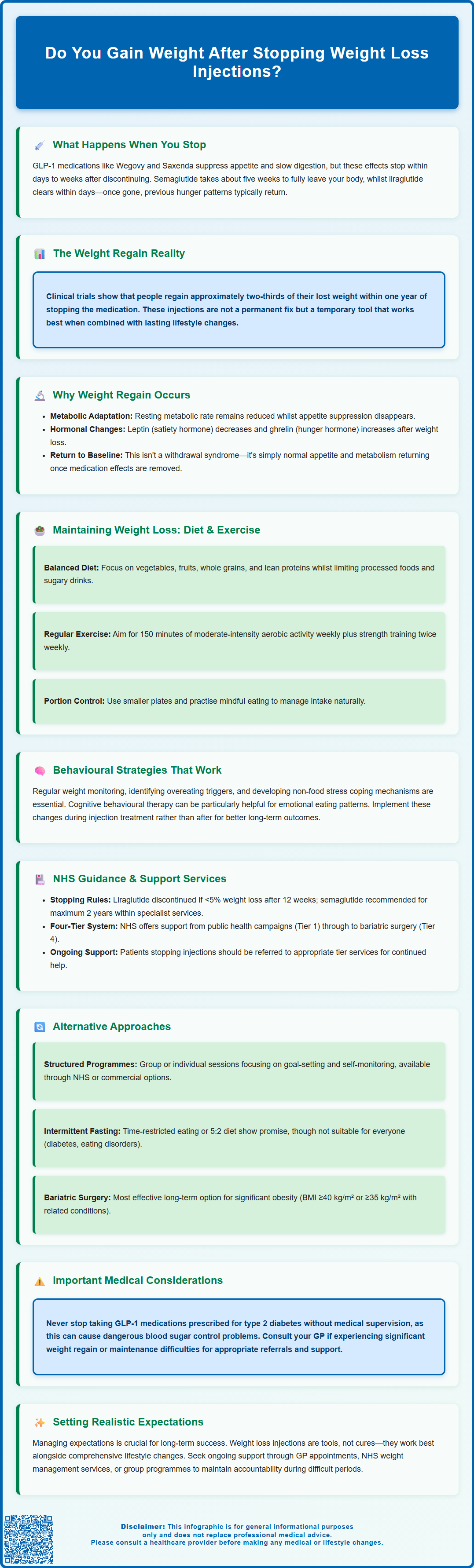
Weight regain after stopping weight loss injections is a common concern for patients using GLP-1 receptor agonists such as semaglutide (Wegovy) or liraglutide (Saxenda). Clinical evidence demonstrates that many individuals regain a significant proportion of lost weight within months of discontinuation. This occurs because the medication's appetite-suppressing and metabolic effects cease once treatment stops, whilst underlying physiological mechanisms that contributed to weight gain remain unchanged. Understanding why weight regain happens and implementing evidence-based strategies for long-term weight maintenance are essential for optimising outcomes. This article explores the mechanisms behind weight regain, practical approaches to sustaining weight loss, and NHS guidance on comprehensive weight management.
Summary: Yes, weight regain is common after stopping weight loss injections, with clinical trials showing patients regain approximately two-thirds of lost weight within one year of discontinuing GLP-1 receptor agonists.
- GLP-1 receptor agonists such as semaglutide and liraglutide suppress appetite by mimicking natural hormones; these effects cease within days to weeks after stopping treatment.
- Weight regain occurs due to metabolic adaptation, hormonal changes (reduced leptin, increased ghrelin), and return of previous appetite patterns once pharmacological support is withdrawn.
- NICE guidance recommends weight loss medications only alongside dietary advice, physical activity support, and behavioural interventions within multicomponent weight management programmes.
- Maintaining weight loss requires structured lifestyle changes including balanced nutrition, at least 150 minutes weekly moderate-intensity exercise, behavioural strategies, and ongoing professional support.
- Patients should never stop GLP-1 treatment for type 2 diabetes without consulting their healthcare provider, as this may cause deteriorating blood glucose control.
- NHS weight management services (Tier 2 and Tier 3) provide structured support for individuals discontinuing weight loss injections; GP referral is recommended for ongoing care.
Table of Contents
What Happens When You Stop Weight Loss Injections
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), work by mimicking natural hormones that regulate appetite and blood glucose levels. These medications slow gastric emptying, enhance feelings of fullness, and reduce hunger signals to the brain. When treatment is discontinued, these pharmacological effects cease within days to weeks, depending on the medication's half-life.
Semaglutide has a half-life of approximately one week, meaning most of the drug is eliminated from the body after about five half-lives (around five weeks). Liraglutide, with a shorter half-life of 13 hours, clears more rapidly. As the medication leaves your system, the appetite-suppressing effects diminish, and many individuals notice a return of previous hunger patterns and food cravings.
Clinical evidence from trials demonstrates that weight regain is common after stopping GLP-1 receptor agonists. The STEP 1 extension trial showed that participants who discontinued semaglutide regained approximately two-thirds of their lost weight within one year. This occurs because the underlying physiological mechanisms that contributed to weight gain—including hormonal regulation, metabolic rate, and appetite control—remain unchanged once the medication is withdrawn.
It is important to understand that weight loss injections are not a permanent solution but rather a tool to support weight management alongside lifestyle modifications. The Medicines and Healthcare products Regulatory Agency (MHRA) and prescribing guidance emphasise that these treatments should be part of a comprehensive weight management programme that includes dietary changes, increased physical activity, and behavioural support to optimise long-term outcomes.
Important note: If you are taking GLP-1 receptor agonists for type 2 diabetes, you should never stop treatment without consulting your healthcare provider, as this could lead to deteriorating blood glucose control.
Why Weight Regain Occurs After Stopping Treatment
Weight regain after discontinuing weight loss injections is a multifactorial process involving physiological, metabolic, and behavioural mechanisms. Understanding these factors can help patients and healthcare professionals develop realistic expectations and appropriate management strategies.
Metabolic adaptation plays a significant role in weight regain. During weight loss, the body undergoes adaptive changes that reduce energy expenditure—a phenomenon sometimes called "metabolic slowdown". Research indicates that resting metabolic rate can decrease beyond what would be expected from the loss of body mass alone. When GLP-1 medications are stopped, this reduced metabolic rate persists whilst appetite-suppressing effects disappear, creating an environment conducive to weight regain.
The body's hormonal response to weight loss also contributes to regain. Leptin levels (which signal satiety) decrease with weight loss, whilst ghrelin (the "hunger hormone") increases. These changes promote increased appetite and reduced energy expenditure—biological mechanisms that evolved to protect against starvation. GLP-1 receptor agonists temporarily override some of these signals, but once discontinued, the hormonal drive to regain weight reasserts itself.
Behavioural factors are equally important. Some individuals may not have established sustainable dietary and activity patterns during treatment, relying primarily on the medication's appetite-suppressing effects. Without the pharmacological support, previous eating habits may return. Additionally, psychological factors such as stress, emotional eating, and reduced motivation can contribute to weight regain.
Current evidence suggests weight regain primarily reflects physiological and behavioural drivers once treatment stops. There is no evidence of a pharmacological withdrawal syndrome or rebound effect beyond the return of normal appetite and metabolic processes. The weight regain reflects the removal of the medication's therapeutic effects rather than an adverse reaction to stopping treatment.
How to Maintain Weight Loss After Stopping Injections
Maintaining weight loss after discontinuing weight loss injections requires a structured, multifaceted approach that addresses diet, physical activity, behavioural strategies, and ongoing support. Evidence suggests that individuals who implement comprehensive lifestyle changes during treatment have better long-term outcomes.
Dietary strategies form the cornerstone of weight maintenance. Focus on a balanced diet rich in vegetables, fruits, whole grains, and lean proteins whilst limiting processed foods, sugary beverages, and high-fat items. Portion control remains crucial—using smaller plates, measuring servings, and eating mindfully can help manage calorie intake without feeling deprived. The NHS Eatwell Guide provides practical recommendations for balanced nutrition. Some individuals benefit from continued calorie tracking or working with a registered dietitian to develop personalised meal plans that are sustainable long-term.
Regular physical activity is essential for weight maintenance. The UK Chief Medical Officers' Physical Activity Guidelines recommend at least 150 minutes of moderate-intensity aerobic activity weekly, combined with strength training exercises on at least two days weekly. Physical activity not only burns calories but also helps preserve lean muscle mass, which supports metabolic rate. Finding enjoyable activities—whether walking, swimming, cycling, or group fitness classes—increases adherence. Incorporating movement throughout the day, such as taking stairs or walking during breaks, contributes to overall energy expenditure.
Behavioural strategies include setting realistic goals, self-monitoring weight regularly (at a frequency that supports adherence without causing distress), identifying and managing triggers for overeating, and developing coping mechanisms for stress that don't involve food. Cognitive behavioural therapy (CBT) techniques can be particularly helpful for addressing emotional eating patterns.
Ongoing support significantly improves maintenance success. This might include regular appointments with a GP or practice nurse, participation in weight management groups (such as those offered through local NHS services), or commercial programmes. Accountability and encouragement from healthcare professionals, family, or peer groups help sustain motivation during challenging periods. Ask your GP about referral to local NHS weight management services (Tier 2 or Tier 3) for structured support.
NHS Guidance on Long-Term Weight Management
The National Institute for Health and Care Excellence (NICE) provides comprehensive guidance on obesity management, emphasising that pharmacological interventions should be integrated within multicomponent weight management programmes. NICE guideline CG189 (Obesity: identification, assessment and management) recommends that weight loss medications are prescribed only alongside dietary advice, physical activity support, and behavioural interventions.
NICE has specific guidance for GLP-1 receptor agonists. For liraglutide 3 mg (Saxenda), NICE Technology Appraisal TA664 states treatment should be discontinued if patients do not lose at least 5% of their initial body weight after 12 weeks on the full 3 mg daily dose. For semaglutide 2.4 mg (Wegovy), NICE Technology Appraisal TA875 recommends treatment within specialist weight management services for up to a maximum of 2 years, with specific eligibility criteria.
The NHS Long Term Plan acknowledges obesity as a major public health challenge and commits to expanding access to evidence-based weight management services. NHS England has developed a tiered approach to weight management:
-
Tier 1: Universal services including public health campaigns and community-based interventions
-
Tier 2: Lifestyle weight management programmes delivered in community settings
-
Tier 3: Specialist multidisciplinary weight management services for individuals with complex needs
-
Tier 4: Bariatric surgery for those meeting specific criteria
Patients discontinuing weight loss injections should be referred to appropriate tier services for ongoing support. Many Integrated Care Boards (ICBs) within Integrated Care Systems (ICSs) commission Tier 2 programmes that provide structured support for 12–24 weeks, including dietary advice, physical activity guidance, and behavioural change techniques.
GP practices play a crucial role in long-term weight management. Regular monitoring, opportunistic advice during consultations, and referral to specialist services when appropriate are all part of comprehensive care. Patients should be encouraged to contact their GP if they experience significant weight regain or struggle with weight maintenance, as additional support or alternative interventions may be beneficial.
Alternative Approaches to Sustaining Weight Loss
For individuals seeking to maintain weight loss without continued pharmacological intervention, several evidence-based alternatives exist, each with varying levels of supporting evidence and suitability for different patients.
Structured behavioural programmes have robust evidence for supporting weight maintenance. These programmes typically include regular group or individual sessions focusing on goal-setting, self-monitoring, problem-solving, and relapse prevention. The NHS Diabetes Prevention Programme, whilst designed for diabetes prevention, incorporates many principles applicable to general weight maintenance. Commercial programmes such as Weight Watchers (WW) and Slimming World also provide structured support, though costs may be a consideration.
Intermittent fasting approaches, including time-restricted eating (limiting food intake to specific hours) or the 5:2 diet (reduced calorie intake on two non-consecutive days weekly), have shown some promise in weight management studies, though results vary between individuals. Individuals with diabetes, eating disorders, or certain medical conditions should consult their GP before attempting fasting regimens.
Meal replacement strategies, using portion-controlled products for one or two meals daily whilst eating a balanced meal, can help some individuals maintain structure and calorie control. NICE guidance (CG189) recognises low-energy total diet replacement programmes for initial weight loss under healthcare supervision, and partial meal replacement may support maintenance, though long-term adherence can be challenging.
Pharmacological alternatives include orlistat, a lipase inhibitor that reduces fat absorption, available both on prescription and over-the-counter (as Alli). Whilst generally less effective than GLP-1 receptor agonists, it may provide modest support for weight maintenance. Patients should be aware of potential gastrointestinal side effects, the need to follow a reduced-fat diet, and possible requirements for fat-soluble vitamin supplementation. Report any suspected side effects to the MHRA Yellow Card scheme.
Bariatric surgery represents the most effective long-term intervention for significant obesity. NICE recommends considering surgery for people with a BMI ≥40 kg/m² or ≥35 kg/m² with obesity-related conditions. Lower thresholds apply for people with type 2 diabetes (BMI ≥30 kg/m²) and those of South Asian origin. Procedures such as gastric bypass or sleeve gastrectomy produce substantial, sustained weight loss and metabolic improvements. Referral criteria and waiting times vary across NHS regions, and patients should discuss this option with their GP if interested.
Frequently Asked Questions
How quickly do you regain weight after stopping weight loss injections?
Weight regain typically begins within weeks of stopping GLP-1 receptor agonists as appetite-suppressing effects diminish. Clinical trials show patients may regain approximately two-thirds of lost weight within one year of discontinuation without sustained lifestyle changes.
Can you prevent weight regain after stopping semaglutide or liraglutide?
Whilst complete prevention is challenging, implementing comprehensive lifestyle changes during treatment—including balanced nutrition, regular physical activity (at least 150 minutes weekly), behavioural strategies, and ongoing support from NHS weight management services—significantly improves long-term weight maintenance outcomes.
Should I contact my GP if I regain weight after stopping weight loss injections?
Yes, contact your GP if you experience significant weight regain or struggle with weight maintenance. Your GP can provide additional support, refer you to NHS weight management services (Tier 2 or Tier 3), or discuss alternative interventions appropriate for your circumstances.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript