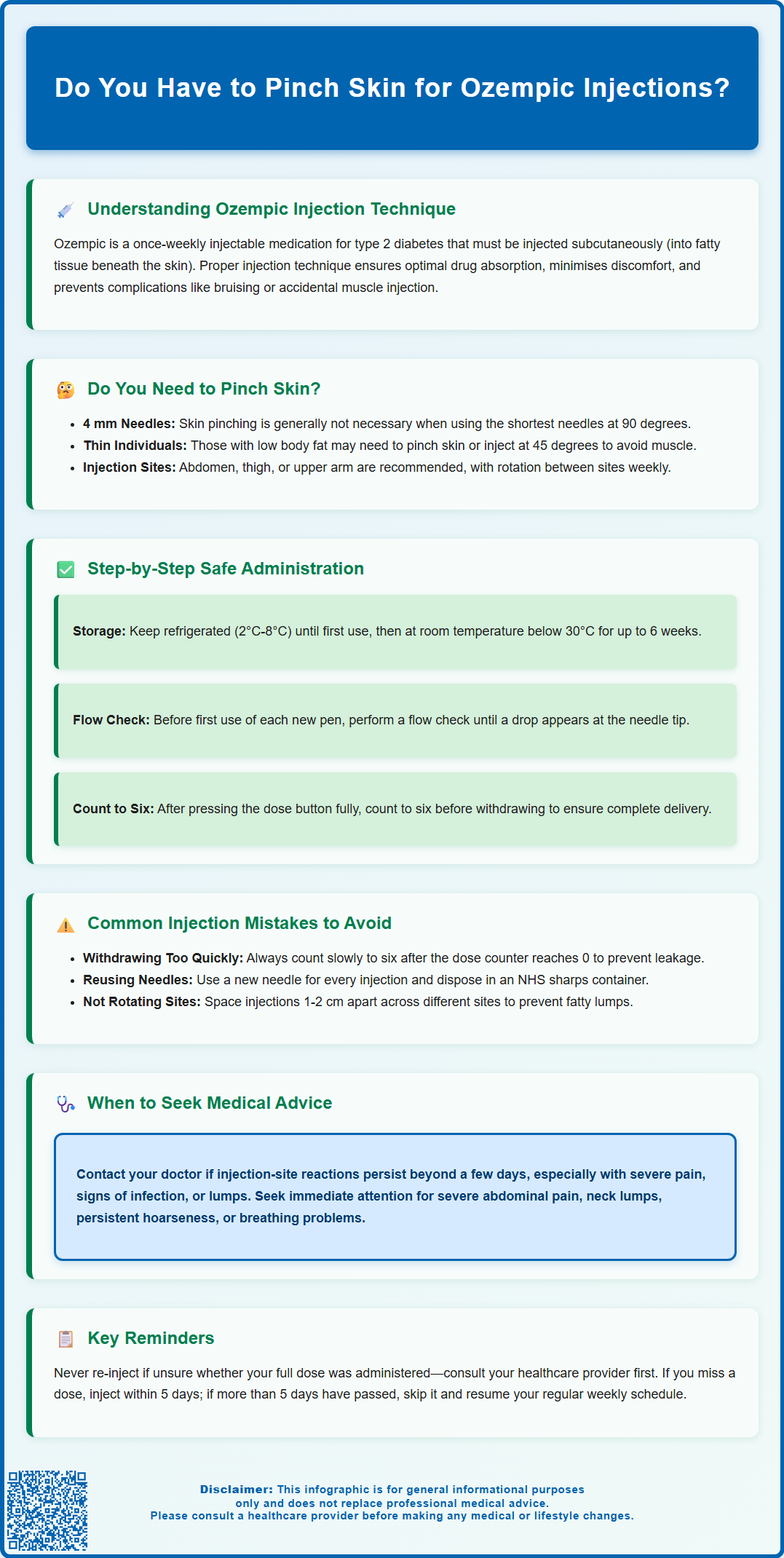
Ozempic (semaglutide) is a once-weekly injectable medication for type 2 diabetes that requires subcutaneous administration. Many patients wonder: do you have to pinch skin for Ozempic injections? The answer depends on needle length and individual body composition. With shorter 4 mm needles—the most commonly used—skin pinching is typically unnecessary for most adults. However, those with very low body fat may benefit from pinching or angling the injection. Understanding proper injection technique ensures optimal medication absorption, minimises discomfort, and reduces complications. This guide explains when skin pinching is needed and how to administer Ozempic safely at home.
Summary: Skin pinching is generally not necessary when injecting Ozempic with 4 mm needles, though individuals with very low body fat may benefit from pinching or angling the injection.
- Ozempic is a GLP-1 receptor agonist administered subcutaneously once weekly for type 2 diabetes management
- Shorter 4 mm pen needles typically reach subcutaneous tissue without skin pinching when injected at 90 degrees
- Individuals with very low body fat may require skin pinching or 45-degree angle injection to avoid intramuscular administration
- Proper technique includes holding the dose button for six seconds after the counter reaches zero to ensure complete delivery
- Injection sites should be rotated systematically between abdomen, thigh, and upper arm to prevent lipohypertrophy
- Needles must never be reused or shared, and used sharps require disposal in NHS-prescribed sharps containers
Table of Contents
Understanding Ozempic Injection Technique
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It is administered as a subcutaneous injection once weekly using a pre-filled pen device. The medication works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, and slows gastric emptying. This mechanism helps improve glycaemic control whilst also promoting weight loss in many patients, although it is important to note that Ozempic is not licensed for weight loss in the UK.
The subcutaneous route of administration means that Ozempic must be injected into the fatty tissue layer beneath the skin, rather than into muscle or directly into the bloodstream. This layer of adipose tissue provides a reservoir from which the medication is gradually absorbed into the systemic circulation, ensuring consistent therapeutic levels throughout the week. The pen device is designed for ease of use and comes in different strengths that deliver weekly doses of 0.25 mg, 0.5 mg, 1 mg, or 2 mg, depending on the prescribing regimen.
Proper injection technique is essential for ensuring optimal drug absorption, minimising discomfort, and reducing the risk of injection-site reactions such as bruising, lipohypertrophy, or inadvertent intramuscular injection. Understanding the correct method for administering Ozempic, including whether to pinch the skin during injection, forms a crucial part of patient education and self-management. Healthcare professionals should provide comprehensive training when initiating treatment, and patients should feel confident in their technique before administering injections independently at home. For safety reasons, pens and needles should never be shared with others, even if the needle has been changed.
Do You Need to Pinch Skin When Injecting Ozempic?
The question of whether to pinch the skin when injecting Ozempic depends primarily on the needle length and the injection site chosen. Ozempic pens do not come with needles included; compatible pen needles (such as NovoFine or NovoFine Plus) need to be prescribed separately. According to current guidance from FIT UK (Forum for Injection Technique) and the manufacturer's instructions, skin pinching is generally not necessary when using shorter 4 mm needles. These needles are specifically designed to reach the subcutaneous tissue without penetrating into the underlying muscle layer, even without creating a skin fold.
For most adults, injecting at a 90-degree angle to the skin without pinching is appropriate when using 4 mm needles. The subcutaneous fat layer in recommended injection sites—the abdomen, thigh, or upper arm—is typically sufficient to accommodate these needle lengths safely. However, there are exceptions to this general rule. Individuals with very low body fat, particularly in certain injection sites, or those who are notably thin may benefit from either pinching the skin or injecting at a 45-degree angle to avoid inadvertent intramuscular injection.
If skin pinching is deemed necessary, the technique involves gently gathering the skin and subcutaneous tissue between the thumb and forefinger to create a raised fold. This should be done without squeezing too tightly, as excessive pressure can cause discomfort and potentially affect absorption. The injection should be administered into the raised fold, and the skin should be released after the injection is complete and the needle has been withdrawn. It's worth noting that upper-arm injections may require assistance from another person to ensure correct technique and avoid intramuscular injection. Patients should discuss their individual circumstances with their diabetes specialist nurse or GP to determine the most appropriate technique for their body composition and chosen injection sites.
Step-by-Step Guide to Administering Ozempic Safely
Before administering Ozempic, ensure the pen has been stored correctly in the refrigerator between 2°C and 8°C until first use, after which it may be kept at room temperature below 30°C for up to six weeks. Never use the pen if it has been frozen. Remove the pen from the refrigerator approximately 15 minutes before injection to allow it to reach room temperature, which can reduce injection discomfort. Check that the solution is clear, colourless, and free from particles. Wash your hands thoroughly with soap and water, and gather all necessary supplies including the Ozempic pen, a new pen needle, and an appropriate sharps container for safe needle disposal.
Attach a new needle to the pen by removing the protective seal and screwing the needle straight onto the pen until secure. Remove both the outer and inner needle caps, keeping the outer cap for later disposal. Before the first use of each new pen, you must perform a flow check to ensure the pen is working correctly and to remove any air bubbles. A flow check should also be performed if the pen has been dropped or you suspect no dose has been delivered. Turn the dose selector to the flow check symbol, point the needle upwards, and tap the pen gently. Press and hold the dose button until the dose counter returns to zero and a drop of medication appears at the needle tip. If no drop appears, repeat this process up to six times.
Select your prescribed dose using the dose selector, ensuring the correct number appears in the dose counter window. Choose an injection site on your abdomen (at least 5 cm away from the navel), front of the thigh, or upper arm, rotating sites each week to prevent lipohypertrophy. Note that upper-arm injections are best given by another person. Clean the chosen area with an alcohol wipe if recommended by your healthcare team, though this is not always necessary for home injections. Insert the needle into the skin at a 90-degree angle using a swift, dart-like motion. Press and hold the dose button fully down until the dose counter shows 0, then keep it pressed whilst counting to six to ensure complete dose delivery. This pause is crucial as Ozempic is a viscous solution that requires time to be fully administered. Withdraw the needle straight out, and carefully replace the outer needle cap before unscrewing and disposing of the used needle in a sharps container. Never reuse needles, as this increases infection risk and can damage the pen mechanism. After use, replace the pen cap to protect the medication from light. Used needles and pens must be disposed of in an NHS-prescribed sharps bin, which can be arranged for collection via your local council or NHS service, never in household waste.
Common Injection Mistakes and How to Avoid Them
One of the most frequent errors patients make when self-administering Ozempic is failing to complete the full six-second count after pressing the dose button. Releasing the button too quickly or withdrawing the needle prematurely can result in incomplete dose delivery, with medication leaking from the injection site. This may lead to suboptimal glycaemic control and confusion about whether the full dose was received. To avoid this, patients should be reminded to keep the needle in place while pressing the dose button until the dose counter shows 0, then count slowly to six whilst maintaining firm pressure on the dose button, only releasing after the needle has been fully withdrawn from the skin.
Another common mistake involves inadequate site rotation. Repeatedly injecting into the same area can cause lipohypertrophy—a buildup of fatty tissue that creates lumps under the skin. These areas have altered absorption characteristics, potentially affecting the medication's efficacy and causing unpredictable blood glucose levels. Patients should rotate injection sites systematically, using different areas of the abdomen, thighs, and upper arms, and spacing injections at least 1-2 cm apart within a site. Keeping a simple diary or using a rotation pattern can help maintain good practice.
Reusing needles is another significant error that compromises both safety and treatment effectiveness. Used needles become blunted and bent, making subsequent injections more painful and increasing the risk of tissue damage. Additionally, leaving a needle attached to the pen between doses can allow air to enter the cartridge or medication to leak out, affecting dose accuracy. Needles should be removed and disposed of immediately after each injection. Some patients also forget to perform the flow check before their first injection with a new pen, which is essential for priming the device and ensuring proper function. Finally, injecting cold medication directly from the refrigerator can cause unnecessary discomfort; allowing the pen to reach room temperature significantly improves the injection experience.
When to Seek Medical Advice About Ozempic Injections
Patients should contact their GP or diabetes specialist nurse if they experience persistent injection-site reactions that do not resolve within a few days. Whilst mild redness, slight swelling, or minor bruising at the injection site is relatively common and usually resolves spontaneously, more significant reactions warrant medical review. These include severe pain, extensive bruising, signs of infection such as increasing warmth, spreading redness, pus formation, or fever. Such symptoms may indicate cellulitis or abscess formation requiring antibiotic treatment. Additionally, if lumps or hard areas develop at injection sites that persist beyond a few weeks, this may represent lipohypertrophy and should be assessed, as continued injection into these areas can impair medication absorption.
Patients should seek prompt medical attention if they develop symptoms suggestive of serious adverse effects, even if these are not directly related to injection technique. Severe, persistent abdominal pain, particularly if radiating to the back and accompanied by nausea and vomiting, may indicate pancreatitis—a rare but serious potential adverse effect of GLP-1 receptor agonists. Similarly, symptoms such as a lump in the neck, persistent hoarseness, difficulty swallowing, or shortness of breath should prompt medical review. While semaglutide has been associated with C-cell tumours in rodents, the relevance to humans is unknown. Seek urgent care if experiencing airway compromise symptoms.
Patients should also seek medical advice if they experience severe, persistent vomiting or diarrhoea, which could lead to dehydration, or symptoms of gallbladder disease such as upper abdominal pain, fever, or jaundice. Those with pre-existing diabetic retinopathy should be aware that rapid improvement in blood glucose control may temporarily worsen retinopathy and should attend regular eye screening appointments.
If patients are uncertain whether they have administered their full dose due to pen malfunction, medication leakage, or technique errors, they should not attempt to re-inject or take an additional dose without first consulting their healthcare provider. Taking more than the prescribed dose could increase the risk of adverse effects, particularly gastrointestinal symptoms and hypoglycaemia if used in combination with other glucose-lowering medications. Conversely, if a dose is missed entirely, patients should follow the guidance provided with their medication: if fewer than five days have passed since the missed dose, inject as soon as remembered; if more than five days have passed, skip the missed dose and resume the regular weekly schedule. Any concerns about injection technique, pen function, or dose administration should be discussed with the diabetes care team, who can provide additional training and support to ensure safe and effective treatment.
Scientific References
Frequently Asked Questions
What needle length is recommended for Ozempic injections?
The 4 mm pen needle is most commonly recommended for Ozempic injections, as it safely reaches subcutaneous tissue without requiring skin pinching for most adults. Compatible needles such as NovoFine or NovoFine Plus must be prescribed separately as they are not included with the pen.
How long should I hold the dose button when injecting Ozempic?
After pressing the dose button until the counter shows zero, continue holding it whilst counting slowly to six before withdrawing the needle. This ensures complete delivery of the viscous medication and prevents dose leakage from the injection site.
Where should I inject Ozempic on my body?
Ozempic should be injected into the abdomen (at least 5 cm from the navel), front of the thigh, or upper arm. Rotate injection sites weekly and space injections 1-2 cm apart within each site to prevent lipohypertrophy and ensure consistent medication absorption.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript