Ozempic (semaglutide), a GLP-1 receptor agonist prescribed for type 2 diabetes and weight management in the UK, can significantly reduce appetite and food intake. This reduction, whilst therapeutically beneficial, may lead to lower consumption of essential vitamins and minerals. Understanding what vitamins to take with Ozempic helps patients maintain optimal nutritional status during treatment. Whilst Ozempic does not directly deplete specific nutrients, the associated decreased dietary intake and gastrointestinal effects can create nutritional gaps. This article examines key micronutrients that warrant attention, safe supplementation practices, and when to seek medical advice regarding vitamin needs whilst taking Ozempic.
Summary: Ozempic does not directly deplete vitamins, but reduced appetite may require attention to vitamin D, B-complex vitamins (especially B12 if also taking metformin), calcium, iron, and magnesium through diet or targeted supplementation based on individual assessment.
- Semaglutide is a GLP-1 receptor agonist that reduces appetite and slows gastric emptying, potentially decreasing overall nutrient intake.
- Vitamin D supplementation (10 micrograms daily) is recommended for UK adults during autumn and winter, particularly important when dietary intake is reduced.
- Unlike metformin, Ozempic has no established direct link to vitamin B12 depletion, though reduced intake of animal-source foods may affect B12 status over time.
- Nutritional assessment should be individualised based on dietary patterns, symptoms, and risk factors rather than routine supplementation for all patients.
- Patients should seek medical advice if experiencing persistent fatigue, neurological symptoms, hair loss, or severe gastrointestinal effects that may indicate deficiency.
Table of Contents
Understanding Ozempic and Nutritional Needs
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. At higher doses, semaglutide is available under the brand name Wegovy for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, alongside diet and physical activity. The medication works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite through effects on the central nervous system.
These mechanisms of action, whilst therapeutically beneficial, can impact nutritional intake. The delayed gastric emptying and reduced appetite often lead to substantially decreased food consumption, which may result in lower intake of essential vitamins and minerals. Patients frequently report early satiety, nausea, and changes in food preferences, all of which can contribute to a more restricted dietary pattern. Additionally, the gastrointestinal effects of Ozempic, including occasional vomiting and diarrhoea, may further compromise nutritional status.
For individuals taking Ozempic, maintaining adequate nutrition becomes particularly important as the body undergoes metabolic changes and, in many cases, significant weight loss. Whilst the medication itself does not directly deplete specific vitamins, the associated reduction in food intake and altered eating patterns can create nutritional gaps. Understanding which vitamins and minerals may require additional attention helps patients maintain optimal health whilst benefiting from their prescribed treatment. Healthcare professionals should consider nutritional assessment for those at risk of deficiencies as part of comprehensive diabetes or weight management care.
It is important to note that semaglutide is contraindicated during pregnancy and breastfeeding. Women of childbearing potential should use effective contraception when treated with semaglutide and discontinue treatment at least 2 months before a planned pregnancy due to the long half-life of the medication.
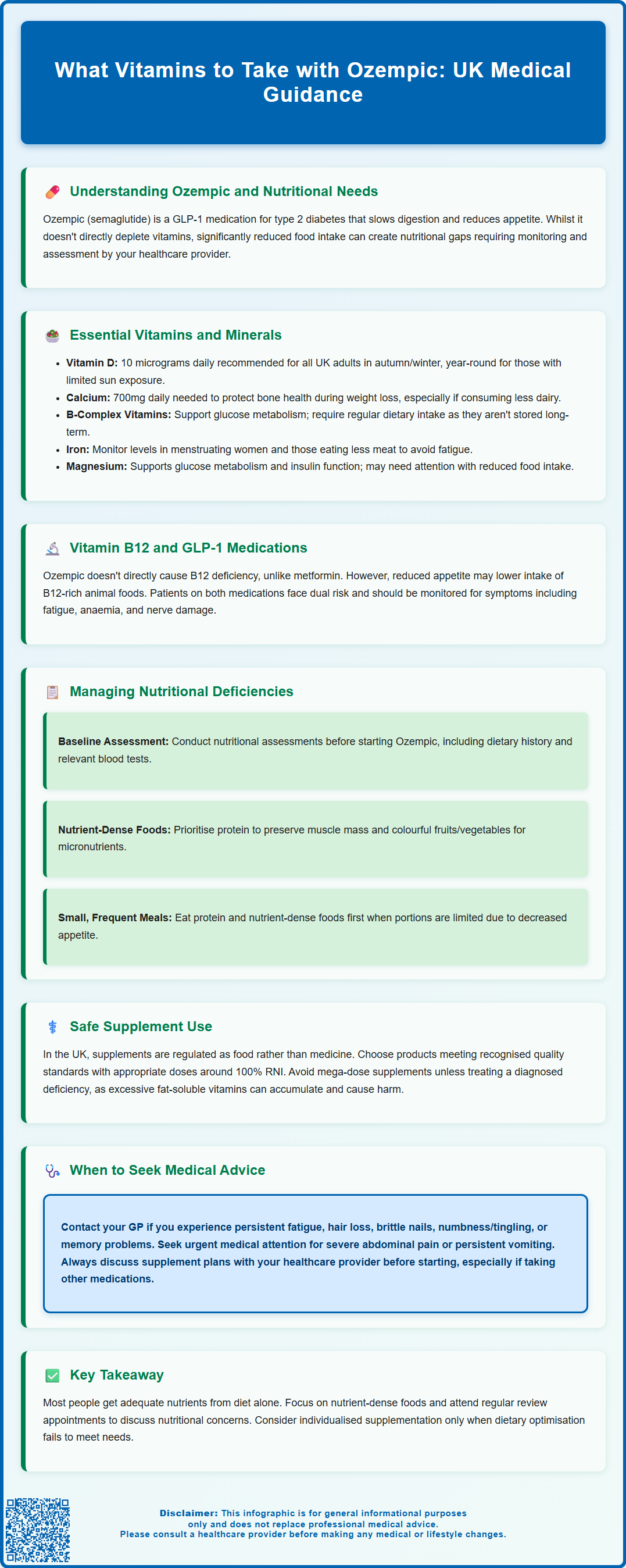
Essential Vitamins and Minerals When Taking Ozempic
Several key micronutrients warrant particular attention for patients prescribed Ozempic, primarily due to reduced dietary intake rather than direct drug interactions. Vitamin D plays a crucial role in bone health, immune function, and may influence glucose metabolism. Deficiency is already prevalent in the UK population, with the NHS recommending that all adults consider taking a daily supplement containing 10 micrograms (400 IU) of vitamin D during autumn and winter months. People with limited sun exposure, darker skin tones, or who cover most of their skin when outdoors should consider taking this supplement year-round. Patients experiencing reduced appetite may consume less vitamin D-rich foods such as oily fish, eggs, and fortified dairy products.
Calcium intake may also decline when overall food consumption decreases, especially if dairy products are less well tolerated or consumed in smaller quantities. Adequate calcium is essential for bone health, particularly important for patients losing significant weight, as rapid weight loss can affect bone mineral density. The UK reference nutrient intake (RNI) for adults is 700mg daily, though some individuals may require more depending on age and other risk factors.
B-complex vitamins, particularly thiamine (B1), folate (B9), and vitamin B12, deserve consideration. While vitamin B12 is stored in significant amounts in the liver (with stores potentially lasting several years), thiamine and folate require more regular dietary intake. Thiamine is essential for glucose metabolism and neurological function, whilst folate supports cell division and DNA synthesis. Iron status should also be monitored in at-risk individuals, especially menstruating women or those with restricted meat intake, as iron deficiency can cause fatigue and may be mistaken for medication side effects. Magnesium, involved in over 300 enzymatic reactions including glucose metabolism and insulin action, may also require attention in those with poor dietary intake or significant gastrointestinal symptoms.
Vitamin B12 and GLP-1 Medications
Vitamin B12 (cobalamin) requires specific consideration for patients taking Ozempic, though the relationship is more complex than with some other diabetes medications. Unlike metformin, which has a well-established association with vitamin B12 malabsorption through interference with calcium-dependent B12-intrinsic factor complex absorption in the terminal ileum, there is no official link between GLP-1 receptor agonists and direct B12 depletion. However, several factors may indirectly affect B12 status in patients taking Ozempic.
Vitamin B12 is found predominantly in animal-source foods including meat, fish, eggs, and dairy products. Patients experiencing reduced appetite and early satiety may consume smaller portions of these B12-rich foods, potentially leading to inadequate intake over time. Those following vegetarian or vegan diets are at particularly high risk. Furthermore, many patients taking Ozempic for type 2 diabetes are also prescribed metformin, creating a dual risk for B12 deficiency. The MHRA recommends checking vitamin B12 levels in patients on long-term metformin therapy if anaemia or peripheral neuropathy develops, and considering periodic monitoring in those at risk of reduced vitamin B12 levels.
Vitamin B12 deficiency can manifest as macrocytic anaemia, fatigue, neurological symptoms including peripheral neuropathy, cognitive changes, and mood disturbances. These symptoms may develop insidiously and could be attributed to diabetes complications or medication side effects if B12 status is not assessed. For patients taking Ozempic, especially those also prescribed metformin or following plant-based diets, B12 measurement should be considered if symptoms develop. Treatment of confirmed deficiency typically follows BNF guidance, which may include intramuscular hydroxocobalamin injections for significant deficiency or oral supplementation in milder cases, based on individual assessment and serum B12 levels.
Managing Nutritional Deficiencies During Treatment
Proactive nutritional management is important for patients taking Ozempic to prevent deficiencies whilst maximising the therapeutic benefits of treatment. Healthcare professionals should consider a baseline nutritional assessment before initiating therapy for those at higher risk, including dietary history, relevant blood tests where clinically indicated (such as full blood count, vitamin B12, vitamin D, and ferritin), and identification of risk factors for malnutrition. This establishes a reference point for monitoring throughout treatment.
Patients should receive dietary counselling emphasising nutrient density rather than simply calorie restriction. When appetite is reduced and portion sizes are smaller, every bite should contribute meaningful nutrition. Prioritising protein-rich foods helps preserve lean muscle mass during weight loss, whilst incorporating a variety of colourful vegetables and fruits ensures adequate micronutrient intake. Small, frequent meals may be better tolerated than larger portions, and patients should be encouraged to eat protein and nutrient-dense foods first when appetite is limited.
Regular monitoring becomes particularly important for patients with significant weight loss, persistent gastrointestinal symptoms, or restricted dietary patterns. Follow-up appointments should include assessment of dietary intake, weight trends, and symptoms that might suggest nutritional deficiencies such as fatigue, hair loss, brittle nails, or neurological symptoms. Repeat blood tests may be indicated based on clinical assessment rather than routine testing for all patients.
For patients who struggle to meet nutritional needs through food alone despite dietary optimisation, targeted supplementation may be appropriate. This should be individualised based on identified deficiencies, dietary restrictions, and clinical presentation rather than routine supplementation for all patients. Referral to a registered dietitian should be considered for persistent gastrointestinal intolerance, complex dietary needs, or those with multiple nutritional concerns.
Safe Supplement Use with Ozempic
When supplementation is deemed necessary, patients should be guided towards safe and appropriate products. In the UK, vitamins and minerals are regulated as food supplements rather than medicines, and quality can vary considerably between products. Patients should look for supplements that meet recognised quality standards and contain appropriate doses. The NHS advises that most people can obtain necessary nutrients from a balanced diet, but acknowledges that certain groups may benefit from specific supplements, such as the recommended 10 micrograms (400 IU) of vitamin D daily during autumn and winter months.
A standard multivitamin and mineral supplement providing around 100% of the reference nutrient intake (RNI) for key micronutrients may be suitable for some patients taking Ozempic, particularly during periods of very restricted intake or rapid weight loss. However, patients should avoid mega-dose supplements unless specifically recommended for a diagnosed deficiency, as excessive intake of certain vitamins and minerals can cause adverse effects. Fat-soluble vitamins (A, D, E, and K) accumulate in body tissues and excessive intake can be harmful.
Timing of supplement intake may influence tolerability and absorption. Taking supplements with food, when possible, often reduces gastrointestinal side effects and may improve absorption of certain nutrients. However, patients experiencing significant nausea from Ozempic should be advised that some supplements, particularly iron, can exacerbate this symptom. In such cases, alternative formulations or timing adjustments may help. While semaglutide's delayed gastric emptying may affect the rate of absorption of some oral medicines, this is usually not clinically relevant for vitamin and mineral supplements.
There are no known direct drug interactions between Ozempic and vitamin or mineral supplements that would contraindicate their concurrent use. However, patients should inform their healthcare provider about all supplements they are taking, as some may affect blood glucose levels or interact with other prescribed medications. For example, vitamin K supplements can affect INR control in patients taking warfarin, and patients should discuss any supplement use with their prescriber.
When to Seek Medical Advice About Vitamin Supplementation
Patients taking Ozempic should contact their GP or diabetes specialist nurse if they experience symptoms that might indicate nutritional deficiency. These include persistent fatigue not explained by blood glucose levels, unusual hair loss, brittle nails, frequent infections suggesting immune compromise, numbness or tingling in the hands or feet, difficulty concentrating or memory problems, persistent mouth ulcers, or unexplained bruising or bleeding. Whilst these symptoms can have various causes, they may indicate vitamin or mineral deficiencies requiring investigation.
Patients should also be aware of specific warning signs related to semaglutide treatment. They should seek urgent medical attention if they develop symptoms of acute pancreatitis, such as severe and persistent abdominal pain which may radiate to the back, or symptoms of gallbladder disease. In these cases, they should stop taking semaglutide and contact their healthcare provider immediately or call NHS 111 for advice. For severe symptoms or life-threatening reactions, patients should call 999 or go to A&E.
Before starting any new supplement regimen, patients should discuss this with their healthcare provider, particularly if considering doses above standard multivitamin levels. This is especially important for individuals with other medical conditions, those taking multiple medications, or anyone who has previously experienced adverse reactions to supplements. Pregnant women or those planning pregnancy require specialist advice, as nutritional needs differ and semaglutide must be discontinued at least 2 months before a planned pregnancy.
Patients should seek urgent medical attention if they develop severe or persistent vomiting or diarrhoea whilst taking Ozempic, as this may lead to dehydration and electrolyte disturbances beyond simple vitamin deficiency. Persistent severe gastrointestinal symptoms may warrant medication review, dose adjustment or temporary pause in treatment. Regular review appointments provide opportunity to discuss nutritional concerns and assess whether current strategies are adequate. Collaborative management between patients and healthcare teams ensures that nutritional health is maintained whilst achieving optimal therapeutic outcomes from Ozempic treatment.
Frequently Asked Questions
Does Ozempic cause vitamin B12 deficiency?
Ozempic does not directly cause vitamin B12 deficiency like metformin does. However, reduced appetite and lower intake of B12-rich animal foods may indirectly affect B12 status, particularly in patients also taking metformin or following plant-based diets.
Should everyone taking Ozempic take vitamin supplements?
Not necessarily. Supplementation should be individualised based on dietary intake, symptoms, and identified deficiencies rather than routine for all patients. A standard multivitamin may be appropriate during periods of very restricted intake, but targeted supplementation based on clinical assessment is preferred.
When should I contact my doctor about vitamins whilst taking Ozempic?
Contact your GP if you experience persistent fatigue, unusual hair loss, numbness or tingling in hands or feet, frequent infections, or other symptoms suggesting nutritional deficiency. Always discuss any new supplement regimen with your healthcare provider before starting.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












