanisms remain under investigation.
- GLP-1 medications work by mimicking gut hormones that regulate insulin secretion, slow gastric emptying, and reduce appetite through central nervous system effects.
- Some patients report reduced appeal of sweet or fatty foods, metallic taste sensations, or general food aversion, particularly during initial treatment or dose escalation.
- Taste changes may relate to delayed gastric emptying, GLP-1 receptor activity in taste buds and brain reward centres, or accompanying gastrointestinal symptoms like nausea.
- Management strategies include smaller frequent meals, texture modifications, adequate hydration, and gradual dose titration under medical supervision.
- Contact your GP if taste changes cause persistent vomiting, dehydration, excessive weight loss, severe abdominal pain, or significantly impact nutritional status or quality of life.
Table of Contents
How GLP-1 Medications Affect Taste and Food Preferences
Glucagon-like peptide-1 (GLP-1) receptor agonists, including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda), are increasingly prescribed for type 2 diabetes management and weight loss. These medications work by mimicking the action of naturally occurring GLP-1, a hormone released from the gut after eating. GLP-1 receptor agonists enhance insulin secretion in response to elevated blood glucose, suppress glucagon release, slow gastric emptying, and reduce appetite through effects on the central nervous system.
Whilst the primary mechanisms of GLP-1 drugs are well established, some people report changes in their taste perception and food preferences. The exact pathways remain under investigation, with several hypotheses being explored. Delayed gastric emptying may alter the sensory experience of eating, as food remains in the stomach longer, potentially affecting flavour perception and satiety signals. Research suggests GLP-1 receptors may be present in taste buds and throughout the gastrointestinal tract, though this evidence is primarily from preclinical studies.
Some individuals describe changes in their relationship with food beyond simple appetite suppression. These include altered taste sensitivity, particularly to sweet or fatty foods, whilst others note a general reduction in food appeal. These changes may be partly neurological, as GLP-1 receptors in the brain's reward centres could modify how pleasurable certain foods feel. It is important to note that there is no definitive evidence establishing a permanent taste alteration with GLP-1 therapy, and individual experiences vary considerably. Understanding these potential effects helps patients and clinicians anticipate and manage treatment-related changes effectively.
Taste Changes Some People Report While Taking GLP-1 Medicines
Some people taking GLP-1 medications report changes in how food tastes or appeals to them. Reduced appeal of sweet foods is one such change. Some patients describe previously enjoyed desserts, chocolate, or sugary beverages as less palatable or even unpleasant. This phenomenon may reflect changes in reward processing rather than true taste dysfunction, as the hedonic value of sweet foods appears diminished.
Aversion to fatty or rich foods is another observation. Some patients find that meals high in fat—such as fried foods, creamy sauces, or fatty meats—trigger nausea or simply lose their appeal. This effect likely relates to delayed gastric emptying, as high-fat foods naturally slow digestion further, potentially causing discomfort or early satiety. A smaller number of individuals report a metallic or altered taste sensation, particularly during the initial weeks of treatment or following dose escalation. If you experience persistent taste changes, it's worth discussing with your healthcare provider as other factors (such as medications, dental issues, or nutritional deficiencies) could also contribute.
Additionally, some patients experience general food aversion or disinterest, where eating feels more like a chore than a pleasure. This extends beyond specific tastes to encompass reduced motivation to eat altogether. Some describe feeling indifferent to foods they once craved, which can be both beneficial for weight management and concerning if it leads to inadequate nutrition.
Gastrointestinal symptoms—including nausea, bloating, and reflux—frequently accompany GLP-1 therapy and can indirectly affect taste perception. When feeling nauseated, most foods become less appealing, and certain smells or flavours may trigger discomfort. These effects are typically dose-dependent and often improve with continued treatment as the body adapts to the medication, particularly if the dose is increased gradually as recommended.
Managing Taste Alterations While on GLP-1 Treatment
If you experience taste changes whilst taking GLP-1 medication, several practical strategies can help maintain adequate nutrition and treatment adherence. Dietary adjustments form the cornerstone of management. Focus on smaller, more frequent meals rather than large portions, as this approach aligns with the medication's effect on gastric emptying and can reduce nausea. Choose foods that remain palatable to you, even if your preferences have shifted. Many patients find success with protein-rich options such as eggs, fish, lean poultry, Greek yoghurt, and legumes, which support satiety without excessive fat content.
Texture and temperature modifications can improve food tolerance. Cold or room-temperature foods are often better tolerated than hot meals when nausea is present. Smoothies, chilled soups, and salads may be more appealing than cooked dishes. Experiment with different textures—some patients prefer softer foods, whilst others find crunchy vegetables more satisfying. Flavour enhancement through herbs, spices, citrus, and vinegar can make meals more interesting without adding unwanted sweetness or fat. Ginger and peppermint may also help settle the stomach.
Maintaining adequate hydration is essential, particularly if food intake decreases. Sip water throughout the day, and consider sugar-free electrolyte drinks or oral rehydration solutions if you're experiencing vomiting or significant fluid loss. Avoid drinking large volumes with meals, as this can increase feelings of fullness and discomfort.
Timing your medication appropriately may help with side effects for some people. For daily GLP-1 medications, taking them in the evening might help you sleep through peak nausea periods, though this effect may be limited for weekly injections due to their long half-life. Avoiding large or high-fat meals, alcohol, and rich foods around dosing days may also improve tolerance. If taste changes significantly impact your quality of life or nutritional status, discuss dose adjustment with your prescriber. Sometimes a slower titration schedule or lower maintenance dose can improve tolerability whilst preserving therapeutic benefits. Never adjust your dose without medical guidance. If your food intake is poor, ask about referral to a registered dietitian for specialist support.
When to Speak to Your GP About Taste Changes on GLP-1 Therapy
Whilst mild taste alterations are sometimes reported with GLP-1 therapy and often manageable, certain situations warrant medical review. Contact your GP or diabetes specialist nurse if taste changes are accompanied by persistent nausea or vomiting that prevents you from maintaining adequate fluid and food intake. Dehydration and malnutrition can develop quickly, particularly in older adults or those with other health conditions. Warning signs include dark urine, reduced urine output, dizziness, confusion, or inability to keep down fluids for more than 24 hours.
Unintentional weight loss beyond your treatment goals requires assessment. Whilst weight reduction is often a desired outcome, excessive or rapid loss may indicate inadequate caloric intake or an underlying problem. NICE guidance emphasises the importance of monitoring nutritional status during weight management interventions. Your healthcare team can assess whether your current regimen remains appropriate or requires modification.
Seek urgent medical advice if you develop severe or persistent abdominal pain, especially if accompanied by nausea, vomiting, or fever. Although rare, GLP-1 medications carry a small risk of pancreatitis, which requires prompt evaluation. Similarly, seek medical attention for symptoms of gallbladder disease, including pain in the upper right abdomen, fever, or yellowing of the skin or eyes (jaundice). New or worsening reflux symptoms that don't respond to simple measures should be discussed, as GLP-1 medications are not recommended in severe gastrointestinal disease.
Changes in blood glucose control warrant review, particularly for patients with diabetes. Reduced food intake can increase hypoglycaemia risk, especially if you take other glucose-lowering medications such as sulphonylureas or insulin. Your prescriber may need to adjust these medications to maintain safe glucose levels.
Finally, if taste changes significantly affect your quality of life or mental wellbeing, don't hesitate to raise this with your healthcare team. Treatment should improve your overall health, not diminish your enjoyment of life. Alternative GLP-1 formulations, dose adjustments, or different therapeutic approaches may be more suitable for your individual circumstances. Your GP can also refer you to a dietitian for specialist nutritional support if needed. For urgent but non-emergency advice, contact NHS 111, or call 999 for severe, life-threatening symptoms. If you suspect you're experiencing side effects from your medication, you can report these through the MHRA Yellow Card scheme.
Frequently Asked Questions
Why do some foods taste different on GLP-1 medication?
GLP-1 medications slow gastric emptying and may affect GLP-1 receptors in taste buds and brain reward centres, potentially altering how sweet or fatty foods taste and how pleasurable they feel. Accompanying nausea can also reduce food appeal.
Are taste changes from GLP-1 therapy permanent?
There is no definitive evidence that GLP-1 medications cause permanent taste alterations. Most taste changes are temporary and often improve as your body adapts to treatment, particularly with gradual dose escalation.
When should I contact my GP about taste changes on GLP-1 treatment?
Contact your GP if taste changes prevent adequate food or fluid intake, cause unintentional weight loss beyond treatment goals, accompany severe abdominal pain, or significantly affect your quality of life. Persistent vomiting or signs of dehydration require prompt medical review.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












