Choosing the best fibre supplement whilst taking GLP-1 medications such as semaglutide (Ozempic, Wegovy) or liraglutide (Saxenda, Victoza) requires careful consideration of digestive tolerance and individual needs. GLP-1 receptor agonists slow gastric emptying and reduce appetite, which can lead to constipation—a very common side effect affecting more than 1 in 10 people on higher doses. Adequate fibre intake supports bowel regularity, blood glucose control, and gut health, but the type and timing of supplementation matter. This article explores evidence-based guidance on selecting and safely using fibre supplements during GLP-1 therapy, aligned with NHS, NICE, MHRA, and BNF recommendations.
Summary: There is no single best fibre supplement for everyone on GLP-1 therapy, but ispaghula husk (psyllium) is widely recommended by UK healthcare professionals for managing constipation and supporting blood glucose control.
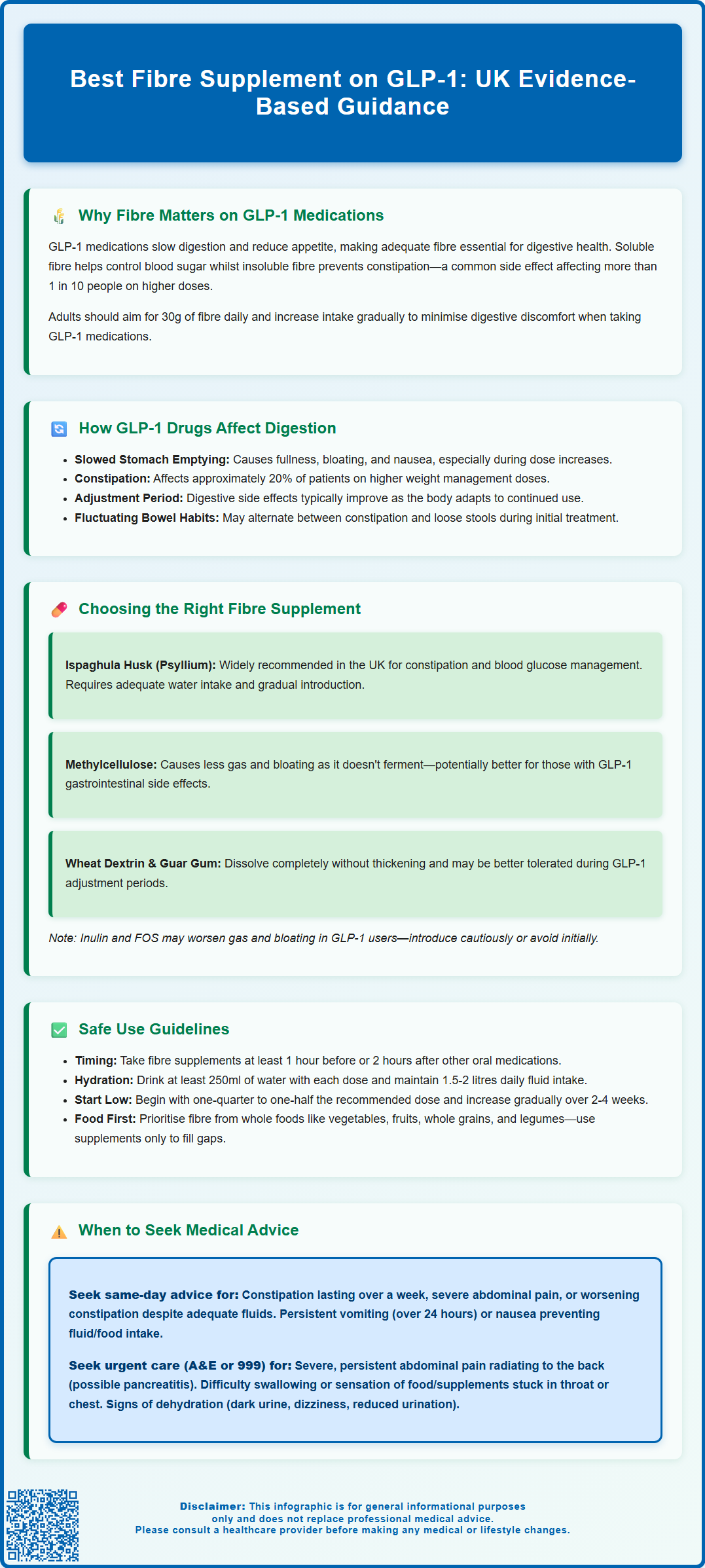
- GLP-1 receptor agonists slow gastric emptying, causing constipation in more than 1 in 10 people on higher doses (Wegovy, Saxenda).
- Ispaghula husk, methylcellulose, wheat dextrin, and partially hydrolysed guar gum are commonly used fibre supplements with varying tolerability profiles.
- Fibre supplements should be taken with at least 250ml of water and introduced gradually to minimise bloating and gas.
- Bulk-forming laxatives should be taken 1 hour before or 2 hours after other oral medications to avoid absorption interference.
- Severe constipation, persistent vomiting, severe abdominal pain, or difficulty swallowing require prompt medical assessment or urgent care.
Table of Contents
Why Fibre Matters When Taking GLP-1 Medications
Glucagon-like peptide-1 (GLP-1) receptor agonists, including semaglutide (Ozempic, Wegovy) and liraglutide (Saxenda, Victoza), are widely used in the management of type 2 diabetes and obesity. These medications work by mimicking a naturally occurring hormone that regulates blood glucose and appetite. However, their mechanism of action—which includes slowing gastric emptying and reducing appetite—can significantly affect digestive function, making adequate fibre intake particularly important.
Fibre plays several crucial roles for individuals on GLP-1 therapy. Soluble fibre helps regulate blood glucose levels by slowing carbohydrate absorption, complementing the glucose-lowering effects of GLP-1 medications. Insoluble fibre adds bulk to stools and promotes regular bowel movements, which becomes especially relevant given that constipation is a common or very common side effect of GLP-1 drugs, depending on the specific product and dose. According to MHRA product information, constipation is very common (affecting more than 1 in 10 people) with higher doses used for weight management (Wegovy, Saxenda), while it is common (affecting up to 1 in 10 people) with doses typically used for diabetes (Ozempic, Victoza).
Beyond addressing constipation, adequate fibre intake supports the gut microbiome, which may influence metabolic health and weight management outcomes, though research in this area is still emerging. Fibre also contributes to satiety—the feeling of fullness—which can help patients adjust to reduced food intake without experiencing excessive hunger. For individuals taking GLP-1 medications, who often experience reduced appetite and smaller meal portions, ensuring sufficient fibre becomes both a therapeutic strategy and a practical necessity for maintaining digestive comfort.
The NHS recommends adults consume 30g of fibre daily, though many people in the UK fall short of this target. Increasing fibre intake gradually helps minimise digestive discomfort, which is particularly important when taking GLP-1 medications.
How GLP-1 Drugs Affect Digestion and Bowel Function
Understanding the pharmacological effects of GLP-1 receptor agonists on the gastrointestinal system helps explain why digestive symptoms occur and why fibre supplementation may be beneficial. GLP-1 medications exert their therapeutic effects through multiple mechanisms that impact both glucose control and digestive function.
Delayed gastric emptying is a well-established effect of GLP-1 drugs that contributes to weight loss and improved glycaemic control. By slowing the rate at which food leaves the stomach and enters the small intestine, these medications prolong satiety and reduce post-prandial glucose spikes. However, this delayed emptying can contribute to feelings of fullness, bloating, and nausea—particularly common when initiating therapy or increasing doses. The European Medicines Agency (EMA) assessment reports note that gastrointestinal adverse effects are typically most pronounced during dose escalation and often improve with continued use.
Effects on intestinal transit may also occur with GLP-1 receptor agonists, though these are more variable and less well characterised than the effects on gastric emptying. The slowing of digestive processes can lead to constipation in some patients, with clinical trials showing varying rates depending on the specific GLP-1 medication and dose. According to MHRA product information, constipation occurs in approximately 20% of patients taking higher doses for weight management, while rates are lower with diabetes doses. Some patients may also experience diarrhoea, and bowel habits can fluctuate during treatment.
Additionally, some patients experience altered bowel habits that may vary between constipation and loose stools, particularly during the adjustment period. NICE guidance on GLP-1 receptor agonists (NG28 for diabetes, TA875 for weight management) acknowledges these gastrointestinal effects and recommends that healthcare professionals counsel patients about expected side effects and management strategies before initiating treatment. The gradual dose escalation recommended in product information is specifically designed to improve gastrointestinal tolerability.
Choosing the Right Fibre Supplement on GLP-1 Therapy
Ispaghula husk (psyllium) is a soluble fibre that forms a gel when mixed with water. It is widely recommended by UK healthcare professionals and is available as a bulk-forming laxative (e.g., Fybogel). Ispaghula is particularly effective for constipation and has evidence supporting its use in blood glucose management. It tends to be well-tolerated when introduced gradually, though adequate fluid intake is essential to prevent it from exacerbating constipation or causing intestinal obstruction. For people with diabetes, sugar-free versions are available and preferable.
Methylcellulose is a semi-synthetic bulk-forming laxative that adds bulk to stools without fermentation, making it may be less likely to cause gas and bloating—a potential advantage for patients already experiencing GLP-1-related gastrointestinal discomfort. It works primarily as a mechanical bulking agent and requires sufficient water intake.
Inulin and fructo-oligosaccharides (FOS) are prebiotic fibres that feed beneficial gut bacteria. Whilst they offer metabolic benefits, they undergo fermentation in the colon, which can produce gas and bloating. For patients on GLP-1 medications who already experience these symptoms, these fibres may need to be introduced very cautiously or avoided initially.
Wheat dextrin and partially hydrolysed guar gum (PHGG) are soluble fibres that dissolve completely in liquids without thickening, making them easy to incorporate into beverages. They may cause less bloating than some other fibres and may be better tolerated during the adjustment period to GLP-1 therapy, though individual responses vary.
When selecting a supplement, consider starting with a lower dose than recommended on the packaging and increasing gradually over several weeks. This approach allows the digestive system to adapt, particularly important given the already altered gut motility from GLP-1 medications. Always check product excipients, including sweeteners and sodium content, particularly if you have diabetes or hypertension.
Safe Use of Fibre Supplements with GLP-1 Medications
Whilst fibre supplements can be beneficial for managing GLP-1-related digestive symptoms, their safe and effective use requires attention to timing, hydration, and potential interactions. The slowed gastric emptying caused by GLP-1 drugs creates specific considerations for supplement administration.
Timing and administration are crucial factors. Bulk-forming laxatives like ispaghula husk should ideally be taken at different times from other oral medications. According to product information and the British National Formulary (BNF), other oral medicines should generally be taken at least 1 hour before or 2 hours after bulk-forming fibre supplements, as fibre can potentially interfere with medication absorption. Always check individual product advice. While GLP-1 drugs are injectable and direct interaction is not a concern, the delayed gastric emptying they cause means that anything consumed may remain in the stomach longer than usual.
Adequate hydration cannot be overemphasised. People taking GLP-1 medications may drink less due to early satiety or nausea, yet fibre supplements require substantial fluid intake to work effectively and safely. Each dose of fibre supplement should be taken with at least 250ml of water, and overall daily fluid intake should be maintained at approximately 1.5 to 2 litres unless medically contraindicated. Insufficient fluid intake with fibre supplements can lead to intestinal obstruction, oesophageal blockage, or worsening constipation—risks that are heightened by the slowed gastric emptying from GLP-1 therapy.
Gradual introduction is essential. Begin with a small amount of fibre supplement (perhaps one-quarter to one-half of the recommended dose) and increase slowly over two to four weeks. This approach minimises gas, bloating, and cramping whilst allowing assessment of tolerance. Patients should monitor their response and adjust accordingly.
Contraindications for bulk-forming laxatives include intestinal obstruction, faecal impaction, colonic atony, and difficulty swallowing. People with severe gastrointestinal disease, including severe gastroparesis, should consult their healthcare provider before using fibre supplements, as GLP-1 medications are generally not recommended in these conditions.
Dietary fibre from whole foods should remain the foundation of fibre intake whenever possible. Supplements are intended to complement, not replace, fibre-rich foods such as vegetables, fruits, whole grains, and legumes. However, given the reduced food intake common with GLP-1 therapy, supplements may help bridge the gap when adequate dietary fibre cannot be achieved through food alone.
When to Seek Medical Advice About Digestive Symptoms
Whilst gastrointestinal symptoms are expected with GLP-1 medications, certain presentations warrant prompt medical evaluation. Patients should be educated about warning signs that distinguish common, manageable side effects from potentially serious complications requiring clinical assessment.
Severe or persistent constipation that does not respond to increased fibre, fluids, and over-the-counter laxatives within a few days requires GP consultation or NHS 111 for same-day advice. Constipation lasting more than a week, or accompanied by severe abdominal pain, may indicate intestinal obstruction—a rare but serious complication. Similarly, if fibre supplements appear to worsen constipation despite adequate fluid intake, medical review is necessary to reassess the management strategy.
Persistent nausea and vomiting that prevents adequate fluid or nutrition intake, or vomiting that lasts more than 24 hours, requires same-day medical assessment via GP or NHS 111. Whilst nausea is common with GLP-1 drugs, severe or prolonged symptoms may indicate gastroparesis (severely delayed gastric emptying) or other complications. The MHRA product information advises that patients experiencing persistent vomiting should contact their healthcare provider promptly.
Abdominal pain that is severe, persistent, or different from previous GLP-1-related discomfort warrants evaluation. Sharp pain, pain that worsens progressively, or pain accompanied by fever could indicate pancreatitis—a known rare adverse effect of GLP-1 medications—or other acute abdominal conditions. If pancreatitis is suspected (persistent severe abdominal pain, sometimes radiating to the back, with or without vomiting), stop taking the GLP-1 medication and seek urgent medical care via A&E or by calling 999.
Right-upper-quadrant pain, especially if accompanied by fever or yellowing of the skin/eyes (jaundice), requires urgent assessment, as GLP-1 medications and weight loss can increase the risk of gallbladder disease.
Signs of dehydration, including dark urine, dizziness, reduced urination, or dry mouth, particularly in the context of reduced fluid intake and fibre supplement use, require medical attention. Dehydration can develop more readily when appetite suppression reduces both food and fluid intake.
Difficulty swallowing or a sensation of food or supplements being stuck in the chest or throat requires immediate medical evaluation, as this may indicate oesophageal obstruction from inadequately hydrated fibre supplements. Stop taking the fibre supplement and seek urgent care.
Patients should maintain regular follow-up with their prescribing clinician as recommended in NICE guidance, typically including monitoring of weight, glycaemic control, and tolerability. Any concerns about digestive symptoms, nutritional adequacy, or the appropriateness of fibre supplementation should be discussed during these appointments or sooner if symptoms are troublesome.
If you experience any suspected side effects from GLP-1 medications or fibre supplements, report them to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Can I take fibre supplements with Ozempic or Wegovy?
Yes, fibre supplements can be taken with GLP-1 medications like Ozempic or Wegovy, but they should be introduced gradually with adequate fluid intake (at least 250ml per dose) to manage constipation safely. Always maintain at least 1 hour before or 2 hours after other oral medications.
Why is constipation so common with GLP-1 medications?
GLP-1 receptor agonists slow gastric emptying and intestinal transit as part of their mechanism of action, which can lead to constipation in more than 1 in 10 people taking higher doses for weight management.
How much fibre should I take daily on GLP-1 therapy?
The NHS recommends 30g of fibre daily for adults. Start fibre supplements at a lower dose than recommended on packaging and increase gradually over 2–4 weeks to minimise digestive discomfort, particularly important given the altered gut motility from GLP-1 medications.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript