GLP-1 receptor agonist pens are pre-filled injection devices used to deliver medications for type 2 diabetes and weight management. Learning how to use the pen correctly ensures safe, effective treatment and optimal blood glucose control. This guide explains step-by-step how to prepare, inject, store, and dispose of your GLP-1 agonist device, including products such as Ozempic, Trulicity, Victoza, Saxenda, and Wegovy. Whether you're using a multi-dose dial pen or a single-use autoinjector, proper technique prevents complications and maximises therapeutic benefit. Understanding injection site rotation, troubleshooting common problems, and recognising when to seek medical advice are essential skills for confident self-management.
Summary: GLP-1 agonist pens are subcutaneous injection devices that deliver diabetes and weight management medications through either multi-dose dial pens or single-use autoinjectors, requiring proper preparation, injection technique, site rotation, and storage to ensure safe and effective treatment.
- GLP-1 receptor agonists mimic a natural gut hormone that stimulates insulin secretion, suppresses glucagon, slows gastric emptying, and promotes satiety.
- Devices are administered subcutaneously into the abdomen, thigh, or upper arm, typically once weekly or once daily depending on the formulation.
- Proper injection technique includes allowing the device to reach room temperature, performing flow checks for multi-dose pens, and holding the injection button for the specified duration.
- Systematic site rotation prevents lipohypertrophy and tissue damage that could affect medication absorption and glycaemic control.
- Unopened devices must be refrigerated at 2°C to 8°C; in-use storage duration varies by product from 14 days to 6 weeks.
- Contact your healthcare team urgently for severe abdominal pain, signs of pancreatitis, hypoglycaemia symptoms, or allergic reactions.
Table of Contents
- What Are GLP-1 Agonist Pens and How Do They Work?
- Preparing Your GLP-1 Pen for First Use
- Step-by-Step Guide to Injecting Your GLP-1 Agonist
- Choosing and Rotating Injection Sites Safely
- Storing Your GLP-1 Pen and Disposing of Needles
- Common Problems and When to Contact Your Healthcare Team
- Frequently Asked Questions
What Are GLP-1 Agonist Pens and How Do They Work?
GLP-1 (glucagon-like peptide-1) receptor agonist devices are pre-filled injection systems used to deliver medications that help manage type 2 diabetes and, in some cases, support weight management. These include multi-dose pens with adjustable doses (such as Ozempic, Victoza) and single-dose autoinjectors with fixed doses (such as Trulicity). They contain medicines such as semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), lixisenatide (Lyxumia), or exenatide (Byetta, Bydureon). The device design makes self-injection straightforward.
GLP-1 receptor agonists work by mimicking a natural hormone produced in the gut. When you eat, GLP-1 is released and performs several important functions: it stimulates insulin secretion from the pancreas when blood glucose levels are elevated, suppresses glucagon (a hormone that raises blood sugar), slows gastric emptying to reduce post-meal glucose spikes, and promotes satiety in the brain. This multi-faceted mechanism helps improve glycaemic control whilst often leading to weight loss as a beneficial side effect.
These medications are administered subcutaneously (under the skin) rather than into muscle or veins. Most GLP-1 receptor agonist devices are designed for once-weekly or once-daily injections , depending on the specific formulation. The MHRA has approved various GLP-1 receptor agonists, and NICE guidelines (NG28) recommend them as treatment options for type 2 diabetes when initial therapies are insufficient. Specific products (Wegovy, Saxenda) are indicated for weight management under specialist guidance according to NICE criteria.
Understanding how your specific device works is essential for achieving optimal therapeutic outcomes. Your healthcare team will prescribe the appropriate medication and dose based on your individual needs, kidney function, and treatment goals. Note that these medications are not insulin and are not suitable for type 1 diabetes.
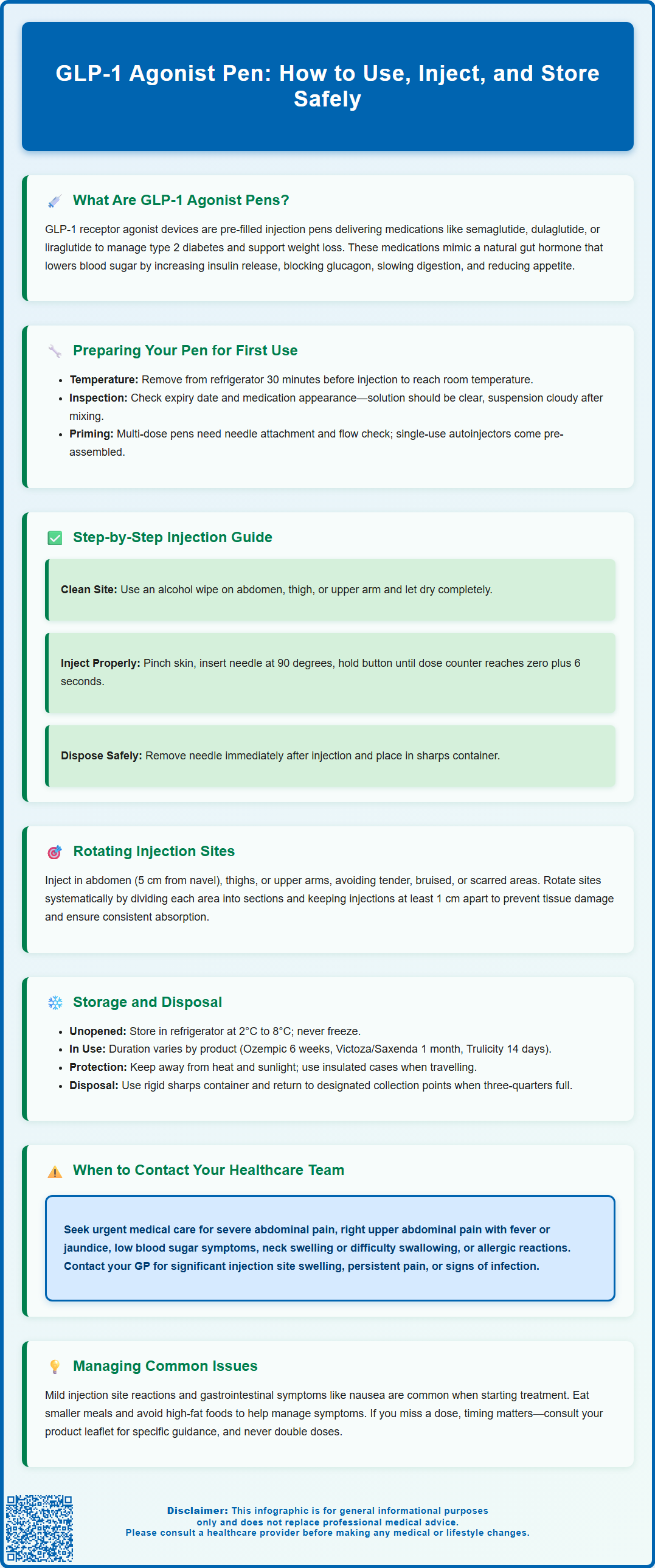
Preparing Your GLP-1 Pen for First Use
Before using your GLP-1 device for the first time, careful preparation ensures safe and effective administration. Start by reading the patient information leaflet supplied with your medication, as different brands have specific instructions. Check the expiry date printed on the label—never use an expired product. Examine the medication through the viewing window; for solution products (like Ozempic, Victoza, Trulicity), it should be clear and colourless or slightly yellow. For suspension products (like some exenatide ER formulations), the medication will appear cloudy after proper mixing. Do not use if the appearance doesn't match your product's description in the leaflet.
Remove the device from the refrigerator approximately 30 minutes before injection to allow it to reach room temperature. Injecting cold medication can cause discomfort at the injection site. Wash your hands thoroughly with soap and water and dry them completely.
Device preparation varies by product type:
For multi-dose pens (e.g., Ozempic, Victoza, Saxenda):
-
Gather your pen, a new pen needle, an alcohol wipe, and a sharps container
-
Remove the pen cap and check that the rubber seal is intact
-
Take a new needle, remove the paper tab, and attach it securely to the pen
-
Remove the outer needle cap (keep it for later) and the inner needle cap (discard it)
-
Perform a flow check exactly as described in your pen's instructions—typically by selecting the flow check symbol (not a dose amount) and pressing the injection button while holding the pen upright until a drop appears
For single-use autoinjectors (e.g., Trulicity, some Wegovy presentations):
-
These devices come with the needle pre-attached and do not require needle assembly
-
No priming or flow check is needed
-
Follow the specific preparation steps in your device's instructions
For products requiring reconstitution (e.g., some exenatide ER formulations):
-
Follow the detailed mixing instructions in your product leaflet
-
Complete all preparation steps before proceeding to injection
Always refer to your specific product's patient information leaflet for exact preparation instructions, as incorrect preparation could affect your dose or treatment efficacy.
Step-by-Step Guide to Injecting Your GLP-1 Agonist
Once your device is prepared, follow these steps for safe injection. Select your injection site—the abdomen (at least 5 cm away from the navel), front or outer thigh, or upper outer arm are suitable areas. Clean the chosen site with an alcohol wipe using a circular motion and allow it to dry completely; injecting through wet skin can cause stinging.
For multi-dose dial-a-dose pens (e.g., Ozempic, Victoza, Saxenda):
-
Dial your prescribed dose using the dose selector. You should hear clicks as you turn the dial, and the dose window will display your prescribed amount
-
Double-check this matches your prescription
-
If you accidentally dial past your dose, you can typically dial backwards—consult your specific pen instructions
For fixed-dose autoinjectors (e.g., Trulicity, some Wegovy presentations):
-
No dose dialling is needed as these deliver a pre-set dose
-
Follow the specific unlocking or preparation steps in your device instructions
With your non-dominant hand, gently pinch a fold of skin at the injection site (particularly important if you are very lean). Hold the device with your dominant hand. Position the needle at a 90-degree angle to the skin surface (for standard short pen needles). In one smooth motion, insert the needle fully into the skin.
Press the injection button firmly and hold it down for the duration specified in your device instructions:
-
For Ozempic/Victoza/Saxenda: keep the button pressed until the dose counter returns to '0' and count slowly to 6
-
For Trulicity: press the injection button, listen for the first click, then wait for the second click/grey indicator
-
For other devices: follow the specific timing in your instructions
After the required time, release the injection button first, then withdraw the needle straight out from the skin. Release the pinched skin. You may notice a small drop of blood or medication at the injection site—this is normal. Apply gentle pressure with a clean cotton ball if needed, but do not rub the area.
For pens with detachable needles: carefully replace the outer needle cap using the cap provided, unscrew the needle, and dispose of it in your sharps container. Replace the pen cap.
For single-use autoinjectors: dispose of the entire device in your sharps container according to the instructions.
Choosing and Rotating Injection Sites Safely
Proper site selection and rotation are essential to prevent tissue changes that could affect medication absorption and glycaemic control. The three main injection areas are the abdomen, thighs, and upper arms, each offering advantages.
The abdomen is often preferred as it provides consistent absorption and is easily accessible. Inject at least 5 cm (approximately two finger-widths) away from your navel in any direction, and avoid the area within 5 cm of any scars or the waistline where clothing might rub. The thighs (front and outer aspects) are suitable for self-injection and particularly useful if you prefer not to inject in the abdomen. The upper outer arm can be used, though this site may be more difficult to reach for self-injection and is often better suited when a family member or carer assists.
Avoid injecting into areas that are tender, bruised, red, hard, or scarred. Do not inject into areas of lipohypertrophy (lumpy areas of fat tissue). If you have recently exercised vigorously, you may wish to choose a different injection site, though the clinical impact on GLP-1 receptor agonist absorption is less established than with insulin.
Systematic rotation prevents tissue damage. Following the Forum for Injection Technique (FIT UK) recommendations, imagine dividing each injection area into quadrants or sections. Use a different section with each injection, moving in a clockwise pattern. Keep injections within the same section at least 1 cm apart. Many patients find it helpful to maintain a simple injection diary or use a smartphone app to track sites used.
Some GLP-1 receptor agonists, particularly exenatide extended-release formulations, commonly cause small nodules at injection sites. These are usually harmless but can persist for weeks. Avoid injecting into existing nodules.
If you notice any lumps, bumps, or changes in skin texture at injection sites, inform your diabetes nurse or GP. These areas should be avoided until they resolve, as altered tissue can lead to unpredictable medication absorption and affect your blood glucose control.
Storing Your GLP-1 Pen and Disposing of Needles
Correct storage maintains medication efficacy and safety. Unopened GLP-1 devices must be stored in the refrigerator at 2°C to 8°C—typically on a middle shelf, not in the freezer compartment or door where temperature fluctuates. Never freeze your device; if it has been frozen, it must be discarded even if it subsequently thaws. Keep devices in their original carton to protect them from light.
Once you start using a device, storage requirements vary significantly by product. Always check your specific patient information leaflet for exact guidance:
-
Ozempic: up to 6 weeks at or below 30°C
-
Victoza/Saxenda: up to 1 month at or below 30°C
-
Trulicity: up to 14 days at or below 30°C
-
Other products: follow the specific guidance in your leaflet
Single-use autoinjectors should be used once and then disposed of; 'in-use' storage guidance does not apply to these devices.
Some patients prefer to continue refrigerating their in-use pen, which is acceptable, but remember to allow it to warm to room temperature before each injection. Always store pens with the cap on to protect the medication from light and prevent contamination.
Keep your device away from direct heat and sunlight—never leave it in a car, on a windowsill, or near radiators. When travelling, use an insulated medication travel case if you'll be away from refrigeration for extended periods. If you're flying, keep your device in hand luggage as hold baggage temperatures can freeze medications. Carry a letter from your GP confirming your need for injectable medication and needles.
Safe needle disposal is a legal and safety requirement. Never reuse needles—this increases infection risk and causes needle blunting, making injections more painful. For pens with detachable needles, use the outer cap provided to safely remove the needle after injection. Immediately after use, place needles or single-use devices in a rigid, puncture-proof sharps container (available via prescription from your GP or through local council schemes). When the container is three-quarters full, seal it and return it according to local arrangements—your pharmacy, GP surgery, or local authority collection point. Never dispose of sharps in household waste. Your local council website provides information on sharps disposal services in your area.
Common Problems and When to Contact Your Healthcare Team
Understanding common issues helps you manage your treatment confidently. If you notice air bubbles in your pen, small bubbles are harmless and won't affect your dose, but large air pockets should be removed by performing a flow check as described in your device instructions. If your pen seems jammed or the dose dial won't turn, don't force it—you may have reached the end of the pen's medication supply. Check the dose counter; if insufficient medication remains for your prescribed dose, you'll need a new pen.
Injection site reactions such as mild redness, itching, or small lumps are common with GLP-1 receptor agonists. For exenatide extended-release formulations, injection site nodules are very common and may persist for weeks but are typically harmless. Applying a cool compress may provide relief for discomfort. However, if you develop significant swelling, persistent pain, or signs of infection (increasing redness, warmth, pus), contact your GP promptly. Bruising occasionally occurs if a small blood vessel is nicked—this is harmless. If you're taking anticoagulants or antiplatelet medications, apply pressure for longer after injection to reduce bruising.
Gastrointestinal side effects including nausea, vomiting, diarrhoea, or constipation are the most frequently reported adverse effects of GLP-1 receptor agonists, particularly when starting treatment or increasing doses. These typically improve over several weeks as your body adjusts. Eating smaller, more frequent meals and avoiding high-fat foods may help. If vomiting is severe or persistent, preventing adequate fluid intake, seek medical advice as dehydration can affect kidney function.
If you miss a dose, follow the specific guidance for your medication:
-
For weekly semaglutide (Ozempic/Wegovy): if within 5 days of the missed dose, inject as soon as possible then resume your regular schedule; if more than 5 days have passed, skip the missed dose and inject on your next scheduled day
-
For weekly dulaglutide (Trulicity) or exenatide ER: if 3 or more days until your next scheduled dose, inject as soon as possible; otherwise, wait for your next scheduled dose
-
For daily liraglutide (Victoza/Saxenda): if within 12 hours of the usual time, inject as soon as possible; otherwise, wait for your next scheduled dose
-
Never double up doses
Contact your healthcare team urgently if you experience: severe, persistent abdominal pain (particularly if radiating to the back), which may indicate pancreatitis; right upper abdominal pain, fever or yellowing of the skin/eyes, which may indicate gallbladder problems; symptoms of hypoglycaemia (shakiness, sweating, confusion, rapid heartbeat), especially if taking GLP-1 receptor agonists alongside insulin or sulfonylureas; neck swelling, persistent hoarseness, or difficulty swallowing; or allergic reactions (rash, itching, difficulty breathing, facial swelling).
If you experience any suspected side effects, report them to the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk. Your diabetes nurse or pharmacist can provide personalised advice, and many surgeries offer telephone consultations for medication queries.
Frequently Asked Questions
How often do I need to inject my GLP-1 agonist pen?
Injection frequency depends on your specific medication: semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and exenatide extended-release are administered once weekly, whilst liraglutide (Victoza, Saxenda) and lixisenatide (Lyxumia) require once-daily injections.
Can I reuse needles for my GLP-1 pen injections?
No, never reuse needles as this increases infection risk, causes needle blunting that makes injections more painful, and may affect dose accuracy. Always use a new sterile needle for each injection and dispose of used needles immediately in a rigid sharps container.
What should I do if I miss a dose of my GLP-1 agonist?
For weekly medications like Ozempic or Wegovy, inject within 5 days of the missed dose then resume your regular schedule; if more than 5 days have passed, skip the missed dose. For daily medications like Victoza, inject within 12 hours of your usual time or wait for the next scheduled dose. Never double up doses.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript