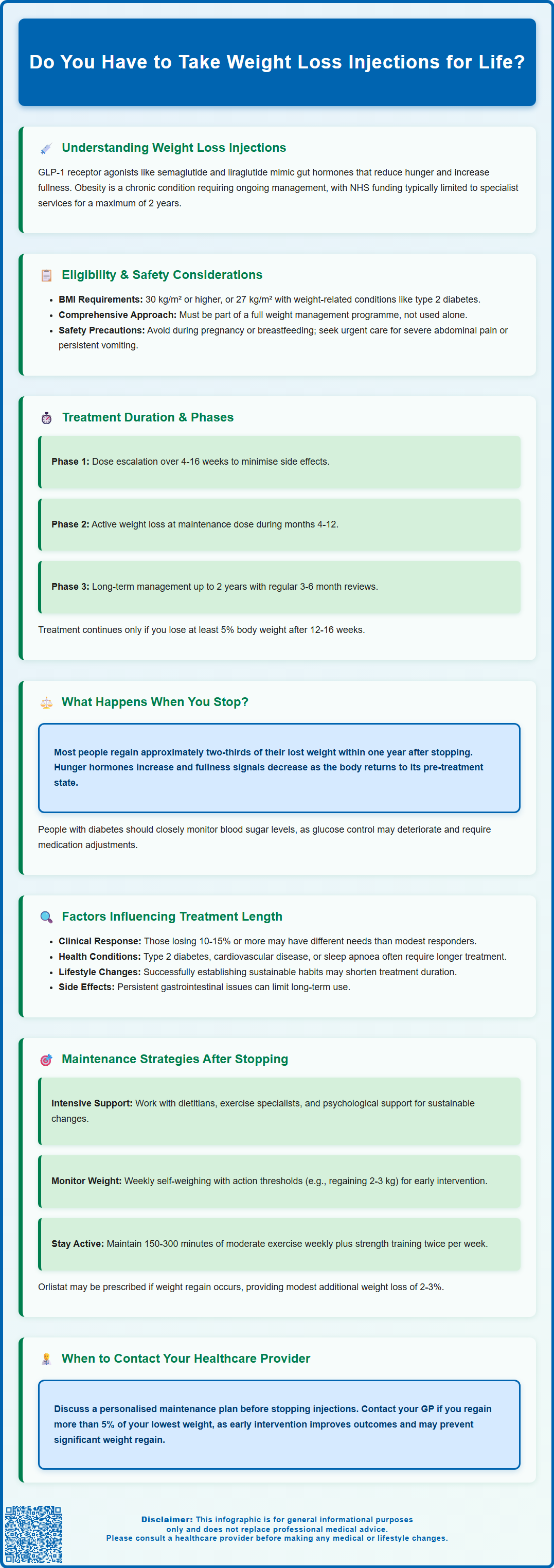
Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) are GLP-1 receptor agonists used to manage obesity in the UK. These medications work by regulating appetite and glucose metabolism, leading to significant weight reduction when combined with lifestyle changes. Treatment duration varies considerably between individuals and depends on clinical response, comorbidities, and tolerability. Under NHS care, NICE guidance typically limits treatment to a maximum of 2 years within specialist weight management services. The decision regarding how long to continue treatment should be made collaboratively with your healthcare team, considering your individual circumstances, weight loss goals, and ability to maintain lifestyle modifications.
Summary: Weight loss injections are not necessarily lifelong, with NHS treatment typically limited to a maximum of 2 years, though duration depends on individual response, comorbidities, and ability to maintain lifestyle changes.
- GLP-1 receptor agonists (semaglutide, liraglutide) work by mimicking gut hormones that regulate appetite and glucose metabolism.
- NICE guidance restricts NHS-funded use to specialist weight management services for up to 2 years maximum.
- Treatment continues only if patients achieve at least 5% weight loss after 12-16 weeks at maintenance dose.
- Most patients regain approximately two-thirds of lost weight within one year of stopping treatment.
- Treatment duration depends on clinical response, obesity-related comorbidities, tolerability, and patient preferences.
- Contraindicated during pregnancy and breastfeeding; requires caution with history of pancreatitis or gallbladder disease.
Table of Contents
Understanding Weight Loss Injections and Long-Term Use
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become important tools in obesity management in the UK. These medications work by mimicking natural gut hormones that regulate appetite and glucose metabolism. They slow gastric emptying (though this effect may diminish over time), enhance satiety signals to the brain, and reduce hunger, leading to significant weight reduction when combined with lifestyle modifications.
The question of lifelong treatment is complex and depends on individual circumstances. Current evidence suggests that obesity is a chronic, relapsing condition requiring ongoing management. These medications are licensed for weight management with duration guided by response and tolerability. Importantly, NHS-funded use is restricted by NICE guidance to specialist weight management services and typically limited to a maximum of 2 years.
Key considerations for treatment include:
-
The chronic nature of obesity as a medical condition
-
Individual metabolic responses and weight maintenance capacity
-
Presence of obesity-related comorbidities (type 2 diabetes, cardiovascular disease)
-
Patient preferences and treatment goals
-
UK eligibility criteria (typically BMI ≥30 kg/m², or ≥27 kg/m² with weight-related comorbidities)
NICE guidance emphasises that pharmacological treatment should be part of a comprehensive weight management programme, not a standalone solution. The decision regarding treatment duration should be made collaboratively between patients and healthcare professionals, with regular review of efficacy, tolerability, and ongoing need.
Important safety considerations include avoiding use during pregnancy or breastfeeding (with contraception advised during treatment), and caution in those with history of pancreatitis, gallbladder disease, or diabetic retinopathy. Seek urgent medical attention for severe abdominal pain, persistent vomiting or signs of dehydration.
How Long Do You Need to Take Weight Loss Injections?
Treatment duration with weight loss injections varies considerably between individuals and depends on multiple clinical factors. According to the product SmPCs (which NICE guidance incorporates), treatment should continue only if patients achieve at least 5% weight loss after 12 weeks at the maintenance dose for liraglutide (Saxenda), or after 16 weeks for semaglutide (Wegovy). This threshold ensures that patients are responding adequately to justify ongoing therapy.
Under NHS care, treatment is typically limited to a maximum of 2 years within specialist weight management services, as specified in NICE Technology Appraisals (TA875 for semaglutide and TA664 for liraglutide). Beyond this period, continued use would require private prescription.
Treatment phases typically include:
-
Initiation phase: Dose escalation (16 weeks for weekly semaglutide; 4 weeks for daily liraglutide)
-
Maintenance phase (months 4-12): Continued weight reduction at therapeutic dose
-
Long-term management (up to 2 years on NHS): Sustained weight maintenance or further loss
Your specialist weight management team will conduct regular reviews, typically every 3-6 months, to assess treatment response, monitor for adverse effects, and evaluate whether continuation is appropriate. Factors influencing duration include achievement of weight loss targets, improvement in obesity-related conditions (such as blood pressure or HbA1c levels), tolerability of side effects, and your ability to maintain lifestyle changes.
If you experience any side effects, report them to your healthcare professional and consider reporting via the MHRA Yellow Card scheme.
What Happens When You Stop Weight Loss Injections?
Discontinuing weight loss injections typically results in weight regain for most patients, though the extent varies considerably. The STEP 1 trial extension study demonstrated that participants who stopped semaglutide regained approximately two-thirds of their lost weight within one year of cessation. This occurs because the medication's effects on appetite regulation, gastric emptying, and metabolic signalling cease once treatment stops, and the underlying biological drivers of obesity reassert themselves.
The physiological response to stopping treatment reflects obesity's chronic nature. When you lose weight, your body undergoes metabolic adaptations that promote weight regain, including reduced energy expenditure, increased hunger hormones (such as ghrelin), and decreased satiety signals. Weight loss injections help counteract these adaptations, but their discontinuation removes this protective effect. Additionally, the neurological pathways governing food reward and appetite, which these medications modulate, return to their pre-treatment state.
Common experiences after stopping include:
-
Gradual return of appetite to pre-treatment levels
-
Increased hunger and reduced feelings of fullness
-
Weight regain over subsequent months (typically 3-12 months)
-
Potential worsening of obesity-related comorbidities if significant weight is regained
For people with diabetes, it's important to monitor blood glucose levels closely when stopping these medications, as diabetes control may worsen, requiring adjustment of other medications.
It is important to note that not all patients experience complete weight regain. Those who have successfully implemented sustainable lifestyle changes—including dietary modifications, regular physical activity, and behavioural strategies—may maintain some weight loss after discontinuation. However, maintaining weight loss without medication support requires considerable ongoing effort and is challenging for many individuals. If you are considering stopping treatment, discuss a structured discontinuation plan with your healthcare provider, including enhanced lifestyle support and regular monitoring to detect early weight regain.
Factors That Influence Treatment Duration
Multiple interconnected factors determine how long an individual may need weight loss injections, making treatment duration highly personalised. Clinical response is paramount—patients who achieve substantial weight loss (typically ≥10-15% of initial body weight) and experience significant improvements in comorbidities may have different duration needs compared to modest responders. Your metabolic profile, including insulin resistance, genetic factors affecting weight regulation, and baseline obesity severity, influences both treatment response and the likelihood of maintaining weight loss after cessation.
Obesity-related comorbidities significantly impact treatment duration decisions. Patients with type 2 diabetes, cardiovascular disease, obstructive sleep apnoea, or metabolic associated steatotic liver disease (MASLD) may require longer treatment to maintain the metabolic improvements achieved through weight loss. Recent research (SELECT trial) has shown cardiovascular benefits with semaglutide in people with established cardiovascular disease, though this specific indication is currently under regulatory review in the UK and not yet part of the licensed indications.
Additional factors include:
-
Lifestyle modification success: Patients who establish sustainable dietary and exercise habits may require shorter treatment durations
-
Previous weight loss attempts: History of weight cycling or unsuccessful maintenance may indicate need for longer therapy
-
Psychological factors: Presence of binge eating disorder or emotional eating patterns may necessitate extended treatment
-
Tolerability: Persistent gastrointestinal side effects may limit long-term use despite efficacy
-
Patient preferences and quality of life: Individual goals, injection burden, and treatment satisfaction
-
Pregnancy planning: Treatment should be stopped at least 2 months before planned conception
Your healthcare team should conduct comprehensive reviews at regular intervals, assessing not only weight changes but also metabolic markers (HbA1c, lipid profile, blood pressure), quality of life measures, and your confidence in maintaining weight loss independently. These multifactorial assessments guide shared decision-making about optimal treatment duration for your specific circumstances.
Alternatives and Maintenance Strategies After Stopping
Successfully maintaining weight loss after discontinuing injections requires a comprehensive, structured approach. Intensive lifestyle support forms the foundation of post-medication maintenance. This includes working with dietitians to establish sustainable eating patterns, engaging with physiotherapists or exercise specialists for tailored physical activity programmes, and accessing psychological support to address behavioural aspects of weight management. NHS-commissioned weight management services and Tier 3 obesity services can provide this multidisciplinary support.
Pharmacological alternatives may be considered if weight regain occurs or appears imminent. Orlistat, a lipase inhibitor available on NHS prescription, offers a non-injection option, though with more modest weight loss effects (typically 2-3% additional loss compared to lifestyle alone). It requires a low-fat diet to minimise gastrointestinal side effects and may require fat-soluble vitamin supplementation. Any medication should be discussed with your healthcare provider to ensure it's appropriate for your circumstances.
For patients with severe obesity (typically BMI ≥35 kg/m² with comorbidities or ≥40 kg/m² without), referral to Tier 4 bariatric surgery services may be appropriate according to NICE guidance (CG189).
Structured maintenance strategies include:
-
Regular self-monitoring: Weekly weighing with predetermined action thresholds (e.g., regaining 2-3 kg triggers intervention)
-
Continued dietary structure: Maintaining portion control, meal planning, and mindful eating practices
-
Physical activity maintenance: Sustaining 150-300 minutes of moderate-intensity exercise weekly, plus muscle-strengthening activities on at least 2 days per week (UK Chief Medical Officers' guidelines)
-
Behavioural techniques: Stimulus control, stress management, and relapse prevention strategies
-
Medical monitoring: Regular GP reviews of weight, metabolic parameters, and comorbidity status
If you are planning to stop weight loss injections, discuss a personalised maintenance plan with your healthcare provider before discontinuation, ensuring adequate support structures are in place. Contact your GP if you experience weight regain exceeding 5% of your lowest achieved weight, as early intervention improves outcomes.
Frequently Asked Questions
How long can you take weight loss injections on the NHS?
Under NHS care, weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) are typically limited to a maximum of 2 years within specialist weight management services, as specified in NICE guidance. Treatment continues only if you achieve at least 5% weight loss after 12-16 weeks at the maintenance dose.
Will I regain weight after stopping weight loss injections?
Most patients experience weight regain after stopping weight loss injections, with studies showing approximately two-thirds of lost weight returning within one year of cessation. However, those who maintain sustainable lifestyle changes including dietary modifications and regular physical activity may retain some weight loss benefits.
What are the alternatives to weight loss injections for maintaining weight loss?
Alternatives include intensive lifestyle support through NHS weight management services, oral medications such as orlistat, structured self-monitoring with regular weighing, sustained physical activity (150-300 minutes weekly), and for eligible patients with severe obesity, referral to bariatric surgery services according to NICE guidance.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript