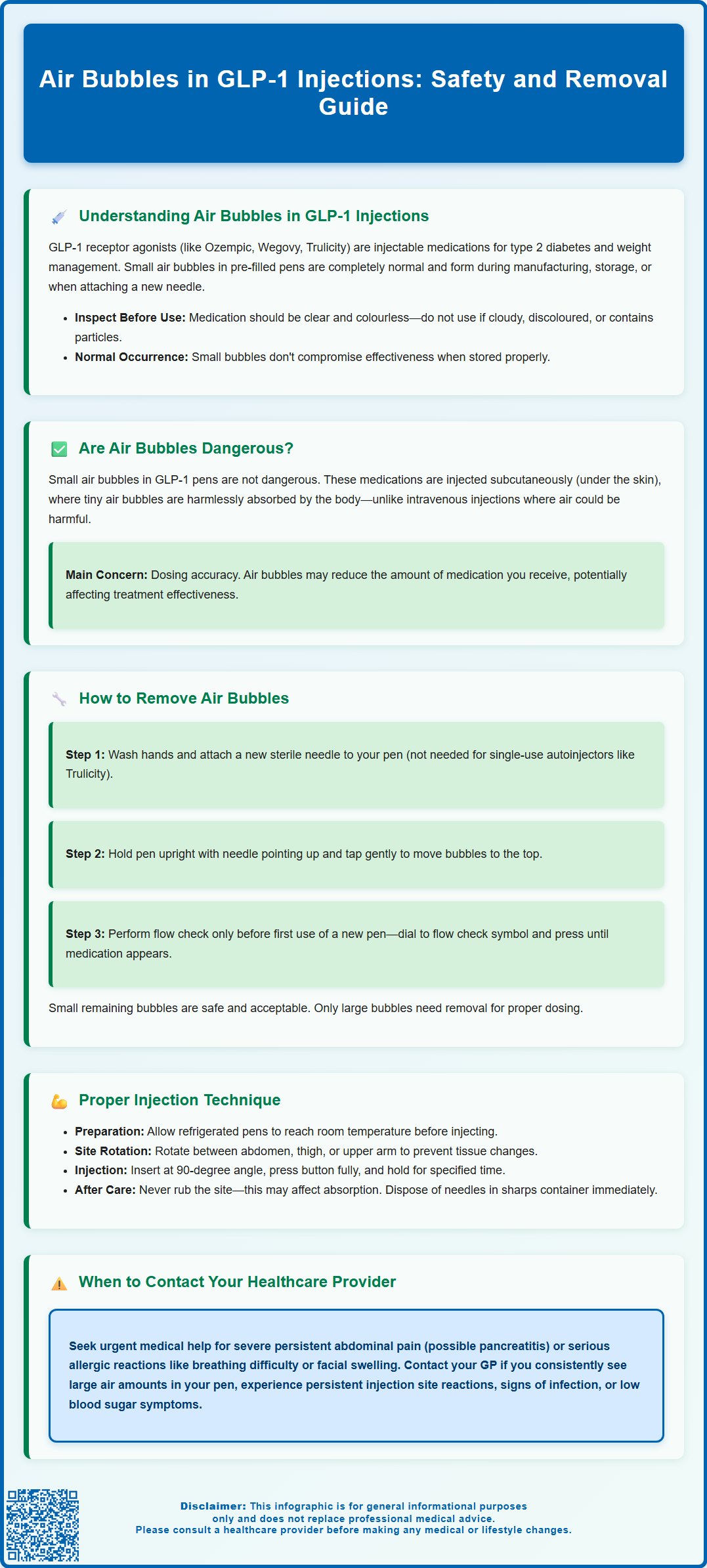
Small air bubbles in GLP-1 injection pens are a common observation that understandably concerns many patients using medications such as semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), or liraglutide (Victoza, Saxenda). These bubbles typically appear during manufacturing, storage, or pen preparation and do not indicate that your medication is compromised. Whilst air bubbles in subcutaneous injections pose no safety risk, removing larger bubbles before injection helps ensure accurate dosing. Understanding when air bubbles matter—and when they don't—empowers patients to use their GLP-1 medications confidently and safely. This guide explains the significance of air bubbles, proper removal techniques, and correct injection practices aligned with UK clinical guidance.
Summary: Small air bubbles in GLP-1 injection pens are not dangerous when administered subcutaneously and are commonly present due to manufacturing or storage, though removing larger bubbles ensures accurate dosing.
- GLP-1 receptor agonists (semaglutide, dulaglutide, liraglutide) are subcutaneous injections for type 2 diabetes and weight management.
- Air bubbles in subcutaneous injections cannot cause air embolism as they are absorbed harmlessly by fatty tissue beneath the skin.
- Large air bubbles may reduce dose accuracy, so removal via tapping and flow checks is recommended for multi-dose pens before injection.
- Proper injection technique includes rotating sites, inserting at 90 degrees, and holding the button for the specified duration to ensure complete delivery.
- Contact your GP for persistent large bubbles or cloudy medication; seek urgent help for severe abdominal pain or allergic reactions.
- Report suspected side effects to the MHRA Yellow Card Scheme and dispose of needles in sharps bins obtained from your GP or pharmacy.
Table of Contents
Understanding Air Bubbles in GLP-1 Injections
Glucagon-like peptide-1 (GLP-1) receptor agonists are injectable medications increasingly prescribed for type 2 diabetes management and, in some formulations, weight management. These medications—including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and others—are typically administered via pre-filled injection pens designed for subcutaneous delivery (under the skin only). Many patients using these medications notice small air bubbles within the pen cartridge and understandably worry about their significance.
Air bubbles can appear in GLP-1 injection pens for several reasons. During manufacturing and filling processes, small amounts of air may become trapped within the medication cartridge. Temperature changes during storage or transport can also cause air to separate from the solution. Additionally, the mechanical action of preparing the pen—attaching a new needle or preparing the device—may introduce or reveal air pockets that were previously unnoticed. Small air bubbles are commonly observed in multi-dose injection pens and their presence does not typically indicate that the medication has been compromised.
Before using any GLP-1 medication, always check that the solution is clear and colourless (or nearly colourless). Do not use the pen if the solution appears cloudy, discoloured, or contains visible particles. The liquid formulation is carefully manufactured to remain stable and effective throughout its shelf life when stored correctly. Understanding that small air bubbles can be normal helps reduce unnecessary anxiety, but it's important to follow the specific Instructions for Use (IFU) provided with your particular GLP-1 device, as handling procedures vary between different products.
Are Air Bubbles in GLP-1 Pens Dangerous?
The presence of small air bubbles in GLP-1 injection pens is not dangerous and poses minimal risk to patients when the medication is administered subcutaneously (under the skin) as intended. This reassurance is supported by manufacturer guidance in Patient Information Leaflets (PILs). GLP-1 medications must only be injected subcutaneously and never into a vein. Unlike intravenous administration—where air bubbles could theoretically enter the bloodstream and cause complications—subcutaneous injections deliver medication into the fatty tissue layer beneath the skin, where small air bubbles are harmlessly absorbed by the body.
Manufacturer instructions and UK injection technique guidance (FIT UK) consistently indicate that small air bubbles in subcutaneous GLP-1 injections are not associated with serious adverse events such as air embolism. The volumes of air typically present in injection pens (often just a few small bubbles) are far below any threshold that could cause harm via the subcutaneous route.
However, air bubbles can affect dosing accuracy. If a significant amount of air is injected instead of medication, you may receive less than your prescribed dose, potentially affecting glycaemic control or treatment outcomes. This is the primary reason why removing visible air bubbles before injection is recommended for multi-dose pens—not because they are dangerous, but to ensure you receive the full therapeutic dose. If you suspect you have not received your full dose, do not administer an extra dose to compensate. Instead, follow the 'missed dose' guidance in your medication's PIL or contact your healthcare professional.
When to seek advice: Contact your GP or diabetes specialist nurse if you consistently notice large amounts of air in your pen, if the medication appears cloudy or discoloured, or if you experience unexpected symptoms after injection. Seek urgent medical help (call NHS 111 or 999) if you develop severe persistent abdominal pain (which may indicate pancreatitis) or signs of a serious allergic reaction such as difficulty breathing, severe rash, or swelling of the face, lips or throat.
How to Remove Air Bubbles from Your GLP-1 Injection Pen
Removing air bubbles from your GLP-1 injection pen is a straightforward process, but the exact procedure varies by device type. Always begin by washing your hands thoroughly and gathering your supplies: the injection pen, a new pen needle, and alcohol wipes. The following guidance applies primarily to multi-dose pens (like Ozempic and Victoza); single-use autoinjectors (like Trulicity and Wegovy) typically do not require bubble removal or priming.
Step-by-step bubble removal process for multi-dose pens:
-
Attach a new needle: Screw or click a new, sterile needle onto your pen according to the device instructions. Remove both the outer and inner needle caps.
-
Hold the pen upright: Position the pen vertically with the needle pointing upward toward the ceiling. This allows air bubbles to rise naturally to the top of the cartridge due to their lower density compared to the liquid medication.
-
Tap the cartridge gently: Using your finger, tap the side of the cartridge several times. This helps dislodge smaller bubbles and encourages them to merge and rise to the top where the needle is attached.
-
Perform a flow check (if required): Following your specific pen's Instructions for Use, perform a flow check by dialling to the flow check symbol (not a specific mg dose) and pressing the injection button whilst holding the pen upright. You should see a drop of medication appear at the needle tip, confirming that air has been expelled. Note that flow checks are typically only required before the first use of a new pen, not before every dose, and some devices do not require flow checks at all.
-
Check the cartridge: Look through the viewing window to confirm that large air bubbles have been removed. Small bubbles may remain—this is acceptable and will not affect your dose or safety.
Important considerations: Always use a new needle for each injection, as reusing needles can introduce air and increase infection risk. Never share your pen or needles with anyone else, even if the needle has been changed. If you cannot remove a large air bubble after following the troubleshooting steps in your device's Instructions for Use, contact your pharmacy or the manufacturer's helpline for advice. Never attempt to remove the cartridge or disassemble the pen yourself, as this compromises sterility and device function. Dispose of used needles in a sharps bin obtained from your GP surgery or pharmacy.
Proper Injection Technique for GLP-1 Medications
Correct injection technique is essential for ensuring optimal medication delivery, minimising discomfort, and reducing the risk of injection site reactions. GLP-1 receptor agonists are designed for subcutaneous administration only, typically into the abdomen, thigh, or upper arm. Manufacturer guidance and FIT UK injection technique recommendations emphasise the importance of proper technique for both efficacy and patient safety.
Preparing for injection:
Before administering your GLP-1 medication, allow the pen to reach room temperature if it has been refrigerated—this reduces injection discomfort. Wash your hands thoroughly and select an injection site, rotating sites with each dose to prevent lipohypertrophy (fatty lumps under the skin) or lipoatrophy (loss of fatty tissue). Avoid areas that are bruised, tender, red, or scarred. Clean the chosen site with an alcohol wipe and allow it to dry completely.
Injection procedure:
-
After preparing your pen according to the specific Instructions for Use, dial your prescribed dose following the pen's instructions.
-
Pinch the skin gently to create a fold of subcutaneous tissue (this may not be necessary for all body types—follow your healthcare professional's advice).
-
Insert the needle at a 90-degree angle (or 45 degrees if you have less subcutaneous fat) using a quick, dart-like motion.
-
Press the injection button fully and hold for the time specified in your device's Instructions for Use to ensure complete dose delivery.
-
Release the skin fold (if used), then withdraw the needle straight out at the same angle it was inserted.
Post-injection care:
Do not rub the injection site, as this may affect medication absorption. Dispose of the used needle immediately in a sharps container—never recap needles, as this increases needlestick injury risk. Return full sharps bins to your GP surgery, pharmacy, or local council waste facility (arrangements vary by area). If a small amount of medication leaks from the injection site or you notice bleeding, apply gentle pressure with a clean tissue; this occasionally occurs and does not necessarily mean you have lost a significant portion of your dose.
Common adverse effects of GLP-1 medications include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, particularly when initiating treatment or increasing doses. These typically improve over time. Injection site reactions—including redness, itching, or mild swelling—are usually minor and self-limiting.
Contact your GP or diabetes team if you experience: persistent injection site reactions, signs of infection (increasing pain, warmth, swelling, or discharge), or symptoms of hypoglycaemia if you are taking GLP-1 medications alongside insulin or sulphonylureas. Seek urgent medical help (NHS 111 or 999) for severe persistent abdominal pain (which may indicate pancreatitis) or signs of a serious allergic reaction. You can report any suspected side effects to the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk.
Regular follow-up with your healthcare team ensures your injection technique remains optimal and allows for monitoring of treatment response and any adverse effects. Many GP surgeries and diabetes centres offer injection technique reviews—do not hesitate to request this support if you feel uncertain about any aspect of your medication administration.
Frequently Asked Questions
Can air bubbles in my GLP-1 pen cause an air embolism?
No, small air bubbles in GLP-1 injections administered subcutaneously (under the skin) cannot cause air embolism, as they are absorbed harmlessly by the fatty tissue and do not enter the bloodstream.
Do I need to remove air bubbles before every GLP-1 injection?
For multi-dose pens, removing visible larger air bubbles helps ensure accurate dosing, though small bubbles are harmless. Single-use autoinjectors like Trulicity and Wegovy typically do not require bubble removal or priming.
What should I do if I cannot remove a large air bubble from my GLP-1 pen?
If you cannot remove a large air bubble after following your device's Instructions for Use, contact your pharmacy or the manufacturer's helpline for advice rather than attempting to disassemble the pen yourself.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript