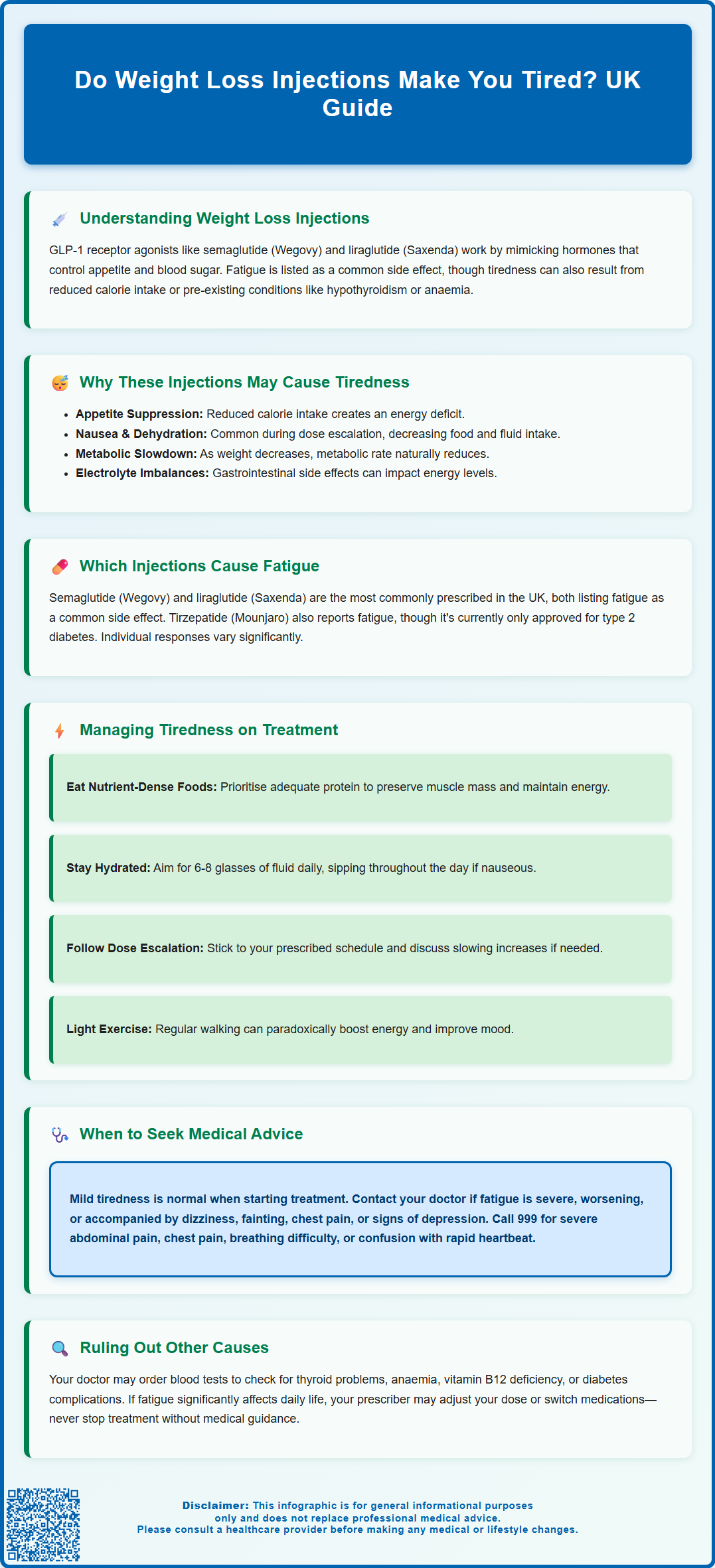
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), are increasingly prescribed for weight management in the UK. Many patients wonder: do weight loss injections make you tired? Fatigue is indeed a recognised adverse reaction with these medications, listed in their Summary of Product Characteristics. The tiredness may stem from the medication itself, reduced calorie intake, gastrointestinal side effects, or metabolic changes during weight loss. Understanding why fatigue occurs and how to manage it effectively can help patients continue treatment safely whilst maintaining quality of life. This article explores the connection between weight loss injections and tiredness, offering practical guidance for UK patients.
Summary: Weight loss injections, particularly GLP-1 receptor agonists like semaglutide and liraglutide, can cause fatigue as a recognised adverse reaction.
- GLP-1 receptor agonists such as Wegovy and Saxenda list fatigue as a common adverse reaction in their Summary of Product Characteristics.
- Tiredness may result from reduced calorie intake, gastrointestinal side effects like nausea, metabolic adaptation during weight loss, or dehydration.
- Gradual dose escalation, adequate nutrition and hydration, and regular physical activity can help manage medication-related fatigue.
- Seek medical advice if fatigue is severe, persistent, worsening, or accompanied by dizziness, chest pain, or signs of dehydration.
- Blood tests may be needed to exclude other causes of tiredness such as thyroid dysfunction, anaemia, or vitamin deficiencies.
Table of Contents
Understanding Weight Loss Injections and Fatigue
Weight loss injections, particularly glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. These medications work by mimicking natural hormones that regulate appetite and blood glucose levels. Fatigue is a commonly reported adverse reaction for these medications, as listed in their Summary of Product Characteristics (SmPC).
In the UK, Wegovy (semaglutide) and Saxenda (liraglutide) are licensed for weight management in adults with a BMI of 30 kg/m² or greater (obesity), or from 27 kg/m² to less than 30 kg/m² (overweight) in the presence of at least one weight-related comorbidity. It's important to note that Ozempic, while containing semaglutide, is not licensed for weight management.
The tiredness experienced during treatment may have multiple causes. Some patients may experience fatigue as a direct medication side effect, while others might feel tired due to reduced calorie intake or changes in eating patterns. Additionally, pre-existing conditions such as hypothyroidism, anaemia, or sleep disorders can contribute to fatigue and should be considered when evaluating tiredness during weight loss treatment. A comprehensive assessment by a healthcare professional can help determine whether fatigue is medication-related or due to other factors requiring separate management.
Why Weight Loss Injections May Cause Tiredness
The mechanisms behind fatigue during weight loss injection therapy are multifactorial. Reduced caloric intake is a significant contributor. GLP-1 receptor agonists work by suppressing appetite and promoting satiety, which naturally leads to decreased food consumption. When calorie intake drops substantially—particularly if the reduction is rapid—the body may experience an energy deficit, manifesting as tiredness or lethargy.
Gastrointestinal adverse effects commonly associated with weight loss injections may also contribute to fatigue. Nausea is very common during dose escalation of GLP-1 therapies according to their SmPCs, and can reduce nutritional intake further and lead to dehydration if accompanied by vomiting. These gastrointestinal symptoms typically occur during dose escalation and may resolve as the body adapts to the medication. However, persistent nausea can result in inadequate nutrition, potentially affecting energy levels.
Metabolic adaptation during weight loss represents another potential mechanism. As body weight decreases, metabolic rate naturally slows—a phenomenon sometimes called adaptive thermogenesis. This metabolic adjustment may contribute to feelings of reduced energy. Additionally, vomiting or diarrhoea can lead to electrolyte imbalances and dehydration, both of which influence energy levels.
For people with diabetes who are also taking insulin or sulfonylureas, hypoglycaemia (low blood sugar) is a risk that can present with symptoms including tiredness and should be monitored carefully. While the exact biological mechanism by which GLP-1 medications directly cause fatigue is not fully elucidated, it remains a recognised adverse reaction in clinical data.
Which Weight Loss Injections Are Most Likely to Cause Fatigue
Among the weight loss injections currently available in the UK, semaglutide (Wegovy) and liraglutide (Saxenda) are the most commonly prescribed GLP-1 receptor agonists for weight management. According to their SmPCs, fatigue is listed as a common adverse reaction for both medications. Individual responses to these medications vary considerably, and the frequency of fatigue may differ between patients.
Tirzepatide (Mounjaro), a dual GIP/GLP-1 receptor agonist approved for type 2 diabetes in the UK, has a similar adverse effect profile to other GLP-1 medications. Fatigue has been reported with tirzepatide use, though the exact frequency may vary from other GLP-1 agonists. At the time of writing, tirzepatide is not yet licensed specifically for weight management in the UK under the brand name Zepbound, though this may change with regulatory updates.
It is worth noting that older weight loss medications such as orlistat (Xenical, Alli) work through entirely different mechanisms—blocking fat absorption rather than affecting appetite hormones—and have different side effect profiles. Fatigue is not typically associated with orlistat use. For patients considering weight loss injections, factors such as starting dose, rate of dose escalation, baseline metabolic health, and concurrent medications all influence whether tiredness occurs. Healthcare professionals typically recommend gradual dose titration to minimise adverse effects, which may also help reduce the likelihood of experiencing significant fatigue during treatment initiation.
Managing Tiredness While Using Weight Loss Injections
If you experience tiredness whilst using weight loss injections, several practical strategies can help manage this symptom effectively. Ensuring adequate nutrition is paramount, even whilst reducing overall calorie intake. Focus on nutrient-dense foods that provide essential vitamins, minerals, and macronutrients. Prioritise lean proteins, whole grains, fruits, vegetables, and healthy fats. Adequate protein intake is particularly important during weight loss to preserve muscle mass and support energy levels. Consider discussing your specific nutritional needs with a registered dietitian, especially if you have conditions such as chronic kidney disease that may require tailored advice.
Maintaining proper hydration is equally crucial. Dehydration can significantly contribute to fatigue and may be exacerbated by gastrointestinal side effects. The NHS recommends 6-8 glasses of fluid daily, adjusting for activity level, climate, and individual needs. If nausea is problematic, try sipping fluids throughout the day rather than drinking large amounts at once. Some patients find that ginger tea or diluted fruit juice helps manage nausea whilst maintaining hydration.
Gradual dose escalation can minimise side effects, including fatigue. Follow your prescriber's titration schedule carefully—rushing to higher doses increases the likelihood of adverse effects. If tiredness is significant, discuss with your healthcare provider whether slowing the dose increase might be appropriate. Regular physical activity, even light exercise such as walking, can paradoxically improve energy levels by enhancing cardiovascular fitness and mood. Start with manageable amounts and gradually increase intensity as tolerated.
Sleep hygiene should not be overlooked. Ensure you're getting 7–9 hours of quality sleep nightly, as inadequate rest will compound any medication-related tiredness. If you're considering vitamin supplementation, discuss this with your healthcare provider first. Blood tests may be needed to identify specific deficiencies before starting supplements. The NHS does recommend that adults consider taking a daily supplement containing 10 micrograms of vitamin D during autumn and winter months.
When to Seek Medical Advice About Fatigue
Whilst mild tiredness during the initial weeks of weight loss injection therapy may be expected as your body adjusts, certain situations warrant prompt medical review. Contact your GP or prescribing clinician if:
-
Fatigue is severe, persistent, or progressively worsening despite self-management strategies
-
Tiredness is accompanied by dizziness, fainting, or significant weakness
-
You experience symptoms suggesting dehydration (dark urine, dry mouth, reduced urination)
-
Fatigue occurs alongside chest pain, shortness of breath, or palpitations
-
You notice signs of depression, such as persistent low mood, loss of interest in activities, or changes in sleep patterns beyond simple tiredness
-
Gastrointestinal symptoms (nausea, vomiting, diarrhoea) are severe or preventing adequate nutrition and hydration
For urgent advice when your GP is unavailable, call NHS 111. Seek immediate medical attention by calling 999 or going to A&E if you develop symptoms of pancreatitis (severe, persistent abdominal pain radiating to the back), severe chest pain, severe shortness of breath, or signs of severe dehydration (confusion, rapid heartbeat, very low urine output).
People with diabetes should be particularly vigilant for symptoms of hypoglycaemia (sweating, dizziness, confusion, hunger), which can also present as tiredness, especially if taking insulin or sulfonylureas alongside GLP-1 medications.
Your healthcare provider may recommend blood tests to exclude other causes of fatigue, including thyroid dysfunction, anaemia, vitamin B12 deficiency, or diabetes-related complications. If fatigue significantly impairs your quality of life or daily functioning, your prescriber may consider adjusting the dose, temporarily down-titrating, or switching to an alternative medication. Do not stop treatment abruptly without medical advice.
If you suspect your fatigue is a side effect of your medication, report it through the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app. This helps authorities monitor medication safety.
Frequently Asked Questions
How long does fatigue from weight loss injections typically last?
Fatigue often occurs during the initial weeks of treatment or during dose escalation and may improve as your body adjusts to the medication. If tiredness persists beyond several weeks or worsens, consult your healthcare provider to exclude other causes and discuss management strategies.
Can I continue exercising if I feel tired on weight loss injections?
Light to moderate physical activity such as walking can actually improve energy levels and is generally encouraged during treatment. Start with manageable amounts and gradually increase intensity as tolerated, ensuring you maintain adequate nutrition and hydration to support your activity level.
Should I stop my weight loss injection if I feel very tired?
Do not stop treatment abruptly without medical advice. If fatigue is severe or significantly affecting your daily life, contact your prescribing clinician who may adjust your dose, slow the titration schedule, or investigate other potential causes of tiredness through blood tests or clinical assessment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript