Constipation is a common gastrointestinal side effect experienced by patients taking Ozempic (semaglutide) for type 2 diabetes mellitus. This occurs because semaglutide slows gastric emptying as part of its mechanism of action, which can lead to harder, less frequent stools. Whilst lifestyle modifications such as increased hydration and dietary fibre are first-line measures, stool softeners and laxatives may be necessary for effective symptom relief. This article explores the safest and most appropriate stool softeners to use alongside Ozempic, including docusate sodium, macrogol, and lactulose, and provides guidance on selecting the right option based on individual patient needs and clinical considerations.
Summary: Macrogol (polyethylene glycol) and docusate sodium are generally considered the safest and most effective stool softeners for patients taking Ozempic, with macrogol often preferred for regular use due to its efficacy and lack of dependency risk.
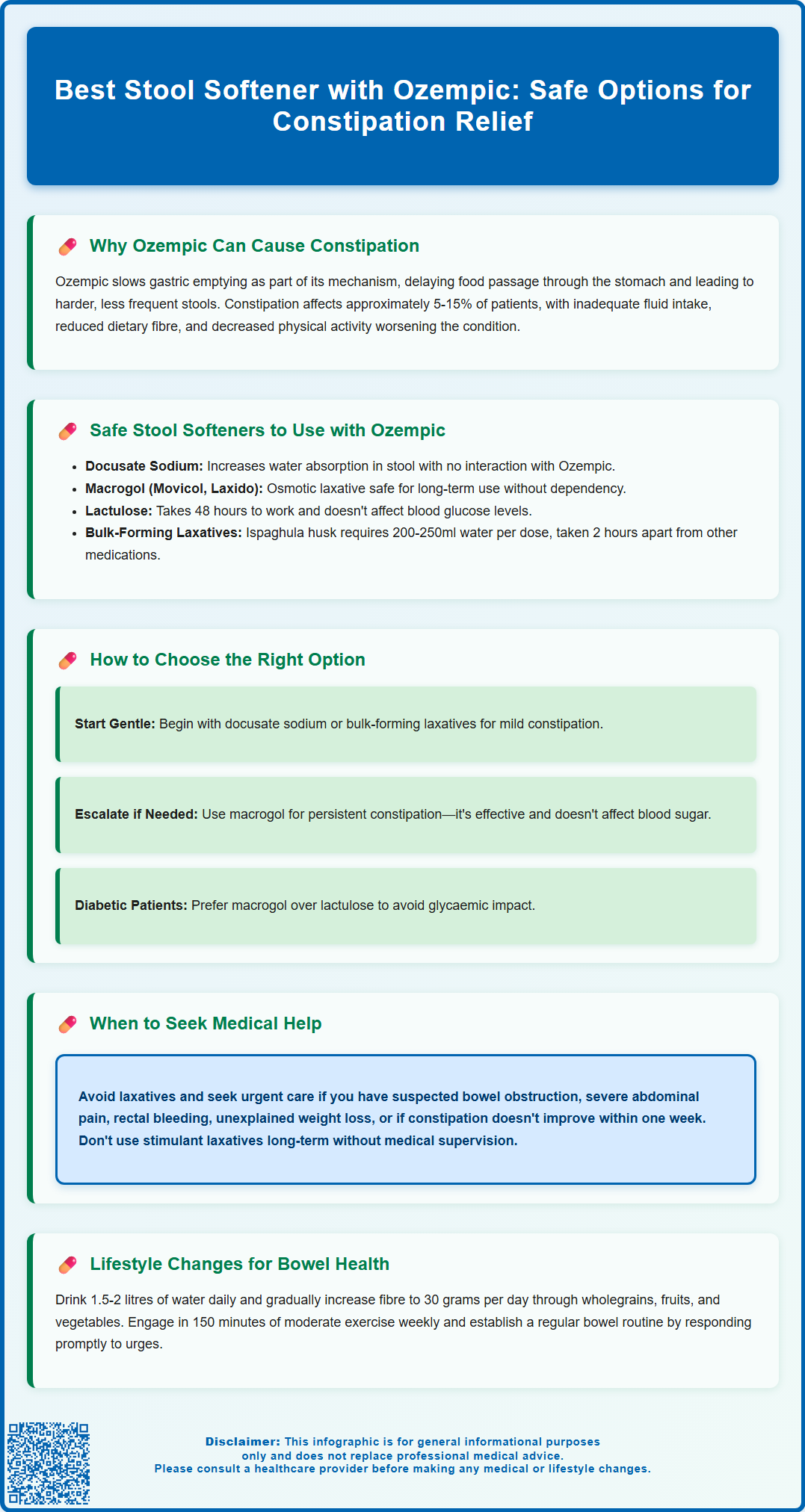
- Ozempic causes constipation in approximately 5–15% of patients by slowing gastric emptying as part of its GLP-1 receptor agonist mechanism.
- Docusate sodium increases water absorption in stools and has no known interaction with semaglutide administered by injection.
- Macrogol (Movicol, Laxido) is an osmotic laxative suitable for long-term use without causing dependency and is widely recommended in NHS practice.
- Bulk-forming laxatives such as ispaghula husk require adequate fluid intake (at least 200–250ml per dose) and should be separated from other oral medicines by 2 hours.
- Persistent or severe constipation, red flag symptoms (rectal bleeding, severe pain, unexplained weight loss), or suspected bowel obstruction require urgent medical review.
Table of Contents
Why Ozempic Can Cause Constipation
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. A different semaglutide formulation (Wegovy) is licensed for weight management. Whilst Ozempic offers significant benefits in glycaemic control, gastrointestinal side effects are amongst the most commonly reported adverse reactions.
Constipation occurs primarily because semaglutide slows gastric emptying as part of its mechanism of action. By mimicking the naturally occurring GLP-1 hormone, Ozempic delays the passage of food through the stomach, which helps regulate blood glucose levels and promotes satiety. This delayed gastric emptying can lead to harder, less frequent stools, particularly during dose escalation or in individuals with pre-existing bowel concerns.
According to the Ozempic Summary of Product Characteristics, constipation affects approximately 5-15% of patients, though the incidence varies with dosage. Factors such as inadequate fluid intake, reduced dietary fibre, and decreased physical activity—often associated with the appetite suppression caused by Ozempic—can further exacerbate constipation. Additionally, some patients may experience nausea or reduced food intake, inadvertently limiting fibre consumption.
It is important to recognise that whilst constipation is an expected side effect for some users, persistent or severe symptoms warrant medical review. Severe gastrointestinal symptoms may lead to dehydration, which requires particular attention. Patients should be advised to maintain adequate hydration, monitor bowel habits and report any significant changes, abdominal pain, or signs of bowel obstruction to their GP or diabetes specialist nurse promptly.
Suspected side effects can be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Safe Stool Softeners to Use with Ozempic
When lifestyle measures alone are insufficient, stool softeners and laxatives can provide effective symptomatic relief. In the UK, several options are available over the counter and are generally considered safe for use alongside Ozempic, though patients should always consult their GP or pharmacist before starting any new medication.
Docusate sodium is a commonly recommended stool softener that works by increasing the amount of water absorbed by the stool, making it softer and easier to pass. It has no known interaction with semaglutide (which is administered by injection). Docusate is available in capsule or liquid form and is suitable for short- to medium-term use.
Macrogol (polyethylene glycol), such as Movicol or Laxido, is an osmotic laxative that draws water into the bowel, softening the stool and stimulating bowel movements. It is widely used in the NHS and is particularly effective for faecal loading or impaction. Macrogol is generally safe for prolonged use and does not cause dependency, making it a practical choice for patients on long-term Ozempic therapy. Some macrogol preparations contain electrolytes, so patients on salt restriction or with heart failure should check with their pharmacist.
Lactulose, another osmotic laxative, is a synthetic sugar that works similarly by increasing stool water content. It may take 48 hours to produce an effect and can cause bloating or flatulence in some individuals. Lactulose is not absorbed into the bloodstream, so it generally does not affect blood glucose levels, though preparations contain sugars and diabetic patients may wish to monitor their glucose levels initially.
Bulk-forming laxatives such as ispaghula husk (Fybogel) or methylcellulose can also be beneficial, particularly for hard stools. These agents increase stool bulk and stimulate peristalsis, though adequate fluid intake is essential to prevent worsening constipation. There is no known contraindication to using these agents with Ozempic, but patients should ensure they drink plenty of water (at least 200-250ml per dose) and separate bulk-forming laxatives from other oral medicines by at least 2 hours to avoid reduced absorption.
Stimulant laxatives like senna or bisacodyl are generally reserved for short-term use or when other measures have failed, as prolonged use may lead to dependency or electrolyte disturbances such as hypokalaemia.
How to Choose the Right Stool Softener
Selecting an appropriate stool softener depends on several factors, including the severity and duration of constipation, individual patient characteristics, and any co-existing medical conditions. A stepwise approach is recommended, starting with the gentlest option and escalating as needed.
For mild, occasional constipation, docusate sodium or a bulk-forming laxative may suffice. These agents are gentle, well tolerated, and suitable for initial management. Patients should be advised to take bulk-forming laxatives with adequate fluids (at least 200–250 ml per dose) to avoid oesophageal or intestinal obstruction, and to separate them from other oral medicines by at least 2 hours.
If constipation persists or is more troublesome, osmotic laxatives such as macrogol are often the next step. According to NICE Clinical Knowledge Summaries, the choice of laxative should be based on stool consistency, with macrogol commonly used and particularly effective for faecal loading. It can be used regularly and adjusted according to response, making it suitable for patients on long-term Ozempic therapy.
Patients with diabetes should be aware that while lactulose is not absorbed into the bloodstream, preparations contain sugars and monitoring blood glucose initially may be prudent. Macrogol is often preferred in this population as it does not affect glycaemic control.
Special considerations include renal or hepatic impairment, where certain laxatives may require dose adjustment or avoidance. Some macrogol preparations with electrolytes contain sodium, which should be considered for patients on salt restriction or with heart failure. Patients with suspected bowel obstruction, inflammatory bowel disease, or severe abdominal pain should avoid laxatives and seek urgent medical advice.
It is also important to consider patient preference and lifestyle. Some individuals may prefer sachets that can be dissolved in water, whilst others may find capsules more convenient. Discussing these preferences with a pharmacist can improve adherence and outcomes.
Patients should be counselled to avoid long-term use of stimulant laxatives without medical supervision, as these can lead to tolerance and colonic atony. If constipation does not improve within a week of appropriate laxative use, or if red flag symptoms develop (such as rectal bleeding, unexplained weight loss, or severe pain), urgent medical review is essential.
Lifestyle Changes to Support Bowel Health on Ozempic
Whilst pharmacological interventions can be effective, lifestyle modifications form the cornerstone of managing constipation in patients taking Ozempic. These measures not only alleviate symptoms but also support overall metabolic and cardiovascular health.
Adequate hydration is paramount. Patients should aim for at least 1.5 to 2 litres of fluid daily, unless contraindicated by other medical conditions. Water, herbal teas, and diluted fruit juices are suitable options. Dehydration exacerbates constipation by allowing the colon to absorb more water from the stool, making it harder and more difficult to pass.
Dietary fibre intake should be gradually increased to 30 grams per day, in line with UK recommendations. Good sources include wholegrain cereals, oats, fruits (especially prunes, apples, and pears), vegetables, pulses, and nuts. Patients should be advised to increase fibre intake slowly to minimise bloating and discomfort. It is important to note that some individuals on Ozempic may experience reduced appetite or nausea, which can make dietary changes challenging; small, frequent meals rich in fibre may be better tolerated.
Regular physical activity stimulates bowel motility and is strongly encouraged. Even moderate exercise, such as a 30-minute daily walk, can significantly improve bowel function. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity per week for adults, which also supports weight management and glycaemic control.
Establishing a regular bowel routine can be helpful. Patients should be encouraged to respond promptly to the urge to defecate and to allow adequate time in the bathroom without straining. The gastrocolic reflex is strongest after meals, so attempting to open the bowels after breakfast may be beneficial. Using a footstool to raise the knees above hip level and leaning slightly forward can help achieve a more effective position for bowel emptying.
Monitoring and communication with healthcare professionals is essential. Patients should keep a symptom diary if constipation is persistent and discuss any concerns during routine diabetes reviews. If lifestyle measures and over-the-counter laxatives are insufficient, prescription options or specialist referral may be warranted. Red flag symptoms—including severe abdominal pain, rectal bleeding, unintentional weight loss, or a significant change in bowel habit—require prompt medical assessment to exclude serious underlying pathology.
Patients are encouraged to report any suspected side effects of Ozempic via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Can I take docusate sodium with Ozempic?
Yes, docusate sodium is generally safe to use with Ozempic as it has no known interaction with semaglutide. It works by softening stools and is suitable for short- to medium-term use, though you should consult your GP or pharmacist before starting any new medication.
Why does Ozempic cause constipation?
Ozempic slows gastric emptying as part of its mechanism to regulate blood glucose and promote satiety. This delayed passage of food through the digestive system can lead to harder, less frequent stools, particularly during dose escalation or in patients with pre-existing bowel concerns.
When should I see a doctor about constipation whilst taking Ozempic?
You should seek urgent medical advice if you experience severe abdominal pain, rectal bleeding, unexplained weight loss, signs of bowel obstruction, or if constipation does not improve within a week of appropriate laxative use. Persistent or worsening symptoms warrant prompt medical review.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript