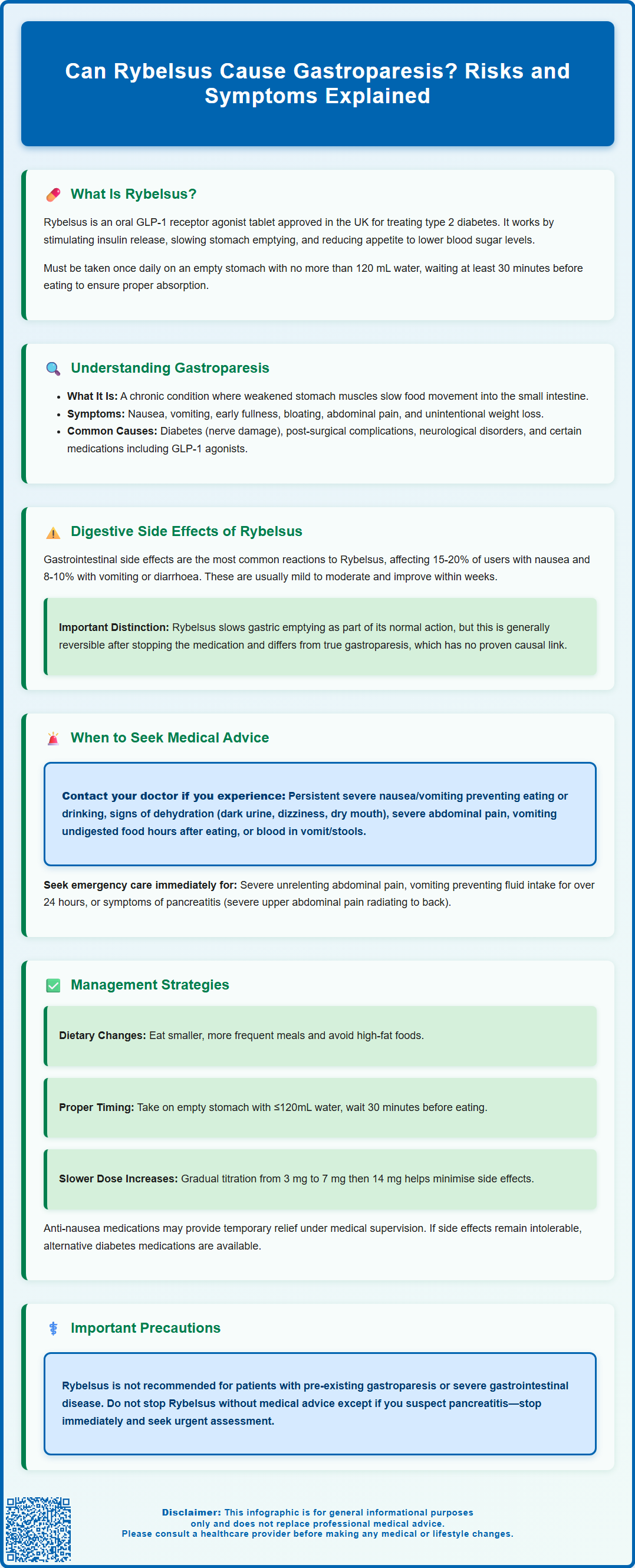
Rybelsus (semaglutide) is an oral GLP-1 receptor agonist licensed in the UK for type 2 diabetes management. Whilst gastrointestinal side effects such as nausea and delayed gastric emptying are common and expected with this medication, patients and clinicians often question whether Rybelsus can cause gastroparesis—a chronic condition characterised by impaired stomach emptying. Understanding the distinction between therapeutic gastric slowing and true gastroparesis is essential for safe prescribing and patient counselling. This article examines the evidence, explores digestive side effects, and provides guidance on when medical review is warranted.
Summary: Rybelsus pharmacologically slows gastric emptying as part of its therapeutic mechanism, but a causal relationship with true gastroparesis has not been established, though rare post-marketing reports exist.
- Rybelsus (semaglutide) is an oral GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment.
- The medication deliberately slows gastric emptying to improve glycaemic control and reduce appetite.
- Common gastrointestinal side effects include nausea, vomiting, and abdominal discomfort, typically resolving within weeks.
- Rybelsus is not recommended for patients with pre-existing severe gastroparesis or severe gastrointestinal disease.
- Persistent severe symptoms such as unrelenting vomiting, dehydration, or severe abdominal pain require urgent medical assessment.
- Regulatory authorities continue to monitor potential associations between GLP-1 receptor agonists and persistent gastric motility problems.
Table of Contents
What Is Rybelsus and How Does It Work?
Rybelsus (semaglutide) is an oral medication approved in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists. Rybelsus is available as a tablet formulation, offering an alternative to injectable GLP-1 therapies such as Ozempic (also semaglutide).
The mechanism of action centres on mimicking the naturally occurring hormone GLP-1, which is released by the intestine in response to food intake. Semaglutide works by:
-
Stimulating insulin secretion from pancreatic beta cells in a glucose-dependent manner, which helps lower blood sugar levels without causing hypoglycaemia when glucose levels are normal
-
Suppressing glucagon release, thereby reducing hepatic glucose production
-
Slowing gastric emptying, which prolongs the time food remains in the stomach and contributes to improved glycaemic control
-
Reducing appetite through central nervous system effects, leading to decreased caloric intake and potential weight loss
Rybelsus must be taken once daily in the morning on an empty stomach with no more than 120 mL of water. Patients should wait at least 30 minutes before consuming food, drink or other oral medicines to ensure proper absorption.
Treatment is typically initiated at a low dose (3 mg once daily) and titrated upwards (7 mg, then 14 mg) to balance efficacy with tolerability. The MHRA-approved indication includes use as monotherapy when metformin is inappropriate, or in combination with other glucose-lowering medications. It is not licensed for weight loss in the UK.
Importantly, Rybelsus is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis. When used with insulin or sulfonylureas, there is an increased risk of hypoglycaemia, and dose adjustments of these medications may be necessary. Rybelsus may affect the absorption of other oral medicines and can increase levothyroxine exposure, requiring thyroid function monitoring.
Understanding Gastroparesis: Symptoms and Causes
Gastroparesis, also known as delayed gastric emptying, is a chronic condition characterised by impaired movement of food from the stomach into the small intestine without any mechanical obstruction. The stomach's muscular contractions become weakened or uncoordinated, resulting in prolonged retention of gastric contents.
Common symptoms of gastroparesis include:
-
Persistent nausea and vomiting, particularly of undigested food
-
Early satiety (feeling full after eating only small amounts)
-
Postprandial fullness and bloating
-
Upper abdominal pain or discomfort
-
Gastro-oesophageal reflux
-
Poor appetite and unintentional weight loss
-
Fluctuating blood glucose levels in people with diabetes
The condition can significantly impact quality of life and nutritional status. In severe cases, it may lead to dehydration, malnutrition, and unpredictable glycaemic control in diabetic patients.
Established causes of gastroparesis include diabetes mellitus (diabetic autonomic neuropathy affecting the vagus nerve), post-surgical complications (particularly following gastric or oesophageal surgery), neurological disorders such as Parkinson's disease, connective tissue diseases like scleroderma, and certain medications (including opioids, anticholinergics, tricyclic antidepressants, and GLP-1 receptor agonists). However, in many cases, no identifiable cause is found, termed idiopathic gastroparesis.
According to British Society of Gastroenterology (BSG) guidance, diagnosis typically involves excluding mechanical obstruction (via endoscopy or imaging) followed by gastric emptying studies. The standard test is a 4-hour solid meal gastric emptying scintigraphy, where patients consume a radiolabelled meal and imaging tracks how quickly the stomach empties. Investigation should be considered in patients with persistent upper gastrointestinal symptoms, particularly those with diabetes experiencing erratic glycaemic control.
Patients with concerning symptoms such as dysphagia at any age, or those aged 55 and over with weight loss and upper abdominal pain, reflux or dyspepsia should be referred urgently to exclude upper GI malignancy, in line with NICE guidance (NG12).
Digestive Side Effects of Rybelsus: What to Expect
Gastrointestinal side effects are the most commonly reported adverse reactions with Rybelsus and other GLP-1 receptor agonists. These effects are directly related to the drug's mechanism of slowing gastric emptying and are typically most pronounced during dose initiation and escalation.
Expected digestive side effects include:
-
Nausea (reported in 15–20% of patients in clinical trials)
-
Vomiting and diarrhoea (each affecting approximately 8–10% of users)
-
Abdominal pain and discomfort
-
Decreased appetite
-
Constipation
-
Dyspepsia and gastro-oesophageal reflux
These symptoms are usually mild to moderate in severity and tend to diminish over time as the body adapts to the medication. Most patients experience improvement within several weeks of maintaining a stable dose. The gradual dose titration protocol is specifically designed to minimise these gastrointestinal effects.
However, an important distinction must be made between expected, transient side effects and true gastroparesis. Whilst Rybelsus pharmacologically slows gastric emptying as part of its therapeutic action, a causal relationship with true gastroparesis has not been established. There are rare post-marketing reports of persistent gastric motility problems, and regulatory authorities continue to monitor this potential association. The delayed gastric emptying induced by GLP-1 receptor agonists is generally reversible upon discontinuation of the medication, though recovery time varies between individuals.
Patients should be aware of additional safety considerations with Rybelsus:
-
Risk of pancreatitis: persistent severe abdominal pain requires urgent medical assessment and treatment interruption
-
Increased risk of gallbladder disease, including cholelithiasis and cholecystitis
-
Potential for dehydration and acute kidney injury with prolonged vomiting or diarrhoea
-
Increased hypoglycaemia risk when used with insulin or sulfonylureas
Patients with pre-existing gastroparesis or severe gastrointestinal disease were typically excluded from clinical trials, and the SmPC states that Rybelsus is not recommended in these populations.
When to Seek Medical Advice About Rybelsus and Stomach Problems
Whilst mild gastrointestinal symptoms are common and expected with Rybelsus, certain warning signs warrant prompt medical evaluation. Patients should be educated about when digestive symptoms require professional assessment rather than simple observation.
Contact your GP or diabetes specialist nurse if you experience:
-
Persistent or severe nausea and vomiting that prevents adequate fluid or food intake
-
Signs of dehydration, including reduced urination, dark urine, dizziness, or dry mouth
-
Severe abdominal pain, particularly if constant or worsening
-
Vomiting of undigested food several hours after eating
-
Unexplained weight loss beyond expected therapeutic effects
-
Blood in vomit or black, tarry stools
-
Difficulty swallowing or sensation of food getting stuck
Seek immediate medical attention (A&E, NHS 111, or call 999) if:
-
You experience severe, unrelenting abdominal pain
-
You have persistent vomiting preventing any fluid intake for more than 24 hours
-
You develop signs of severe dehydration or altered consciousness
-
You experience symptoms suggestive of pancreatitis (severe upper abdominal pain radiating to the back)
For patients with diabetes, erratic blood glucose control despite usual management may indicate impaired gastric emptying affecting carbohydrate absorption and insulin timing. This requires discussion with your diabetes care team to adjust treatment regimens appropriately.
It is also important to report gastrointestinal symptoms that, whilst not severe, significantly impact quality of life or persist beyond the initial adjustment period (typically 4–8 weeks). Your healthcare provider can assess whether dose adjustment, additional supportive measures, or alternative treatments might be more appropriate.
Do not stop taking Rybelsus without medical advice unless you suspect pancreatitis—in which case, stop the medication and seek urgent medical assessment.
If you experience any suspected side effects from Rybelsus, you can report them directly to the MHRA through the Yellow Card Scheme at yellowcard.mhra.gov.uk. This helps regulators monitor medication safety.
Alternatives and Management Strategies for GLP-1 Side Effects
For patients experiencing troublesome gastrointestinal effects with Rybelsus, several management strategies and alternative options exist. The approach should be individualised based on symptom severity, diabetes control, and patient preferences.
Strategies to minimise GLP-1-related digestive symptoms:
-
Dietary modifications: Eating smaller, more frequent meals; avoiding high-fat foods that delay gastric emptying further; limiting fibre if experiencing bloating; ensuring adequate hydration
-
Timing adjustments: Taking Rybelsus correctly—in the morning on an empty stomach with no more than 120 mL water, waiting at least 30 minutes before eating, drinking or taking other oral medicines
-
Slower dose titration: Remaining at lower doses for longer periods before escalating
-
Symptomatic relief: Anti-emetics may provide temporary relief under medical supervision:
- Metoclopramide: MHRA restricts use to short-term only (usually ≤5 days) due to risk of neurological side effects
- Domperidone: Has restricted indications and requires ECG monitoring due to QT prolongation risk
-
Ondansetron: May be considered for severe nausea
-
Proton pump inhibitors: May help if reflux symptoms are prominent
Alternative diabetes medications should be considered if gastrointestinal side effects remain intolerable despite optimisation strategies. According to NICE guidance (NG28) for type 2 diabetes management, options include:
-
Other GLP-1 receptor agonists: Some patients may tolerate different formulations better, though similar GI effects often occur across the class; weekly injectable semaglutide, dulaglutide or tirzepatide may be options
-
SGLT2 inhibitors: Offer cardiovascular and renal benefits with different mechanisms and side effect profiles
-
DPP-4 inhibitors: Generally well-tolerated with minimal gastrointestinal effects, though less potent for weight reduction
-
Insulin therapy: Particularly if beta-cell function is significantly impaired
-
Combination approaches: Adjusting doses of existing medications or adding complementary agents
For patients with pre-existing gastroparesis or severe gastrointestinal disorders, GLP-1 receptor agonists are not recommended according to the SmPC. Alternative therapeutic pathways should be prioritised. Regular review with diabetes specialist teams ensures treatment remains aligned with individual needs, tolerability, and glycaemic targets whilst maintaining quality of life.
Patients taking levothyroxine or warfarin with Rybelsus should have thyroid function or INR monitored, respectively, as Rybelsus may affect absorption of these medications.
Frequently Asked Questions
Does Rybelsus slow down stomach emptying?
Yes, Rybelsus deliberately slows gastric emptying as part of its therapeutic mechanism to improve blood glucose control and reduce appetite. This is an expected pharmacological effect rather than a disease state, though it can cause gastrointestinal symptoms.
What are the warning signs that Rybelsus is causing serious stomach problems?
Seek medical attention if you experience persistent severe vomiting preventing fluid intake, signs of dehydration, severe unrelenting abdominal pain, vomiting undigested food hours after eating, blood in vomit, or difficulty swallowing. These symptoms require professional assessment.
Can I take Rybelsus if I already have gastroparesis?
No, Rybelsus is not recommended for patients with pre-existing severe gastroparesis or severe gastrointestinal disease according to the Summary of Product Characteristics. Alternative diabetes treatments should be considered in consultation with your healthcare team.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript