What to eat on Ozempic is a common concern for patients prescribed this GLP-1 receptor agonist for type 2 diabetes. Ozempic (semaglutide) slows gastric emptying and reduces appetite, making dietary adjustments essential for managing side effects and maintaining adequate nutrition. Whilst no specific restrictive diet is required, choosing nutrient-dense foods—lean proteins, non-starchy vegetables, and complex carbohydrates—can optimise blood glucose control and minimise gastrointestinal symptoms such as nausea and constipation. Understanding which foods to prioritise and which to limit helps you tolerate treatment better whilst supporting your diabetes management goals. This guide provides practical, evidence-based advice aligned with UK clinical guidance to help you eat well on Ozempic.
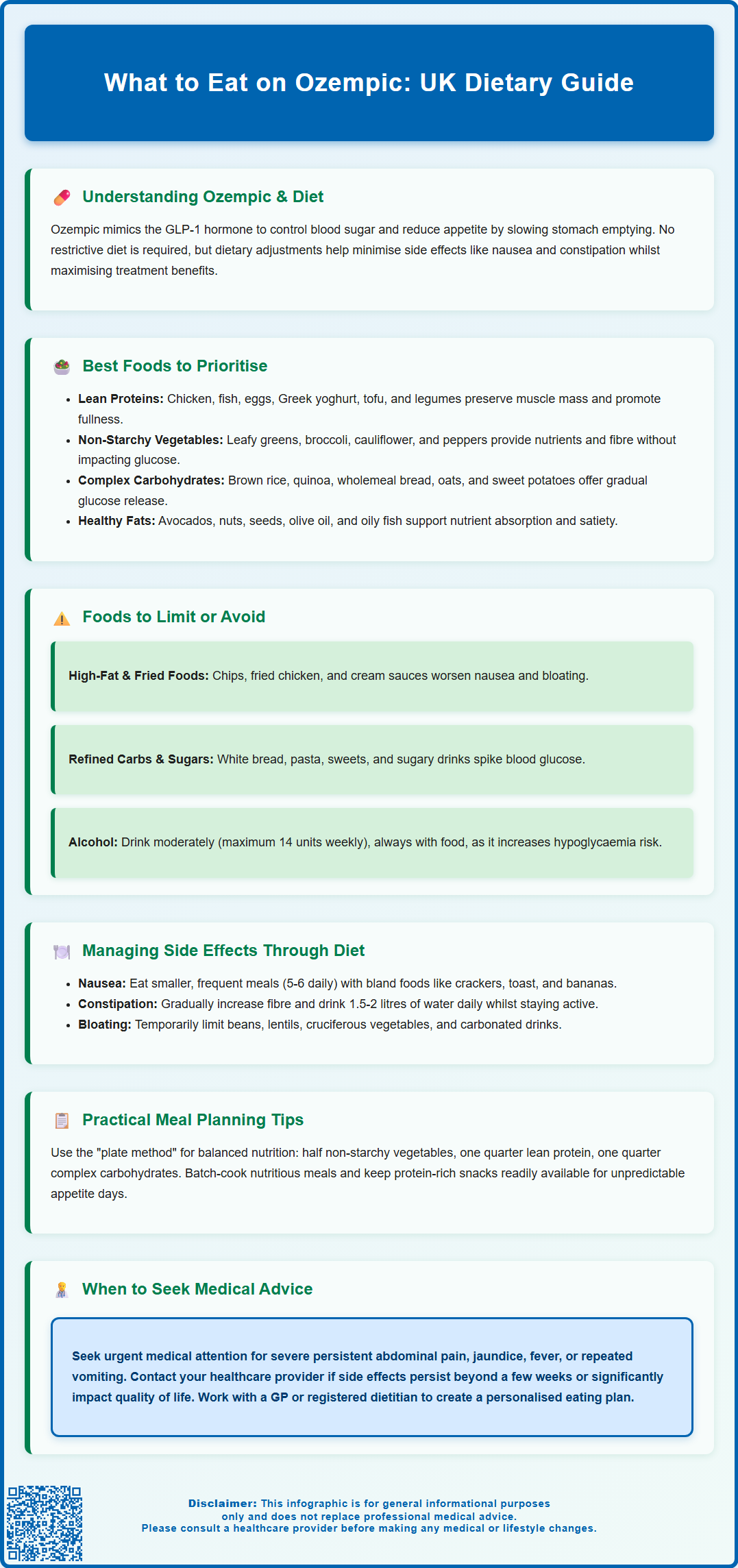
Summary: On Ozempic, prioritise lean proteins, non-starchy vegetables, complex carbohydrates, and healthy fats whilst limiting high-fat, fried, and refined sugary foods to manage side effects and support blood glucose control.
- Ozempic (semaglutide) is a GLP-1 receptor agonist that slows gastric emptying, reduces appetite, and helps regulate blood glucose in type 2 diabetes.
- Lean proteins (chicken, fish, eggs, Greek yoghurt), non-starchy vegetables, and wholegrain complex carbohydrates form the foundation of an optimal Ozempic diet.
- High-fat and fried foods, refined carbohydrates, and added sugars should be limited as they worsen gastrointestinal side effects and impair glycaemic control.
- Common side effects include nausea, constipation, and bloating; eating smaller, frequent meals and increasing fibre gradually can help manage these symptoms.
- Patients taking insulin or sulfonylureas alongside Ozempic should discuss dose adjustments with their diabetes team to reduce hypoglycaemia risk as appetite decreases.
- Seek urgent medical attention for severe persistent abdominal pain, jaundice, fever, or repeated vomiting, which may indicate serious complications such as pancreatitis.
Table of Contents
Understanding Ozempic and Dietary Considerations
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in response to food intake, suppresses glucagon release (both in a glucose-dependent manner), and slows gastric emptying. This mechanism not only helps to regulate blood glucose levels but also reduces appetite and promotes a feeling of fullness, which can lead to weight loss as a secondary benefit.
Whilst Ozempic is not primarily a weight-loss medication (though semaglutide is licensed for weight management under the brand name Wegovy at higher doses), many patients experience reduced appetite and changes in their relationship with food. Understanding how to adapt your diet whilst taking Ozempic is essential for maximising therapeutic benefits, minimising side effects, and maintaining adequate nutrition. The medication does not require a specific restrictive diet, but certain dietary adjustments can help you tolerate the treatment better and support your overall health goals.
Dietary considerations become particularly important because the slowed gastric emptying and reduced appetite can make it challenging to consume adequate nutrients, especially protein, vitamins, and minerals. Additionally, some foods may exacerbate common gastrointestinal side effects such as nausea, bloating, and constipation. Working with your GP or a registered dietitian can help you develop an individualised eating plan that aligns with your diabetes management goals, addresses any nutritional deficiencies, and supports sustainable lifestyle changes. The NICE guidelines for type 2 diabetes emphasise the importance of dietary modification alongside pharmacological treatment, making nutritional awareness a cornerstone of effective diabetes care.
Important safety note: Ozempic is not recommended during pregnancy or breastfeeding. If you're planning a pregnancy, you should stop taking Ozempic at least 2 months beforehand and discuss alternative diabetes management with your healthcare team. If you experience severe, persistent abdominal pain (which may radiate to your back), yellowing of the skin/eyes (jaundice), or fever, seek urgent medical attention as these could indicate serious conditions such as pancreatitis or gallbladder disease.
Best Foods to Eat While Taking Ozempic
Choosing nutrient-dense, easily digestible foods can help you maintain adequate nutrition whilst managing the appetite-suppressing effects of Ozempic. Lean protein sources should form a central part of your diet, as protein helps preserve muscle mass during weight loss, promotes satiety, and supports stable blood glucose levels. Excellent options include skinless chicken breast, turkey, white fish (such as cod or haddock), eggs, low-fat Greek yoghurt, cottage cheese, and plant-based proteins like tofu, lentils, and chickpeas. Aim to include a portion of protein with each meal to support your body's nutritional needs.
Non-starchy vegetables are particularly valuable, as they provide essential vitamins, minerals, and fibre whilst being low in calories and having minimal impact on blood glucose. Focus on leafy greens (spinach, kale, rocket), cruciferous vegetables (broccoli, cauliflower, Brussels sprouts), courgettes, peppers, tomatoes, and mushrooms. These foods can help you feel satisfied without overwhelming your digestive system, which may be more sensitive due to slowed gastric emptying.
Complex carbohydrates with a low glycaemic index should replace refined carbohydrates in your diet. Choose wholegrain options such as brown rice, quinoa, wholemeal bread, rolled oats, and sweet potatoes. These foods release glucose more gradually into the bloodstream, helping to maintain stable blood sugar levels and providing sustained energy. Healthy fats in moderate amounts are also important for nutrient absorption and satiety. Include sources such as avocados, nuts (almonds, walnuts), seeds (chia, flaxseed), olive oil, and oily fish like salmon or mackerel, which also provide beneficial omega-3 fatty acids.
Staying well-hydrated is crucial, as adequate fluid intake can help prevent constipation (a common side effect) and support overall wellbeing. Water should be your primary beverage, though herbal teas and diluted sugar-free squash are acceptable alternatives.
For balanced meal planning, consider following the NHS Eatwell Guide or the Diabetes UK plate method, which recommends filling half your plate with non-starchy vegetables, one quarter with lean protein, and one quarter with complex carbohydrates.
Foods to Limit or Avoid on Ozempic
Certain foods can exacerbate the gastrointestinal side effects of Ozempic or interfere with optimal blood glucose control, making them worth limiting or avoiding, particularly during the initial titration period. High-fat and fried foods are among the most problematic, as they delay gastric emptying even further and can trigger or worsen nausea, bloating, and indigestion. Foods such as chips, fried chicken, pastries, cream-based sauces, and fatty cuts of meat may sit heavily in your stomach and cause considerable discomfort. The combination of Ozempic's mechanism and high-fat meals can create an unpleasant sensation of prolonged fullness.
Refined carbohydrates and added sugars should be minimised, as they cause rapid spikes in blood glucose levels, counteracting the glycaemic benefits of Ozempic. Limit white bread, white pasta, white rice, sugary cereals, biscuits, cakes, sweets, and sugar-sweetened beverages. These foods provide little nutritional value and can make diabetes management more challenging. If you do consume carbohydrates, pair them with protein or healthy fats to slow glucose absorption.
Highly processed foods often contain excessive sodium, unhealthy fats, and additives that may worsen gastrointestinal symptoms. Ready meals, processed meats (sausages, bacon, deli meats), and packaged snacks typically fall into this category. Spicy and acidic foods may also trigger or intensify nausea and heartburn in some individuals taking Ozempic. If you notice that curries, chilli-based dishes, citrus fruits, or tomato-based sauces cause discomfort, consider reducing your intake or avoiding them during periods when side effects are most pronounced.
Alcohol warrants particular caution, as it can affect blood glucose levels unpredictably, increase the risk of hypoglycaemia (especially if you're taking other diabetes medications), and may worsen nausea. If you choose to drink, do so in moderation (following UK Chief Medical Officers' guidelines of no more than 14 units per week) and always consume alcohol with food. Carbonated beverages may increase bloating in some people – if you notice they worsen your symptoms, consider limiting them.
Important: If you're also taking insulin or sulfonylurea medications (such as gliclazide) and your appetite decreases significantly on Ozempic, discuss possible dose adjustments with your diabetes team to reduce your risk of hypoglycaemia (low blood sugar).
Managing Common Side Effects Through Diet
Gastrointestinal side effects are the most frequently reported adverse reactions to Ozempic, particularly during the initial weeks of treatment and following dose increases. Strategic dietary choices can significantly reduce the severity and duration of these symptoms. For nausea, which affects a substantial proportion of patients, eating smaller, more frequent meals (five to six times daily) rather than three large meals can help prevent overwhelming your digestive system. Bland, easily digestible foods such as plain crackers, toast, bananas, rice, and boiled potatoes may be better tolerated when nausea is prominent. Ginger tea or ginger biscuits may provide natural relief for some individuals, though evidence for this remains largely anecdotal.
Avoiding lying down immediately after eating and ensuring you eat slowly, chewing thoroughly, can reduce the likelihood of nausea and reflux. Some patients find that cold or room-temperature foods are better tolerated than hot meals when experiencing nausea. Constipation is another common concern, resulting from slowed gastrointestinal motility. Increasing your fibre intake gradually through fruits (particularly prunes, pears, and berries), vegetables, wholegrain cereals, and pulses can help maintain regular bowel movements. However, introduce fibre slowly to avoid exacerbating bloating.
For diarrhoea, which can also occur, focus on staying hydrated with regular sips of water or oral rehydration solutions. Temporarily choose lower-fibre, low-fat, bland foods such as white toast, rice, bananas, and plain potatoes. Soluble fibre from oats may help firm stools. Avoid caffeine, alcohol, and spicy foods until symptoms improve.
Adequate hydration is essential for preventing and managing both constipation and diarrhoea—aim for at least 1.5 to 2 litres of water daily, unless otherwise advised by your healthcare provider. Regular physical activity, even gentle walking, can also stimulate bowel function. For bloating and abdominal discomfort, identify and temporarily reduce foods known to produce gas, such as beans, lentils, cruciferous vegetables, onions, and carbonated drinks. Peppermint tea may provide symptomatic relief for some individuals.
Seek urgent medical attention if you experience severe, persistent abdominal pain (which may radiate to your back), yellowing of the skin/eyes (jaundice), fever, or repeated vomiting/inability to keep fluids down. If you experience hypoglycaemia (low blood sugar) and are taking insulin or sulfonylureas, contact your healthcare team promptly to adjust your doses.
If side effects persist beyond the first few weeks, become severe, or significantly impact your quality of life, contact your GP or diabetes specialist nurse. In some cases, a slower dose titration or additional symptomatic management may be appropriate. Never discontinue Ozempic without medical advice, as abrupt cessation can affect your diabetes control. You can report any suspected side effects to the MHRA through the Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Meal Planning and Practical Tips for Ozempic Users
Successful dietary management whilst taking Ozempic requires thoughtful planning and a flexible approach that accommodates your changing appetite and tolerance. Meal timing is particularly important—consider administering your weekly Ozempic injection on the same day each week. Side effect timing varies between individuals, but some people experience more pronounced effects in the days immediately after their injection. Observe your own pattern and consider planning lighter meals for when your symptoms tend to be strongest.
Portion control becomes easier with Ozempic due to enhanced satiety signals, but it's important to ensure you're still meeting your nutritional requirements despite eating less. Use smaller plates to make reduced portions appear more satisfying, and focus on nutrient density rather than calorie density. A useful framework is the "plate method" recommended by Diabetes UK and aligned with the NHS Eatwell Guide: fill half your plate with non-starchy vegetables, one quarter with lean protein, and one quarter with complex carbohydrates. This approach ensures balanced nutrition whilst supporting blood glucose management.
Meal preparation can be invaluable when appetite is unpredictable. Batch-cook nutritious meals such as vegetable soups, chicken and vegetable stir-fries, or bean-based stews that can be portioned and frozen. Having healthy options readily available reduces the temptation to skip meals or resort to less nutritious convenience foods when you're not feeling well. Keep simple, protein-rich snacks accessible, such as hard-boiled eggs, Greek yoghurt, cheese portions, or unsalted nuts, to maintain energy levels between meals.
If you're also taking insulin or sulfonylureas, keep hypo treatments (such as glucose tablets, fruit juice, or dextrose gel) readily available, especially when your appetite is reduced. Discuss with your diabetes team whether your insulin or sulfonylurea doses need adjustment as your eating patterns change with Ozempic.
Monitoring and adjustment are key to long-term success. Keep a food diary noting what you eat, portion sizes, and any symptoms experienced. This can help you identify patterns and problematic foods. Regular blood glucose monitoring (as advised by your diabetes team) will help you understand how different foods affect your levels. Schedule regular reviews with your GP or practice nurse to assess your progress, discuss any nutritional concerns, and adjust your diabetes management plan as needed. If weight loss is significant or you're struggling to maintain adequate nutrition, request a referral to a registered dietitian who can provide specialised support tailored to your individual circumstances and ensure you're meeting all your nutritional needs whilst taking Ozempic.
Frequently Asked Questions
Can I eat normally whilst taking Ozempic?
You can eat normally on Ozempic, but many patients find their appetite decreases and certain foods (especially high-fat or fried items) worsen side effects like nausea. Focus on smaller portions of nutrient-dense foods—lean proteins, vegetables, and wholegrain carbohydrates—to maintain adequate nutrition whilst managing symptoms.
What foods should I avoid on Ozempic?
Limit high-fat and fried foods, refined carbohydrates, added sugars, and highly processed items, as these can worsen gastrointestinal side effects and impair blood glucose control. Spicy or acidic foods may also trigger nausea in some individuals.
How can I manage nausea from Ozempic through diet?
Eat smaller, more frequent meals (five to six daily) with bland, easily digestible foods such as toast, crackers, bananas, and rice. Avoid lying down immediately after eating, eat slowly, and consider ginger tea for natural relief.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










