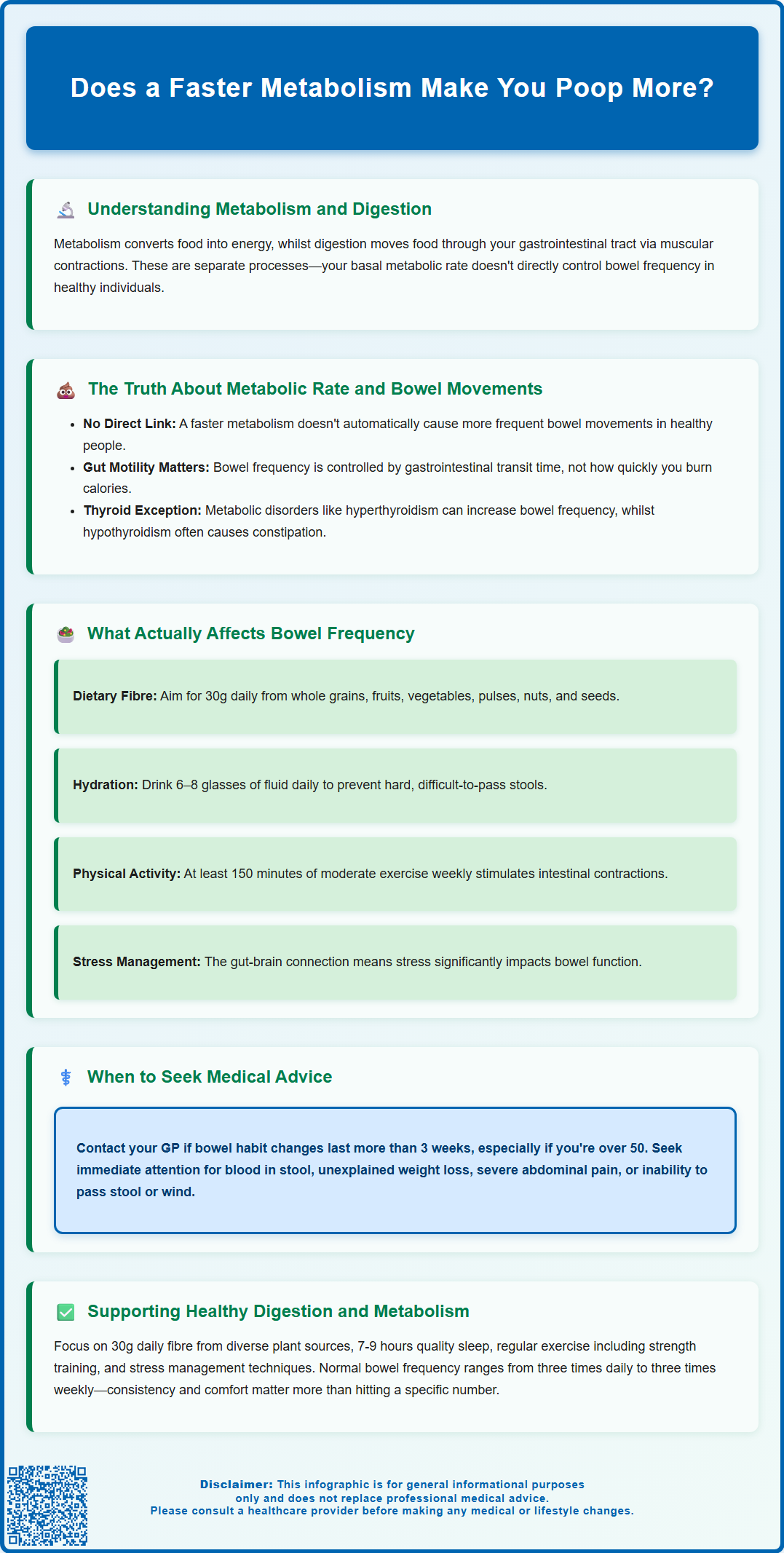
Many people wonder whether having a faster metabolism leads to more frequent bowel movements. Whilst metabolism and digestion are interconnected bodily processes, the relationship between metabolic rate and stool frequency is more complex than commonly assumed. Metabolism refers to how your body converts food into energy, whilst bowel habits are primarily governed by gastrointestinal transit time—the speed at which waste moves through your digestive tract. Understanding this distinction helps clarify misconceptions about metabolic rate and defecation patterns. This article examines the evidence linking metabolism to bowel frequency, explores the factors that genuinely influence how often you poop, and provides guidance on when changes in bowel habits warrant medical attention.
Summary: A faster metabolism does not necessarily make you poop more; bowel frequency is primarily determined by gastrointestinal transit time, diet, and hydration rather than metabolic rate alone.
- Metabolic rate and bowel frequency are indirectly related; gastrointestinal motility is the primary determinant of stool frequency in healthy individuals.
- Thyroid disorders can affect both metabolism and bowel habits—hyperthyroidism may increase stool frequency whilst hypothyroidism often causes constipation.
- Dietary fibre intake, hydration status, physical activity, and gut microbiome composition have greater influence on bowel regularity than basal metabolic rate.
- Normal bowel frequency ranges from three times daily to three times weekly according to NHS guidance; consistency matters more than specific frequency.
- Persistent changes in bowel habit lasting over three weeks, blood in stool, or unexplained weight loss warrant GP evaluation and possible specialist referral.
Table of Contents
Understanding Metabolism and Digestive Function
Metabolism refers to the complex biochemical processes by which your body converts food and drink into energy. This encompasses both catabolism (breaking down molecules to release energy) and anabolism (using energy to build cellular components). Your basal metabolic rate (BMR) represents the energy your body requires at rest to maintain vital functions such as breathing, circulation, and cell production.
The digestive system operates through a separate but interconnected process called gastrointestinal motility—the coordinated muscular contractions that move food through your digestive tract. After you eat, food travels through the oesophagus to the stomach, where it is broken down by gastric acid and enzymes. It then moves into the small intestine for nutrient absorption, and finally into the large intestine (colon), where water is absorbed and waste is formed into stool.
Whilst metabolism and digestion are distinct physiological processes, they do influence one another. Metabolic processes are involved in nutrient utilisation, but in healthy individuals, basal metabolic rate does not directly determine colonic transit time—the key driver of stool frequency. Certain metabolic hormones—particularly thyroid hormones—can influence gut motility. For instance, thyroid hormones regulate the speed of many bodily functions, including digestive transit time.
It is important to recognise that bowel movement frequency varies considerably between individuals. According to NHS guidance, normal bowel habits can range from three times daily to three times weekly. What matters most is consistency and comfort rather than adhering to a specific frequency. Understanding this variability helps contextualise the relationship between metabolism and defecation patterns.
Does a Faster Metabolism Make You Poop More?
The short answer is: not necessarily. Whilst there is a biological connection between metabolic rate and digestive function, the relationship is indirect and influenced by multiple factors. A faster metabolism does not automatically translate to more frequent bowel movements in healthy individuals.
The primary determinant of bowel frequency is gastrointestinal transit time—how long it takes for food to travel from ingestion to excretion—rather than metabolic rate itself. Transit time is influenced by gut motility, which is controlled by the enteric nervous system (the "brain" of the gut), hormones, and the composition of your diet. Someone with a faster metabolism may process nutrients more efficiently, but this does not necessarily accelerate the physical movement of waste through the colon.
However, certain metabolic conditions can affect bowel habits. Hyperthyroidism (overactive thyroid) increases metabolic rate and commonly causes more frequent, looser stools due to accelerated gut motility, as noted by the NHS. Conversely, hypothyroidism (underactive thyroid) slows metabolism and often leads to constipation. These conditions demonstrate that when metabolic changes are significant and pathological, they can indeed influence bowel patterns.
For individuals without thyroid disorders or other metabolic conditions, the correlation between metabolic rate and bowel frequency is weak. Factors such as dietary fibre intake, hydration status, physical activity, gut microbiome composition, and stress levels play far more substantial roles in determining how often you defecate. A person with a naturally faster metabolism who consumes a low-fibre diet may experience less frequent bowel movements than someone with a slower metabolism who eats plenty of fibre-rich foods.
In healthy individuals, evidence of a direct causal link between higher metabolic rate and increased bowel frequency is limited; stool frequency is mainly determined by colonic transit and diet rather than by basal metabolic rate alone.
Factors That Affect Bowel Movement Frequency
Dietary fibre is the most significant dietary factor influencing bowel regularity. Fibre adds bulk to stool and helps it move through the intestines more efficiently. The NHS recommends adults consume approximately 30 grams of fibre daily from sources such as:
-
Whole grains (oats, brown rice, wholemeal bread)
-
Fruits and vegetables
-
Pulses (beans, lentils, chickpeas)
-
Nuts and seeds
Hydration status directly affects stool consistency. The colon absorbs water from digested food; insufficient fluid intake results in harder, more difficult-to-pass stools. Adequate hydration—generally 6–8 glasses of fluid daily as recommended by the NHS—supports normal bowel function.
Physical activity stimulates intestinal contractions and reduces the time it takes for food to move through the large intestine. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity weekly. Regular exercise, even moderate walking, can help maintain regular bowel habits. Conversely, sedentary behaviour is associated with constipation.
Gut microbiome composition plays a crucial role in digestive health. The trillions of bacteria residing in your intestines influence gut motility, immune function, and even mood through the gut-brain axis. Disruptions to the microbiome—from antibiotics, illness, or dietary changes—can temporarily alter bowel patterns.
Stress and psychological factors significantly impact bowel function through the gut-brain connection. Anxiety and stress can either accelerate or slow gut motility, leading to diarrhoea or constipation respectively. Conditions such as irritable bowel syndrome (IBS) exemplify this mind-gut interaction.
Medications can affect bowel habits as a side effect. Opioid analgesics commonly cause constipation, whilst some antibiotics may cause diarrhoea. Iron supplements often cause constipation, and metformin may cause diarrhoea in some people. If bowel changes start after a new medicine, seek advice from a pharmacist or GP; do not stop prescribed medicines without advice.
Age and hormonal changes also influence bowel patterns. Digestive transit naturally slows with ageing, and hormonal fluctuations during menstruation can temporarily affect bowel regularity in people who menstruate.
When to Seek Medical Advice About Bowel Habits
Whilst bowel habit variations are often benign, certain changes warrant medical evaluation. You should contact your GP if you experience:
-
Persistent change in bowel habit lasting more than three weeks, particularly if you are over 50 years old
-
Blood in your stool (red blood or black, tarry stools)
-
Unexplained weight loss accompanying bowel changes
-
Severe or persistent abdominal pain
-
Persistent diarrhoea lasting more than 7 days, or sooner if accompanied by dehydration, severe pain, or fever
-
Severe constipation unresponsive to lifestyle modifications and over-the-counter remedies
These symptoms may indicate conditions requiring investigation, such as inflammatory bowel disease (Crohn's disease or ulcerative colitis), coeliac disease, or colorectal cancer. Your GP may use faecal immunochemical testing (FIT) to help assess your risk and determine if you need referral to a specialist, in line with NICE guidance.
The NHS Bowel Cancer Screening Programme varies across UK nations: in England, adults aged 60–74 are invited (with phased expansion to ages 50–59); Scotland screens from 50–74; Wales from 55–74; and Northern Ireland from 60–74. Early detection significantly improves outcomes.
Signs of thyroid dysfunction should also prompt medical review. Hyperthyroidism symptoms include frequent loose stools, unintentional weight loss despite increased appetite, rapid heartbeat, tremor, and heat intolerance. Hypothyroidism may present with constipation, unexplained weight gain, fatigue, and cold sensitivity. Your GP can arrange thyroid function tests (typically TSH with reflex free T4; T3 is only measured if hyperthyroidism is suspected) if indicated.
Sudden onset of severe symptoms—such as inability to pass stool or wind, severe abdominal distension, or vomiting—may indicate bowel obstruction requiring urgent assessment. Similarly, profuse diarrhoea with signs of dehydration (dizziness, reduced urination, confusion) necessitates prompt medical attention.
NICE guidance emphasises safety-netting advice: if you have concerns about persistent or worsening bowel symptoms, it is always appropriate to seek medical evaluation rather than attributing changes solely to diet or metabolism.
Supporting Healthy Metabolism and Digestion
Optimising both metabolic and digestive health involves evidence-based lifestyle strategies rather than quick fixes or unproven supplements.
Dietary approaches should prioritise:
-
Adequate fibre intake from diverse plant sources to support regular bowel movements (NHS recommends 30g daily)
-
Balanced macronutrients including sufficient protein to support metabolic function
-
Probiotic and prebiotic foods such as yoghurt, kefir, sauerkraut, and foods rich in inulin (onions, garlic, bananas) to support gut microbiome health. Evidence for probiotics is mixed and benefits are often strain-specific; for conditions like IBS, NICE suggests trying a single product for up to 4 weeks and stopping if there's no benefit
-
Regular meal patterns rather than erratic eating, which helps regulate digestive processes
-
Mindful eating and thorough chewing to aid digestion
Physical activity benefits both metabolism and gut motility. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity weekly, plus strength activities on at least 2 days per week. Resistance training helps maintain muscle mass, which supports metabolic rate, whilst aerobic exercise promotes healthy gut transit.
Adequate sleep is essential for metabolic regulation. Sleep deprivation disrupts hormones that control appetite and metabolism (leptin and ghrelin) and may indirectly affect digestive function through stress pathways. The NHS advises adults should aim for 7–9 hours of quality sleep nightly.
Stress management techniques—including mindfulness, cognitive behavioural approaches, or relaxation exercises—can benefit both metabolic health and gut function, particularly for individuals with stress-sensitive digestive symptoms.
Hydration remains fundamental. Water supports metabolic processes and maintains healthy stool consistency. The NHS recommends 6-8 cups/glasses of fluid daily, though individual needs vary based on activity level, climate, and overall health.
Avoiding unnecessary restrictions is important. Unless you have diagnosed food intolerances or allergies, overly restrictive diets may compromise nutritional adequacy and gut microbiome diversity. If you suspect food intolerances, seek proper investigation rather than self-diagnosing.
For persistent concerns about metabolism or digestion, consult healthcare professionals who can provide personalised assessment and evidence-based recommendations tailored to your individual circumstances. If you experience side effects that you suspect may be related to a medicine, report them to the MHRA Yellow Card scheme.
Frequently Asked Questions
Can thyroid problems affect how often you poop?
Yes, thyroid disorders significantly affect bowel habits. Hyperthyroidism (overactive thyroid) increases metabolic rate and commonly causes more frequent, looser stools due to accelerated gut motility, whilst hypothyroidism (underactive thyroid) slows metabolism and often leads to constipation.
What is the most important factor affecting bowel movement frequency?
Dietary fibre intake is the most significant factor influencing bowel regularity. The NHS recommends approximately 30 grams of fibre daily from whole grains, fruits, vegetables, pulses, nuts, and seeds to support healthy bowel function and regular stool frequency.
When should I see a GP about changes in my bowel habits?
You should contact your GP if you experience persistent changes in bowel habit lasting more than three weeks (particularly if over 50), blood in your stool, unexplained weight loss, severe abdominal pain, persistent diarrhoea lasting over 7 days, or severe constipation unresponsive to lifestyle changes.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












