Ozempic (semaglutide), a GLP-1 receptor agonist used for type 2 diabetes and weight management, commonly causes constipation by slowing gastrointestinal motility. Choosing the best laxative to take with Ozempic requires understanding both the medication's effects and safe, evidence-based treatment options. According to NICE guidance, macrogol is typically recommended as first-line therapy for chronic constipation in adults, offering effective relief with a favourable safety profile. This article explores laxative choices, selection criteria, and lifestyle strategies to support bowel health while taking Ozempic, ensuring safe and coordinated care for patients experiencing this common side effect.
Summary: Macrogol (such as Movicol or Laxido) is generally recommended as the first-line laxative for constipation in patients taking Ozempic.
- Macrogol is an osmotic laxative that draws water into the bowel to soften stools and is recommended by NICE as first-line treatment for chronic constipation in adults
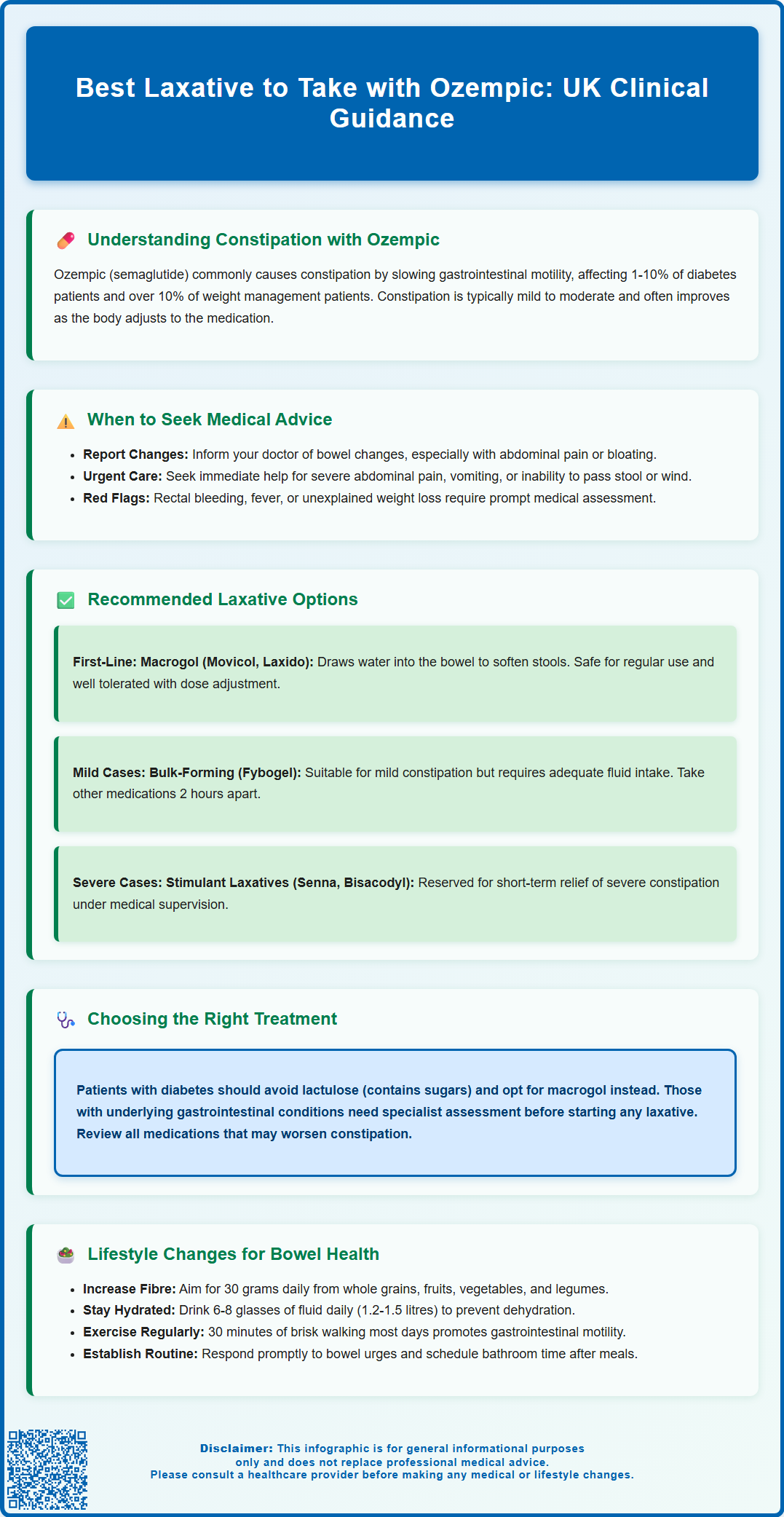
- Constipation affects 1-10% of Ozempic users and over 10% of Wegovy users, caused by semaglutide's effect on gastrointestinal motility
- Bulk-forming laxatives like ispaghula husk may suit mild constipation but require adequate fluid intake to prevent obstruction
- Stimulant laxatives such as senna or bisacodyl provide short-term relief for severe constipation and should be used under medical supervision
- No specific laxative interactions with Ozempic are documented, but patients should inform healthcare providers of all medications taken
- Persistent or severe constipation, abdominal pain, vomiting, or inability to pass stool requires urgent medical assessment
Table of Contents
Understanding Constipation with Ozempic
Constipation is a commonly reported adverse effect among patients taking semaglutide. According to the Summary of Product Characteristics (SmPC), constipation is classified as 'common' with Ozempic (affecting 1-10% of patients) and 'very common' with Wegovy (affecting more than 10% of patients). The mechanism underlying constipation relates to the medication's effect on gastrointestinal motility. By influencing the movement of food through the digestive tract, semaglutide can reduce the frequency and ease of bowel movements.
It is important to recognise that constipation associated with semaglutide is typically mild to moderate in severity and often improves with time as the body adjusts to the medication. Gastrointestinal side effects frequently occur during initiation or dose escalation and may improve with slower titration as per the SmPC guidance. However, persistent or severe constipation warrants medical review, as it may indicate inadequate management or, rarely, more serious gastrointestinal complications.
Patients should be encouraged to report bowel habit changes to their GP or diabetes specialist nurse, particularly if accompanied by abdominal pain, bloating, or rectal bleeding. Urgent medical assessment should be sought for severe, persistent abdominal pain, vomiting, inability to pass stool or gas (possible obstruction), or symptoms suggesting pancreatitis or gallbladder disease. Understanding the relationship between Ozempic and bowel function is the first step in implementing effective management strategies.
Safe Laxative Options for Ozempic Users
When lifestyle measures alone are insufficient to manage constipation in patients taking Ozempic, laxatives may be considered as an adjunctive treatment. The choice of laxative should be guided by the individual's clinical circumstances, the severity of constipation, and any contraindications. In the UK, several classes of laxatives are available over the counter or on prescription, each with distinct mechanisms of action and safety profiles.
According to NICE Clinical Knowledge Summaries (CKS) and the British National Formulary (BNF), macrogol (e.g., Movicol, Laxido) is usually recommended as first-line treatment for chronic constipation in adults. These osmotic laxatives draw water into the bowel, softening stools and promoting evacuation. Macrogol is generally well tolerated, though patients with renal impairment or heart failure should be aware of the electrolyte and sodium content of some preparations. These agents are safe for regular use in most patients.
Bulk-forming laxatives, such as ispaghula husk (Fybogel) and methylcellulose, may be suitable for mild, intermittent constipation. These agents work by absorbing water in the intestinal lumen, increasing stool bulk and stimulating peristalsis. They are well tolerated but require adequate fluid intake to prevent intestinal obstruction. Importantly, bulk-forming laxatives should be avoided in patients with suspected bowel obstruction or faecal impaction, and they may impede the absorption of concomitant oral medicines, which should be taken at least 2 hours apart.
Stimulant laxatives, such as senna and bisacodyl, act by stimulating colonic motility and are useful for short-term relief of more severe constipation. While generally recommended for short-term use, some patients may require longer-term treatment under medical supervision. Stool softeners like docusate sodium have limited evidence for efficacy but may be considered as an adjunct when stools are particularly hard.
There is no official evidence suggesting that any specific laxative interacts adversely with Ozempic, but patients should always inform their healthcare provider of all medications and supplements they are taking to ensure safe and coordinated care.
How to Choose the Right Laxative
Selecting the most appropriate laxative for a patient taking Ozempic requires a comprehensive assessment of the individual's bowel symptoms, medical history, and treatment goals. The first consideration is the severity and duration of constipation. For chronic constipation, NICE CKS recommends macrogol as the first-line treatment for most adults, with bulk-forming agents as an alternative when appropriate.
For patients with moderate constipation, osmotic laxatives such as macrogol are particularly effective in softening stools and increasing bowel movement frequency. Macrogol is well evidenced in clinical practice and generally well tolerated, though some patients may experience abdominal cramping or bloating, especially during the initial days of treatment. Dose titration according to response is advisable, and patients should be reviewed regularly to assess efficacy and tolerability.
Bulk-forming laxatives may be suitable for mild, intermittent symptoms in patients who can maintain adequate fluid intake. These agents should be used with caution in immobile patients or those with dysphagia due to the risk of oesophageal or intestinal obstruction if taken with insufficient fluid.
In cases of severe or refractory constipation, a short course of a stimulant laxative may be warranted, but this should be used judiciously and under medical supervision. Patients with underlying gastrointestinal conditions, such as inflammatory bowel disease or intestinal obstruction, require specialist assessment before initiating laxative therapy.
It is also important to review any medications that may contribute to constipation, such as opioids, anticholinergics, or iron supplements. For patients experiencing significant gastrointestinal symptoms with semaglutide, temporary dose adjustment or slower titration may be considered in line with the SmPC guidance.
Regarding specific considerations, patients with diabetes should be aware that lactulose solution contains galactose and lactose which may theoretically affect blood glucose levels, although systemic absorption is minimal. Macrogol is generally preferred in this population. Those with swallowing difficulties may prefer liquid formulations, while others may find sachets or tablets more convenient. Shared decision-making, informed by clinical evidence and patient values, is essential to optimise outcomes and adherence.
Lifestyle Changes to Support Bowel Health
While laxatives can provide symptomatic relief, addressing the underlying causes of constipation through lifestyle modification is fundamental to long-term bowel health, particularly for patients on Ozempic. Dietary fibre intake is a cornerstone of constipation management. The NHS recommends that adults consume approximately 30 grams of fibre daily, obtained from sources such as whole grains, fruits, vegetables, legumes, nuts, and seeds. Increasing fibre gradually helps to avoid excessive bloating and allows the gastrointestinal tract to adapt.
Adequate hydration is equally critical, especially when using bulk-forming laxatives or increasing dietary fibre. The NHS advises aiming for 6-8 glasses of fluid daily (about 1.2-1.5 litres), adjusted for individual factors such as activity levels, climate, and health conditions. Dehydration can exacerbate constipation and reduce the efficacy of many laxative agents. Patients taking Ozempic may experience reduced appetite and thirst, so proactive hydration strategies should be encouraged.
Regular physical activity has been shown to promote gastrointestinal motility and improve bowel regularity. Even moderate exercise, such as brisk walking for 30 minutes most days of the week, can have beneficial effects. Patients should be supported to incorporate physical activity into their daily routine in a manner that is safe and sustainable, taking into account any comorbidities or mobility limitations.
Establishing a regular bowel routine is also helpful. Patients should be advised to respond promptly to the urge to defecate and to allocate sufficient time for bowel movements, ideally after meals when the gastrocolic reflex is most active. Stress management and adequate sleep are additional factors that can influence bowel function and overall wellbeing.
Patients should be advised to contact their GP if constipation persists despite these measures. Urgent medical attention should be sought for sudden severe abdominal pain, persistent vomiting, inability to pass stool or wind, or fever. Additionally, symptoms such as unexplained weight loss, rectal bleeding, or a significant change in bowel habit (especially in those over 50) may warrant investigation for more serious conditions in line with NICE guidance on suspected cancer recognition and referral. A holistic approach that combines appropriate laxative use with sustainable lifestyle changes offers the best prospect for maintaining bowel health while benefiting from Ozempic therapy.
Frequently Asked Questions
Why does Ozempic cause constipation?
Ozempic (semaglutide) slows gastric emptying and reduces gastrointestinal motility as part of its mechanism of action, which can decrease bowel movement frequency and cause constipation in 1-10% of users.
Can I take laxatives long-term while on Ozempic?
Macrogol is safe for regular, long-term use in most patients and is recommended by NICE for chronic constipation. Stimulant laxatives should generally be used short-term, though some patients may require longer treatment under medical supervision.
When should I see a doctor about constipation on Ozempic?
Seek urgent medical attention for severe abdominal pain, persistent vomiting, inability to pass stool or gas, rectal bleeding, or symptoms suggesting bowel obstruction. Contact your GP if constipation persists despite lifestyle changes and laxatives.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












