Weight loss injections, including semaglutide (Wegovy) and liraglutide (Saxenda), are increasingly prescribed for obesity management in the UK. A common question amongst patients considering these treatments is: do weight loss injections hurt? Most people experience minimal discomfort—typically a brief pinch or sting lasting only seconds. The fine needles used (31G–32G) and subcutaneous delivery into fatty tissue help reduce pain. However, individual experiences vary based on pain threshold, injection technique, needle size, and anxiety levels. Understanding what to expect and how to minimise discomfort can help patients feel more confident about starting treatment.
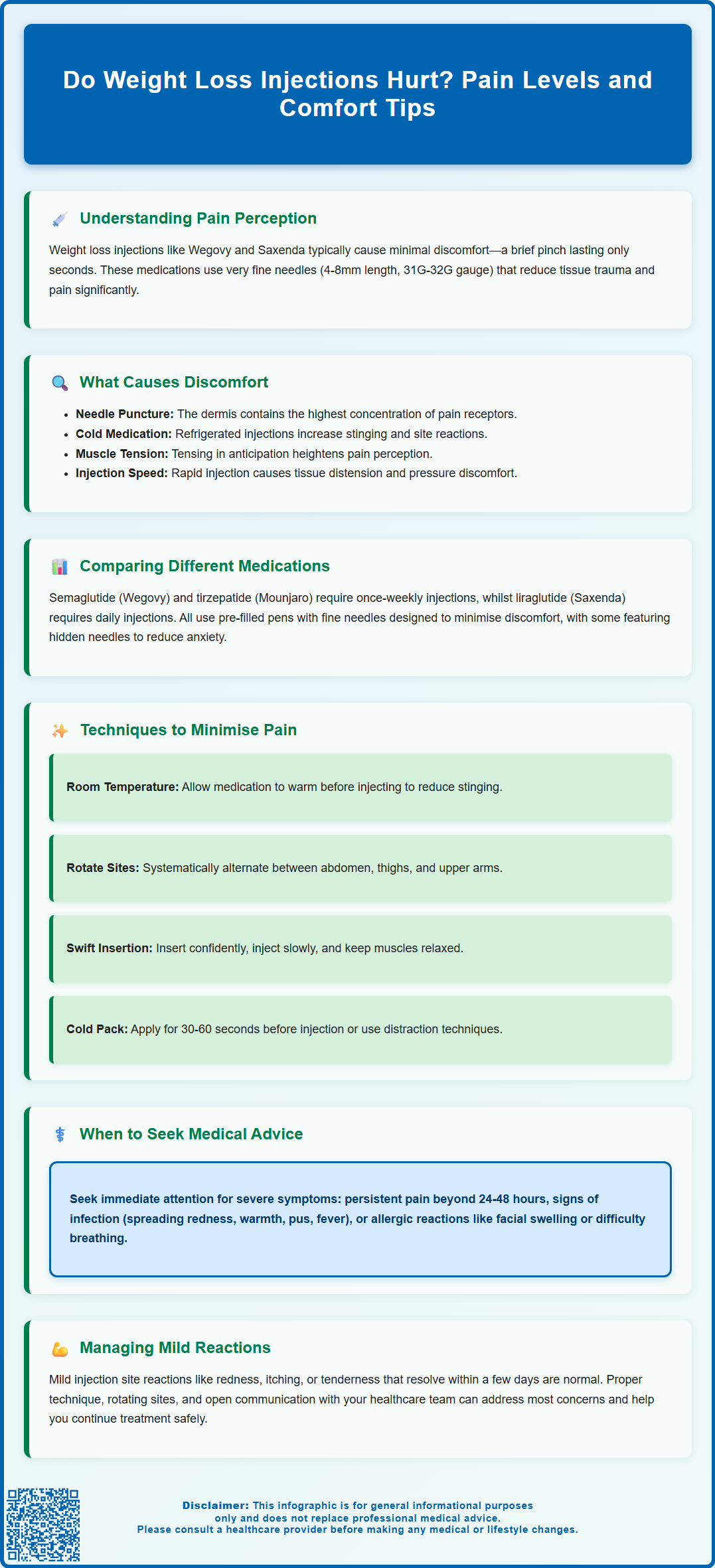
Summary: Weight loss injections typically cause minimal discomfort, often described as a brief pinch or sting lasting only seconds, due to the fine needles used and subcutaneous delivery method.
- GLP-1 receptor agonists like semaglutide (Wegovy) and liraglutide (Saxenda) use fine-gauge needles (31G–32G) that are thinner than standard injection needles, reducing tissue trauma and pain.
- Subcutaneous injection delivers medication into fatty tissue beneath the skin rather than muscle, which minimises discomfort compared to intramuscular injections.
- Pain perception varies between individuals and is influenced by anxiety levels, injection technique, needle size, injection site selection, and personal pain threshold.
- Proper technique—including allowing medication to reach room temperature, rotating injection sites, relaxing muscles, and injecting slowly—can substantially reduce discomfort and injection site reactions.
- Seek medical advice if you experience severe or worsening pain, signs of infection, significant bruising, allergic reaction symptoms, or persistent lumps at injection sites.
Table of Contents
- Understanding Weight Loss Injections and Pain Perception
- What Causes Discomfort During Weight Loss Injections
- Pain Levels: Comparing Different Injectable Weight Loss Medications
- Techniques to Minimise Pain and Injection Site Reactions
- When to Seek Medical Advice About Injection Pain
- Frequently Asked Questions
Understanding Weight Loss Injections and Pain Perception
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for obesity management in the UK. A common concern amongst patients considering these treatments is whether the injections cause pain. The experience of pain during subcutaneous injections varies between individuals and is influenced by multiple factors including needle gauge, injection technique, anatomical site, and personal pain threshold.
Many patients find that weight loss injections cause minimal discomfort, often described as a brief pinch or sting lasting only seconds. The needles used for these medications are fine—typically 4mm to 8mm in length with gauges of 31G or 32G for Wegovy and Saxenda—which is considerably thinner than needles used for intramuscular injections or blood tests. This fine gauge helps reduce tissue trauma and associated pain. Subcutaneous administration, where medication is delivered into the fatty tissue layer beneath the skin rather than into muscle, further minimises discomfort.
Pain perception varies considerably between individuals due to differences in pain sensitivity, anxiety levels, and previous injection experience. Research indicates that anticipatory anxiety can amplify pain perception, whilst relaxation techniques and proper injection training can substantially reduce discomfort. It is important to distinguish between the brief sensation during needle insertion and potential injection site reactions that may develop afterwards, such as mild redness, swelling, or tenderness. These post-injection symptoms are generally temporary and resolve within a few days without intervention.
Key factors influencing pain experience:
-
Individual pain threshold and anxiety levels
-
Needle size and injection technique
-
Injection site selection and rotation
-
Medication formulation and volume
If you experience any suspected side effects from your medication, you can report these through the MHRA Yellow Card Scheme.
What Causes Discomfort During Weight Loss Injections
Understanding the mechanisms behind injection-related discomfort can help patients manage expectations and adopt strategies to minimise pain. The primary cause of immediate pain during injection is mechanical stimulation of nociceptors (pain receptors) in the skin and subcutaneous tissue as the needle penetrates. The dermis contains the highest concentration of these sensory nerve endings, which explains why the initial skin puncture typically causes the most noticeable sensation.
The volume and pH of the injected medication also influence discomfort levels. GLP-1 receptor agonists are administered in relatively small volumes, which reduces tissue distension and associated pressure-related pain. However, if the medication's pH differs significantly from physiological pH (approximately 7.4), it may cause a brief stinging or burning sensation as it disperses through the tissue. Injection speed matters considerably—rapid administration can cause more discomfort than slow, steady delivery.
Cold medication injected directly from refrigerated storage can cause additional discomfort due to temperature differential. The product information for weight loss injections typically recommends allowing the pen to reach room temperature before administration, as per the specific instructions in your medication's Patient Information Leaflet (PIL). Following these temperature guidelines can substantially reduce injection-related pain. Failure to do so may result in a more pronounced stinging sensation and increased likelihood of injection site reactions.
Common causes of injection discomfort:
-
Needle penetration through pain-sensitive dermis
-
Rapid injection speed causing tissue distension
-
Cold medication temperature
-
Medication pH and formulation characteristics
-
Injection into areas with less subcutaneous fat
-
Reusing injection sites without adequate rotation
Muscle tension at the injection site can also amplify pain perception. Patients who tense their muscles in anticipation of the injection often experience more discomfort than those who remain relaxed. Additionally, injecting into areas with insufficient subcutaneous fat or accidentally hitting small blood vessels can increase pain and bruising risk.
Pain Levels: Comparing Different Injectable Weight Loss Medications
The main injectable weight loss medications licensed in the UK for weight management include semaglutide (Wegovy), liraglutide (Saxenda), and tirzepatide (Mounjaro). These medications have similar delivery methods, though there are differences in formulation, injection frequency, and delivery devices.
Semaglutide (Wegovy) is administered once weekly using a pre-filled, single-dose pen with a fine needle. The weekly dosing schedule means fewer injections overall, which many patients find advantageous. The injection volume is fixed according to the dose pen (0.5ml or 0.75ml depending on the dose). The pen device is designed for ease of use, with a hidden needle that may help reduce anxiety in needle-phobic patients.
Liraglutide (Saxenda) requires daily subcutaneous injection, which means more frequent needle exposure but allows patients to become accustomed to the injection routine more quickly. The pen uses a similar fine-gauge needle, and the injection volume is approximately 0.5ml at the 3.0mg maintenance dose. Some patients report that the daily injection becomes routine and less anxiety-provoking over time, whilst others find the frequency burdensome.
Tirzepatide (Mounjaro) is administered once weekly and features a pre-filled pen. Like other GLP-1 medications, it is designed for subcutaneous injection and uses a fine-gauge needle to minimise discomfort.
Comparative considerations:
-
All licensed weight loss injections use fine-gauge needles designed to minimise discomfort
-
Weekly injections (semaglutide, tirzepatide) mean less frequent needle exposure
-
Daily injections (liraglutide) allow faster habituation to injection routine
-
Pen device design and needle visibility affect psychological comfort
Individual preference often relates more to injection frequency and device design than actual pain levels. Always follow the specific instructions provided with your medication and discuss any concerns with your healthcare provider.
Techniques to Minimise Pain and Injection Site Reactions
Adopting proper injection technique and preparation strategies can substantially reduce both immediate pain and subsequent injection site reactions. Healthcare professionals should provide comprehensive training when initiating weight loss injection therapy, and patients should feel confident in their technique before self-administering at home.
Pre-injection preparation: Allow the medication pen to reach room temperature by removing it from the refrigerator for the time specified in your medication's Patient Information Leaflet (PIL). Cold medication can cause more discomfort and may increase the risk of injection site reactions. Wash hands thoroughly before injection. If your skin is visibly clean, additional cleaning may not be necessary as per NHS guidance, but if recommended in your medication's instructions, clean the injection site with an alcohol wipe and allow the skin to dry completely—injecting through wet alcohol can cause stinging. Select an appropriate injection site with adequate subcutaneous fat: the abdomen (avoiding a 5cm radius around the navel) or front or outer thighs are commonly recommended. Upper arms may be suitable but often require assistance from another person. Rotate injection sites systematically to prevent lipohypertrophy (fatty lumps) and reduce localised irritation.
During injection: Relax the muscles at the injection site—tension increases pain perception. Follow your device's specific instructions regarding skin pinching and injection angle. Generally, pinching the skin gently creates a fold of subcutaneous tissue, which helps ensure the medication is delivered into fat rather than muscle. Insert the needle with a swift, confident motion (hesitation can increase discomfort). Inject slowly and steadily to minimise tissue distension and pressure-related pain. Keep the needle in place after injection for the time specified in your pen's instructions to prevent medication leakage, which can cause skin irritation.
Post-injection care: Withdraw the needle smoothly at the same angle of insertion. Apply gentle pressure with a clean cotton pad if needed, but avoid rubbing the site vigorously, which can increase irritation and bruising risk. Dispose of the used pen or needle safely in a sharps container. You can request a sharps bin from your GP or pharmacy, and follow your local council's guidance for disposal.
Additional pain-reduction strategies:
-
Apply a cold pack (not ice directly) to the injection site for 30-60 seconds before injection to provide temporary numbing
-
Use distraction techniques such as coughing during needle insertion
-
Practice relaxation breathing to reduce anxiety and muscle tension
-
Consider topical anaesthetic cream (discuss with GP) for particularly needle-phobic patients
-
Maintain consistent injection timing to establish routine and reduce anticipatory anxiety
Systematic site rotation is crucial—using the same location repeatedly increases the risk of lipohypertrophy, which can affect medication absorption and cause discomfort. Keep a simple log or use a rotation pattern (e.g., alternating between left and right sides, moving through different anatomical areas weekly).
When to Seek Medical Advice About Injection Pain
Whilst mild, transient discomfort during and immediately after weight loss injections is normal, certain symptoms warrant medical evaluation. Patients should be educated about warning signs that may indicate injection site complications, allergic reactions, or improper injection technique requiring intervention.
Seek prompt GP or prescriber advice if you experience:
-
Severe or worsening pain at the injection site that persists beyond 24-48 hours or intensifies rather than improving
-
Signs of infection including increasing redness spreading beyond the immediate injection site, warmth, swelling, pus or discharge, or fever
-
Significant bruising that is extensive, painful, or accompanied by a hard lump under the skin
-
Allergic reaction symptoms such as widespread rash, hives, facial swelling, difficulty breathing, or rapid heartbeat—these require immediate medical attention via 999 or A&E
-
Persistent lumps or hard areas at injection sites that don't resolve within a few weeks, which may indicate lipohypertrophy
-
Numbness, tingling, or shooting pain radiating from the injection site, suggesting possible nerve irritation
-
Recurrent severe pain with every injection despite proper technique, which may indicate an underlying issue
Injection site reactions can include mild, self-limiting symptoms such as redness, itching, or tenderness. These usually resolve within a few days without treatment. The frequency of these reactions varies by medication and is detailed in each product's SmPC (Summary of Product Characteristics). However, if reactions become progressively worse with subsequent injections or significantly impact quality of life, medical review is appropriate.
Patients experiencing excessive anxiety or needle phobia that prevents adherence to prescribed therapy should discuss this with their healthcare provider. Alternative strategies, including additional injection training, psychological support, or consideration of other weight loss approaches, may be explored. NICE guidance emphasises the importance of patient-centred care and shared decision-making in obesity management.
When to contact your GP or prescriber:
-
Injection site symptoms persisting beyond 3-4 days
-
Concerns about injection technique or medication administration
-
Difficulty adhering to treatment due to pain or anxiety
-
Questions about managing minor injection site reactions
-
Any unexpected or concerning symptoms following injection
Maintaining open communication with your healthcare team ensures optimal treatment outcomes and allows prompt identification and management of any complications. Avoid injecting into areas of broken or irritated skin. Most injection-related concerns can be effectively addressed through technique refinement, site rotation optimisation, or supportive measures, allowing patients to continue benefiting from these evidence-based weight loss therapies.
Frequently Asked Questions
How painful are weight loss injections like Wegovy and Saxenda?
Most patients experience minimal discomfort, typically described as a brief pinch or sting lasting only seconds. The fine needles used (31G–32G) and subcutaneous delivery into fatty tissue help reduce pain compared to other types of injections.
What can I do to reduce pain from weight loss injections?
Allow the medication pen to reach room temperature before injecting, rotate injection sites systematically, relax your muscles during injection, inject slowly and steadily, and consider applying a cold pack to the site for 30–60 seconds beforehand. Proper technique substantially reduces discomfort.
When should I contact my GP about injection site pain?
Seek medical advice if you experience severe or worsening pain persisting beyond 24–48 hours, signs of infection (spreading redness, warmth, pus, fever), significant bruising, allergic reaction symptoms, persistent lumps, or numbness and tingling radiating from the injection site.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










