Glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide and liraglutide are transforming appetite regulation and food choices for many patients managing type 2 diabetes or obesity. These medications work by mimicking natural hormones that control hunger and satiety, often leading to significant changes in eating patterns and food preferences. Whilst home-prepared meals offer optimal nutritional control, practical circumstances sometimes necessitate fast food choices. Understanding how to navigate these options whilst on GLP-1 therapy helps maintain treatment effectiveness and nutritional adequacy. This guide explores evidence-based strategies for selecting appropriate fast food when taking GLP-1 medications, alongside essential nutritional considerations and side effect management.
Summary: The best fast food options on GLP-1 medications prioritise grilled protein sources, smaller portions, and customisation to reduce fat content whilst maintaining adequate nutrition.
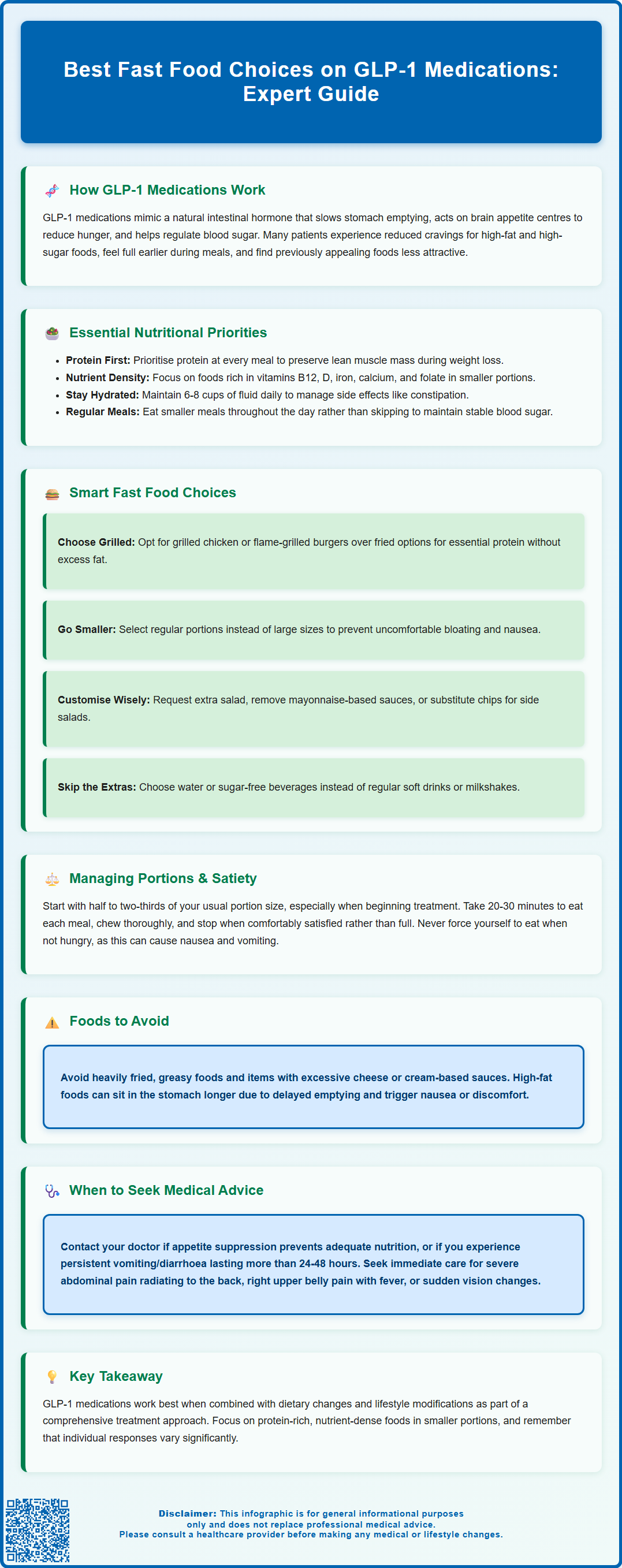
- GLP-1 receptor agonists slow gastric emptying and reduce appetite by acting on brain receptors, requiring smaller meal portions and slower eating pace.
- Grilled chicken, flame-grilled burgers without excessive sauces, and fish options provide essential protein with lower fat content than fried alternatives.
- High-fat and heavily fried foods may trigger nausea and discomfort due to delayed gastric emptying caused by GLP-1 medications.
- Adequate protein intake, micronutrient attention, and hydration (6–8 cups daily) are crucial when appetite is suppressed to prevent nutritional deficiencies.
- Common gastrointestinal side effects include nausea and constipation, particularly during treatment initiation; severe abdominal pain requires urgent medical review for possible pancreatitis.
- Patients should inform healthcare professionals about GLP-1 use before procedures involving sedation due to aspiration risk from delayed gastric emptying.
Table of Contents
How GLP-1 Medications Affect Appetite and Food Choices
Glucagon-like peptide-1 (GLP-1) receptor agonists have specific licensed indications in the UK. Semaglutide (Ozempic) and liraglutide (Victoza) are approved for type 2 diabetes management, while semaglutide (Wegovy) and liraglutide (Saxenda) are licensed for weight management in adults with obesity or overweight with weight-related conditions.
The mechanism of action involves several pathways that influence eating behaviour. GLP-1 receptor agonists slow gastric emptying (an effect that may diminish over time with continued treatment), meaning food remains in the stomach for longer periods, promoting a feeling of fullness. They also act on receptors in the brain's appetite centres, particularly the hypothalamus, reducing hunger signals and increasing satiety. Additionally, these medications enhance insulin secretion and suppress glucagon release in a glucose-dependent manner when blood glucose levels are elevated, helping to stabilise blood glucose levels while reducing the risk of hypoglycaemia when used alone.
Many patients taking GLP-1 medications report changes in their food preferences and eating patterns. Some experience reduced cravings for high-fat and high-sugar foods, alongside an earlier sense of fullness during meals. Some individuals find that previously appealing foods no longer hold the same attraction, though responses vary considerably between patients.
It is important to recognise that whilst GLP-1 medications can facilitate healthier food choices, they work most effectively when combined with appropriate dietary modifications and lifestyle changes. The NICE guidelines for obesity management emphasise that pharmacological interventions should be part of a comprehensive approach including nutritional education and behavioural support.
Nutritional Considerations When Taking GLP-1 Treatments
When taking GLP-1 receptor agonists, maintaining adequate nutrition becomes particularly important due to the medications' effects on appetite and food intake. The reduced appetite and early satiety can lead to significantly decreased caloric consumption, which, whilst beneficial for weight management, may inadvertently result in nutritional deficiencies if dietary choices are not carefully considered.
Protein intake should be prioritised to preserve lean muscle mass during weight loss. Including a good source of protein at each meal and snack is advisable. While specific requirements vary by individual, many dietitians suggest aiming for adequate protein distribution throughout the day. Those with specific nutritional needs should discuss personalised protein targets with a registered dietitian or healthcare professional.
Micronutrient adequacy requires attention, particularly for vitamins B12, D, iron, calcium, and folate. When consuming smaller portions, it becomes more challenging to meet daily requirements through diet alone. Patients should focus on nutrient-dense foods that provide maximum nutritional value in smaller volumes. A daily multivitamin supplement may be considered for some individuals, though this should be discussed with a healthcare professional.
Hydration is another critical consideration. The NHS recommends 6-8 cups of fluid daily for most adults, though requirements may differ for those with certain medical conditions such as heart or kidney disease. Some patients experience nausea or reduced thirst alongside decreased appetite. Maintaining adequate fluid intake helps manage potential side effects such as constipation, which is common with GLP-1 medications, and supports overall physiological function.
Patients should be encouraged to eat regular, smaller meals rather than skipping meals entirely, even when appetite is suppressed. This approach helps maintain stable blood glucose levels and ensures consistent nutrient intake throughout the day. For those taking GLP-1 medications alongside insulin or sulfonylureas, it's particularly important not to skip meals or drastically reduce carbohydrate intake without medical advice, as this could increase hypoglycaemia risk.
Choosing Fast Food Options While on GLP-1 Therapy
Whilst home-prepared meals offer greater control over ingredients and nutritional content, there are occasions when fast food may be the practical option. For individuals taking GLP-1 medications, making informed choices at fast food establishments can help maintain nutritional goals whilst managing the medication's effects on appetite and digestion.
Grilled protein options generally represent better choices than fried alternatives. Grilled chicken sandwiches, flame-grilled burgers (without excessive sauces), or fish options provide essential protein without the added fat from deep frying, which may be poorly tolerated due to delayed gastric emptying. Many UK fast food chains now provide detailed nutritional information and calorie labelling (mandatory for larger businesses), allowing patients to compare options and select items with appropriate protein content and moderate fat levels.
Portion size awareness is crucial. Many fast food establishments offer smaller portion sizes that may be more appropriate for individuals on GLP-1 therapy. A regular-sized fast food meal may be excessive given the reduced appetite and early satiety these medications produce. Choosing smaller burgers, regular rather than large portions of chips, and avoiding meal deals that encourage overconsumption can help prevent uncomfortable fullness and potential nausea. If considering children's meals, check nutrition information to ensure they provide adequate protein and aren't excessively high in salt or sugar.
Customisation options should be utilised. Most chains allow modifications such as requesting extra salad, removing mayonnaise-based sauces, or substituting chips for side salads. These adjustments can significantly improve the nutritional profile of a meal. Opting for water or sugar-free beverages rather than regular soft drinks, milkshakes or other high-sugar options eliminates unnecessary calories and sugar that may worsen gastrointestinal symptoms.
Foods to approach cautiously include heavily fried items, very greasy foods, and those with excessive cheese or cream-based sauces. The delayed gastric emptying caused by GLP-1 medications means high-fat foods may sit uncomfortably in the stomach for extended periods, potentially triggering nausea or discomfort. If side effects such as persistent nausea, vomiting, or abdominal pain occur after eating, patients should contact their GP or diabetes specialist nurse for advice.
Managing Portion Sizes and Satiety on GLP-1 Medications
The enhanced satiety produced by GLP-1 receptor agonists requires a fundamental adjustment in approach to portion sizes. Many patients find that their previous meal portions are no longer appropriate, and attempting to consume usual amounts can lead to uncomfortable fullness, nausea, or even vomiting.
Starting with smaller portions is advisable, particularly when beginning GLP-1 therapy or after dose increases. A practical approach is to serve approximately half to two-thirds of a previous typical portion, eating slowly and mindfully. Patients should be encouraged to stop eating when they feel comfortably satisfied rather than continuing to a feeling of fullness. The medication's effect on satiety signals means that the sensation of fullness may arrive quite suddenly, and eating beyond this point can cause significant discomfort.
Eating pace matters considerably. The delayed gastric emptying means that the stomach fills more quickly and empties more slowly than before starting medication. Eating too rapidly may result in consuming more food than can be comfortably accommodated before satiety signals register. Taking at least 20–30 minutes to complete a meal, putting utensils down between bites, and chewing thoroughly can help prevent overeating and associated discomfort. Remaining upright for 30-60 minutes after eating and sipping fluids slowly between (rather than during) meals may also help reduce reflux and nausea.
Recognising individual tolerance is important, as responses to GLP-1 medications vary between individuals. Some patients experience profound appetite suppression, whilst others notice more modest effects. Additionally, tolerance to different food types may vary; some individuals find that certain textures or food groups are better tolerated than others. Keeping a brief food diary during the initial weeks of treatment can help identify personal patterns and preferences.
Avoiding the temptation to 'push through' feelings of fullness is crucial. Unlike typical dieting, where some hunger is expected, GLP-1 medications are designed to reduce appetite physiologically. Forcing oneself to eat when not hungry or continuing to eat when satisfied can trigger adverse effects and is counterproductive to the medication's intended mechanism. If appetite becomes so suppressed that maintaining adequate nutrition or hydration is difficult, this should be discussed with the prescribing clinician, as dose adjustment may be necessary.
Patients should inform healthcare professionals, including surgical teams, endoscopists and dentists, about their GLP-1 medication use before procedures involving sedation or anaesthesia, due to the delayed gastric emptying effect and potential aspiration risk.
Common Side Effects and Food Tolerance on GLP-1 Drugs
GLP-1 receptor agonists are generally well-tolerated, but gastrointestinal side effects are common, particularly during treatment initiation and dose escalation. Understanding these effects and their relationship to food intake helps patients manage symptoms and maintain treatment adherence.
Nausea is the most frequently reported side effect, affecting many patients to varying degrees depending on the specific medication and dose. This typically occurs during the first few weeks of treatment or following dose increases and often improves with time as the body adjusts. Nausea may be exacerbated by consuming large portions, eating too quickly, or consuming high-fat foods. Management strategies include eating smaller, more frequent meals, avoiding lying down immediately after eating, and choosing bland, easily digestible foods when symptoms are present. If nausea is severe, persistent, or accompanied by inability to keep down fluids, patients should contact their healthcare provider promptly.
Constipation affects many patients due to the medication's effect on gastrointestinal motility. Adequate fibre intake (approximately 30 grams daily as recommended by the Scientific Advisory Committee on Nutrition), sufficient hydration, and regular physical activity can help manage this. However, introducing high-fibre foods should be done gradually to avoid bloating and discomfort. If constipation persists despite lifestyle measures, discussing appropriate laxative options with a pharmacist or GP is advisable.
Vomiting, diarrhoea, and abdominal discomfort occur less frequently but require attention. Persistent vomiting or diarrhoea can lead to dehydration and electrolyte imbalances, which may increase the risk of acute kidney injury. Patients experiencing these symptoms should ensure adequate fluid intake and seek medical advice if symptoms continue for more than 24–48 hours, or if they notice reduced urine output or dark-coloured urine.
Food aversions and taste changes are reported by some patients. Changes in taste (dysgeusia) are listed as possible side effects for some GLP-1 medications. Some individuals develop aversions to previously enjoyed foods, particularly those high in fat or sugar. Whilst this may support weight management goals, it is important to ensure that aversions do not lead to an overly restricted diet lacking nutritional variety.
Serious adverse effects, whilst rare, include pancreatitis and gallbladder problems. Patients should seek immediate medical attention if they experience severe, persistent abdominal pain, particularly if radiating to the back, as this may indicate pancreatitis. Similarly, right upper quadrant pain, fever, or yellowing of the skin/eyes should prompt urgent medical review for possible gallbladder disease. People with diabetes, especially those with pre-existing diabetic retinopathy, should report any visual changes promptly, as rapid improvement in blood glucose control with semaglutide may temporarily worsen retinopathy.
Patients taking GLP-1 medications alongside insulin or sulfonylureas may have an increased risk of hypoglycaemia and should discuss potential dose adjustments of these medications with their healthcare team.
Report suspected side effects to medicines via the Yellow Card Scheme at yellowcard.mhra.gov.uk or search for MHRA Yellow Card in the Google Play or Apple App Store.
Frequently Asked Questions
Can I eat fast food whilst taking GLP-1 medications like semaglutide or liraglutide?
Yes, occasional fast food consumption is possible on GLP-1 therapy, though home-prepared meals are preferable. Choose grilled protein options, smaller portions, and customise orders to reduce fat content whilst ensuring adequate protein intake to support nutritional goals.
Why do high-fat fast foods cause discomfort on GLP-1 medications?
GLP-1 receptor agonists slow gastric emptying, meaning food remains in the stomach longer. High-fat foods may sit uncomfortably for extended periods, potentially triggering nausea, discomfort, or vomiting due to this delayed emptying effect.
How should I adjust portion sizes when eating fast food on GLP-1 treatment?
Start with approximately half to two-thirds of your previous typical portion, eating slowly over 20–30 minutes. Stop when comfortably satisfied rather than full, as satiety signals arrive suddenly with GLP-1 medications, and overeating can cause significant discomfort.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












