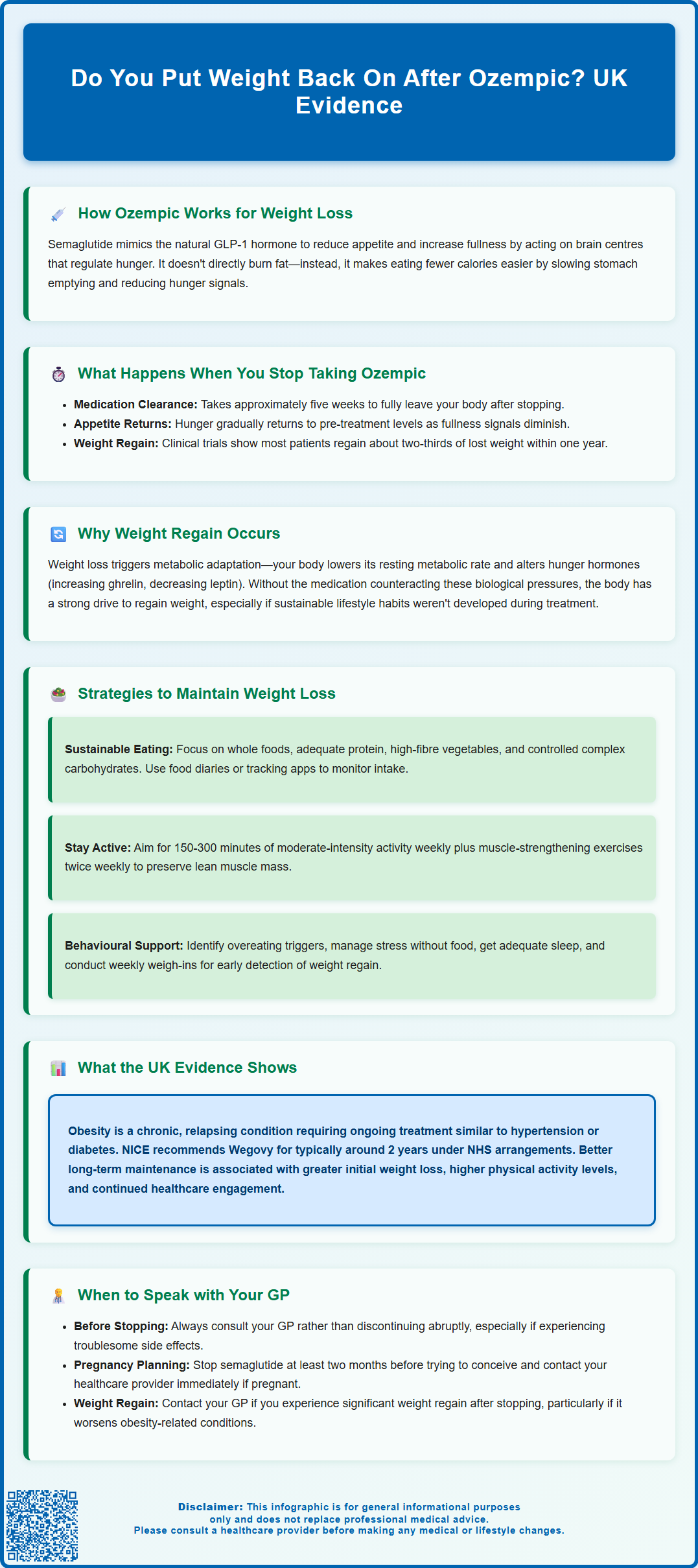
Many people wonder whether weight returns after stopping Ozempic (semaglutide), a concern supported by clinical evidence. When semaglutide treatment ends, its appetite-suppressing effects gradually fade as the medication clears from the body over approximately five weeks. Research, including the STEP 4 trial published in JAMA, demonstrates that most individuals regain around two-thirds of their lost weight within a year of discontinuation. This occurs because the medication's influence on hunger regulation ceases, and underlying metabolic adaptations that defend against weight loss reassert themselves. Understanding these mechanisms and implementing evidence-based maintenance strategies are essential for anyone considering or currently using semaglutide for weight management in the UK.
Summary: Most people regain approximately two-thirds of their lost weight within one year of stopping Ozempic (semaglutide), as the medication's appetite-suppressing effects cease and underlying metabolic adaptations reassert themselves.
- Semaglutide is a GLP-1 receptor agonist that reduces appetite by acting on brain centres and slowing gastric emptying, requiring ongoing weekly injections to maintain effects.
- The medication has a one-week half-life and takes approximately five weeks to clear from the body after the final dose, during which appetite gradually returns.
- Weight regain occurs due to removal of appetite suppression, metabolic adaptation during weight loss, and hormonal changes including increased ghrelin and decreased leptin.
- NICE recommends Wegovy (semaglutide 2.4mg) for weight management only through specialist services for adults with BMI ≥35 kg/m² (or ≥30 kg/m² with comorbidities), typically limited to around 2 years under NHS arrangements.
- Maintaining weight loss requires comprehensive lifestyle changes including sustainable dietary patterns, regular physical activity, behavioural strategies, and ongoing healthcare support.
- Decisions to stop or continue semaglutide should always be made in consultation with your GP or prescribing healthcare professional, with consideration of individual circumstances and health status.
Table of Contents
- How Ozempic Works for Weight Loss
- What Happens When You Stop Taking Ozempic
- Why Weight Regain Occurs After Stopping Ozempic
- Strategies to Maintain Weight Loss After Ozempic
- Long-Term Weight Management: What the Evidence Shows
- When to Speak with Your GP About Stopping Ozempic
- Scientific References
- Frequently Asked Questions
How Ozempic Works for Weight Loss
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK specifically for the treatment of type 2 diabetes mellitus. For weight management, the Medicines and Healthcare products Regulatory Agency (MHRA) has approved semaglutide at a higher dose (2.4mg) under the brand name Wegovy. It's important to distinguish between these medications, as they contain the same active ingredient but at different doses for different licensed indications.
The mechanism of action involves mimicking the naturally occurring hormone GLP-1, which is released from the intestine in response to food intake. Semaglutide binds to GLP-1 receptors in multiple tissues, including the pancreas, gastrointestinal tract, and brain. In the pancreas, it enhances glucose-dependent insulin secretion and suppresses inappropriate glucagon release, thereby improving glycaemic control. In the gastrointestinal system, it slows gastric emptying, which prolongs the sensation of fullness after meals and reduces appetite.
Crucially, semaglutide acts on appetite-regulating centres in the hypothalamus, reducing hunger signals and food cravings. This multifaceted approach leads to a spontaneous reduction in caloric intake, which is the primary driver of weight loss. Clinical trials of Wegovy (semaglutide 2.4mg) have demonstrated weight reductions of approximately 15% of initial body weight at 68 weeks, while Ozempic at diabetes doses typically produces more modest weight loss. The STEP 1 trial published in the New England Journal of Medicine (2021) provides the key evidence for Wegovy's efficacy.
It is important to understand that semaglutide does not directly burn fat or increase metabolism. Rather, it creates physiological conditions that make it easier for individuals to adhere to a reduced-calorie diet by diminishing hunger and enhancing satiety. The medication requires ongoing administration via weekly subcutaneous injection to maintain these effects, as the drug's influence on appetite regulation is not permanent once treatment ceases.
In the UK, NICE Technology Appraisal 875 recommends Wegovy only for adults with a BMI of at least 35 kg/m² (or 30 kg/m² with weight-related comorbidities) and through specialist weight management services. Treatment is typically limited to around 2 years under NHS commissioning arrangements.
What Happens When You Stop Taking Ozempic
When treatment with semaglutide is discontinued, the medication's effects on appetite regulation and gastric emptying gradually diminish as the drug is cleared from the body. According to the Summary of Product Characteristics, semaglutide has a half-life of approximately one week, meaning it takes roughly five weeks for the medication to be substantially eliminated from the system after the final dose. During this washout period, patients typically notice a progressive return of appetite and hunger signals.
Many individuals report that their previous eating patterns and food cravings re-emerge within weeks of stopping treatment. The sensation of fullness after meals becomes less pronounced, and the volume of food required to feel satisfied often increases back towards pre-treatment levels. This physiological shift occurs because the external GLP-1 receptor stimulation provided by semaglutide is no longer present, and the body reverts to its baseline appetite regulation.
Clinical studies examining weight trajectories after semaglutide discontinuation have consistently demonstrated that most patients experience some degree of weight regain. The STEP 4 trial (published in JAMA, 2021) and the STEP 1 extension study (published in Diabetes, Obesity and Metabolism, 2022) showed that within one year of stopping treatment, individuals typically regain approximately two-thirds of the weight they had lost whilst on the medication.
The rate and extent of weight regain vary considerably between individuals and depend on multiple factors, including the lifestyle modifications adopted during treatment, ongoing dietary habits, physical activity levels, and underlying metabolic factors. Some patients maintain a portion of their weight loss, whilst others return close to their pre-treatment weight. In some cases, individuals may regain more than their original weight loss, though responses vary significantly between patients.
Why Weight Regain Occurs After Stopping Ozempic
Weight regain following semaglutide cessation is primarily explained by the removal of the medication's appetite-suppressing effects, combined with complex physiological adaptations that occur during weight loss. When individuals lose significant weight, the body undergoes metabolic adaptations often referred to as "adaptive thermogenesis" or "metabolic adaptation." These changes represent the body's attempt to defend against what it perceives as an energy deficit and potential threat to survival.
Research by Sumithran et al. (New England Journal of Medicine, 2011) has demonstrated that weight loss triggers a reduction in resting metabolic rate that exceeds what would be predicted based solely on the loss of metabolically active tissue. Additionally, hormones that regulate hunger and satiety undergo unfavourable changes: levels of ghrelin (the hunger hormone) increase, whilst levels of leptin (which signals satiety) decrease. These hormonal shifts create a biological drive to increase food intake and restore lost weight. When semaglutide is discontinued, these underlying metabolic pressures are no longer counteracted by the medication's appetite-suppressing properties.
Furthermore, many individuals may not have established sustainable dietary and activity patterns during their time on medication. If weight loss occurred primarily due to the medication's effects rather than through the development of lasting behavioural changes, the foundation for weight maintenance is inherently unstable. The medication may have facilitated weight loss without requiring the individual to develop the skills, habits, and psychological strategies necessary for long-term weight management.
Psychological factors also contribute to weight regain. Some patients may experience a sense of deprivation or restriction whilst on the medication, leading to compensatory eating behaviours once treatment stops. Others may have unrealistic expectations about maintaining weight loss without ongoing intervention. The absence of regular medical monitoring and support that often accompanies medication treatment can further reduce accountability and motivation for continued lifestyle modification.
Strategies to Maintain Weight Loss After Ozempic
Maintaining weight loss after discontinuing semaglutide requires a comprehensive, evidence-based approach that addresses both dietary habits and physical activity. The National Institute for Health and Care Excellence (NICE) guidance on obesity management (CG189) recommends that weight management interventions should include behavioural components that support long-term lifestyle change, rather than relying solely on pharmacological treatment.
Dietary strategies should focus on establishing sustainable eating patterns rather than restrictive diets. A balanced approach that emphasises whole foods, adequate protein intake (which enhances satiety), high-fibre vegetables, and controlled portions of complex carbohydrates can help manage appetite without the medication's assistance. Keeping a food diary or using a nutrition tracking application may increase awareness of eating patterns and caloric intake. Regular meal timing and avoiding prolonged periods without food can help stabilise blood glucose levels and reduce excessive hunger.
Physical activity plays a crucial role in weight maintenance. The UK Chief Medical Officers' Physical Activity Guidelines recommend at least 150-300 minutes of moderate-intensity activity per week, or 75-150 minutes of vigorous activity, plus muscle-strengthening activities on at least two days per week. However, research suggests that those maintaining significant weight loss may benefit from higher volumes of activity. Resistance training is particularly valuable as it helps preserve lean muscle mass, which supports metabolic rate. Finding enjoyable forms of movement increases the likelihood of long-term adherence.
Behavioural strategies are equally important. These include identifying and managing triggers for overeating, developing stress management techniques that do not involve food, ensuring adequate sleep (as sleep deprivation increases appetite hormones), and building a supportive environment. Regular self-monitoring through weekly weigh-ins can provide early warning of weight regain, allowing for prompt intervention. The NHS provides Tier 2 lifestyle weight management services in many areas, and your GP can refer you to these programmes or to dietetic services. For those with more complex needs, Tier 3 specialist weight management services may be appropriate. Cognitive behavioural approaches that address the psychological aspects of eating and body image can be particularly helpful for sustainable change.
Long-Term Weight Management: What the Evidence Shows
The evidence base regarding long-term weight management following GLP-1 receptor agonist treatment is evolving, with emerging data providing important insights for clinical practice. The STEP (Semaglutide Treatment Effect in People with obesity) trial programme has been particularly informative. The STEP 4 trial (JAMA, 2021) specifically examined what happens when semaglutide is withdrawn after initial weight loss. Participants who discontinued semaglutide after 20 weeks regained approximately two-thirds of their lost weight over the subsequent 48 weeks, whilst those who continued treatment maintained their weight loss and achieved further modest reductions.
These findings align with our broader understanding of obesity as a chronic, relapsing condition rather than an acute problem that can be permanently resolved with short-term intervention. The biological mechanisms that defend against weight loss remain active long after weight reduction, creating ongoing physiological pressure towards weight regain. This has led many obesity medicine specialists to conceptualise pharmacological treatment for obesity similarly to treatment for other chronic conditions such as hypertension or type 2 diabetes, where ongoing therapy is typically required to maintain therapeutic benefits.
It is important to note that in the UK, NICE Technology Appraisal 875 recommends semaglutide 2.4mg (Wegovy) for weight management through specialist services with treatment typically limited to around 2 years under current NHS commissioning arrangements. Continuation beyond this period would require individual funding decisions.
Factors associated with better weight maintenance include greater initial weight loss, higher levels of physical activity, continued engagement with healthcare services, and the presence of structured support systems. The recent SELECT trial (NEJM, 2023) has provided additional evidence on longer-term outcomes with semaglutide treatment, though primarily focused on cardiovascular benefits rather than weight maintenance.
NICE guidance on obesity management acknowledges that pharmacological treatment may be appropriate for some individuals, particularly when weight regain occurs after stopping medication and the person has obesity-related comorbidities. The decision to continue, stop, or restart treatment should be individualised, taking into account clinical response, tolerability, patient preference, and the presence of weight-related health complications. As with all medications, ongoing monitoring for adverse effects is essential.
When to Speak with Your GP About Stopping Ozempic
The decision to discontinue semaglutide should always be made in consultation with your GP or the healthcare professional who prescribed the medication, rather than stopping abruptly without medical guidance. There are several circumstances when a discussion about stopping or continuing treatment is particularly important. If you are experiencing troublesome adverse effects such as persistent nausea, vomiting, abdominal pain, or other gastrointestinal symptoms that significantly impact your quality of life, your GP can assess whether dose adjustment, symptomatic management, or treatment cessation is most appropriate.
You should contact your GP promptly if you develop symptoms that might indicate serious complications, including severe abdominal pain (which could indicate pancreatitis), right upper quadrant pain, fever or jaundice (which might suggest gallbladder problems), visual changes, a persistent lump in the neck or hoarseness, or symptoms of hypoglycaemia if you are taking other diabetes medications. These situations require urgent clinical assessment. Additionally, if you are planning pregnancy or discover you are pregnant, immediate discussion with your healthcare provider is essential, as semaglutide is not recommended during pregnancy and should be discontinued at least two months before conception attempts, according to the Summary of Product Characteristics.
If you have achieved your weight loss goals and are considering stopping treatment, a planned discussion with your GP allows for the development of a structured maintenance plan. Your GP can help you assess whether you have established sustainable lifestyle changes, discuss realistic expectations about weight maintenance, and arrange appropriate follow-up monitoring. They may refer you to NHS Tier 2 lifestyle services or Tier 3 specialist weight management programmes to support the transition off medication.
Conversely, if you have stopped semaglutide and are experiencing significant weight regain, particularly if this is affecting obesity-related health conditions such as type 2 diabetes, hypertension, or sleep apnoea, you should discuss this with your GP. Restarting treatment may be clinically appropriate in some cases, though it's important to note that Wegovy for weight management is prescribed through specialist weight management services according to NICE guidance. Your GP can also explore whether there are barriers to weight maintenance that could be addressed through additional support services. Regular communication with your healthcare team ensures that decisions about continuing or stopping treatment are made collaboratively, with full consideration of your individual circumstances, health status, and treatment goals.
Scientific References
- Wegovy 0.25 mg, FlexTouch solution for injection in pre-filled pen - Summary of Product Characteristics.
- Semaglutide for managing overweight and obesity. Technology appraisal guidance [TA875].
- Once-Weekly Semaglutide in Adults with Overweight or Obesity.
- Obesity - Treatment.
- Ozempic - European Public Assessment Report.
Frequently Asked Questions
How quickly does weight return after stopping Ozempic?
Weight regain typically begins within weeks of stopping semaglutide as appetite returns, with clinical studies showing most individuals regain approximately two-thirds of their lost weight within one year of discontinuation. The rate varies depending on lifestyle modifications, dietary habits, and physical activity levels maintained after stopping treatment.
Can you maintain weight loss after stopping semaglutide without regaining?
Some individuals maintain a portion of their weight loss through comprehensive lifestyle changes including sustainable dietary patterns, regular physical activity (150-300 minutes weekly), behavioural strategies, and ongoing healthcare support. However, maintaining significant weight loss without medication requires substantial effort due to metabolic adaptations and hormonal changes that promote weight regain.
Should I discuss stopping Ozempic with my GP before doing so?
Yes, you should always consult your GP or prescribing healthcare professional before stopping semaglutide rather than discontinuing abruptly. Your doctor can help develop a structured maintenance plan, assess whether sustainable lifestyle changes are established, arrange appropriate follow-up monitoring, and potentially refer you to NHS weight management services for ongoing support.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript