Weekly weight loss injections, primarily semaglutide (Wegovy), are prescription-only GLP-1 receptor agonist medications administered once weekly to support weight management in adults with obesity or overweight. These injections work by mimicking natural hormones that regulate appetite and metabolism, helping reduce caloric intake when combined with lifestyle changes. Approved by the MHRA and recommended by NICE for specific patient groups, they represent a medical intervention requiring ongoing healthcare supervision rather than a cosmetic quick fix. Eligibility depends on BMI thresholds, weight-related health conditions, and commitment to dietary and physical activity modifications. Access through the NHS follows strict clinical pathways with treatment duration typically limited to two years.
Summary: Weekly weight loss injections are prescription GLP-1 receptor agonist medications, primarily semaglutide (Wegovy), administered once weekly to support weight management alongside lifestyle changes in eligible adults with obesity.
- Semaglutide (Wegovy) is a GLP-1 receptor agonist that suppresses appetite, slows gastric emptying, and improves glucose metabolism through weekly subcutaneous injection.
- NICE recommends semaglutide for adults with BMI ≥35 kg/m² or BMI 30-34.9 kg/m² with weight-related comorbidities, with lower thresholds for certain ethnic groups.
- Common side effects include nausea, vomiting, diarrhoea, and constipation, typically occurring during dose escalation; serious risks include pancreatitis and gallbladder problems.
- NHS access requires GP referral to specialist weight management services (tier 3), with treatment limited to 2 years and continuation dependent on achieving weight loss targets.
- Treatment must be prescribed by registered healthcare professionals following comprehensive assessment, baseline investigations, and ongoing medical supervision throughout the treatment period.
Table of Contents
- What Are Weekly Weight Loss Injections?
- How Do GLP-1 Injections Work for Weight Loss?
- Available Weekly Injections in the UK
- Who Can Use Weekly Weight Loss Injections?
- Side Effects and Safety Considerations
- Getting Weekly Weight Loss Injections Through the NHS
- Scientific References
- Frequently Asked Questions
What Are Weekly Weight Loss Injections?
Weekly weight loss injections refer primarily to semaglutide (marketed as Wegovy), a medication administered once per week via subcutaneous injection to support weight management in adults with obesity or overweight. Wegovy belongs to a group called glucagon-like peptide-1 (GLP-1) receptor agonists, originally developed for type 2 diabetes management but now licensed for weight loss at higher doses. While liraglutide (Saxenda) is another GLP-1 receptor agonist approved for weight management in the UK, it requires daily rather than weekly administration.
These injections are not cosmetic treatments or quick fixes, but prescription-only medicines intended for use alongside lifestyle modifications including dietary changes and increased physical activity. They are designed for individuals who meet specific clinical criteria related to body mass index (BMI) and associated health conditions. The weekly administration schedule of Wegovy offers convenience compared to daily injections, potentially improving adherence to treatment.
The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Wegovy following rigorous clinical trials demonstrating its efficacy and safety profile. However, it remains part of a comprehensive weight management programme rather than a standalone solution. Healthcare professionals assess suitability on an individual basis, considering medical history, current medications, and realistic weight loss goals. It is important to understand that these injections work by influencing appetite regulation and metabolic processes, requiring ongoing medical supervision throughout the treatment period.
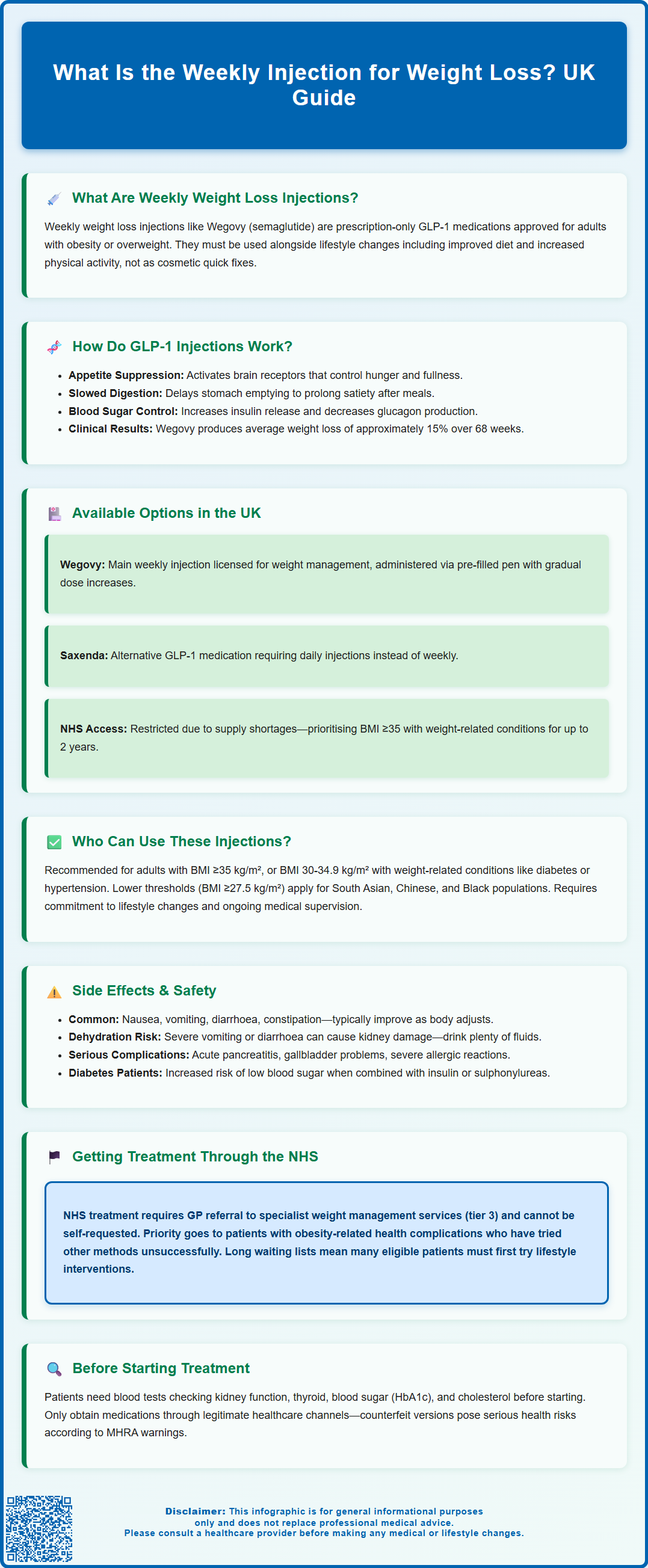
How Do GLP-1 Injections Work for Weight Loss?
GLP-1 receptor agonists mimic the action of glucagon-like peptide-1, a naturally occurring hormone produced in the intestines in response to food intake. This hormone plays a crucial role in regulating appetite, glucose metabolism, and energy balance. When administered as a weekly injection, these synthetic analogues bind to GLP-1 receptors in various tissues, including the brain, pancreas, and gastrointestinal tract, triggering multiple physiological responses that contribute to weight reduction.
The primary mechanism involves appetite suppression through effects on the hypothalamus, the brain region responsible for hunger and satiety signals. By activating GLP-1 receptors in this area, the medication increases feelings of fullness and reduces hunger between meals, leading to decreased caloric intake. Additionally, these injections slow gastric emptying, meaning food remains in the stomach longer, prolonging the sensation of satiety after eating and reducing the desire to consume additional food.
Beyond appetite regulation, GLP-1 receptor agonists influence glucose-dependent insulin secretion from pancreatic beta cells, improving glycaemic control particularly in individuals with type 2 diabetes or prediabetes. They also reduce glucagon secretion, a hormone that raises blood glucose levels, further contributing to metabolic improvements. The combined effects on appetite, gastric motility, and glucose homeostasis create an environment conducive to sustained weight loss when paired with appropriate lifestyle interventions. Clinical trials of semaglutide 2.4 mg (Wegovy), such as the STEP programme, have demonstrated average weight reductions of approximately 15% of initial body weight over 68 weeks, significantly greater than the 5-10% typically seen with liraglutide 3.0 mg. Individual responses vary considerably based on adherence, baseline characteristics, and concurrent lifestyle modifications.
Available Weekly Injections in the UK
In the United Kingdom, semaglutide (Wegovy) represents the primary weekly injection specifically licensed for chronic weight management. Wegovy received MHRA approval and is available through both NHS and private healthcare pathways for eligible patients. The medication is administered once weekly via a pre-filled injection pen, with doses gradually increased over several months to minimise gastrointestinal side effects. The standard maintenance dose is 2.4 mg weekly, though some patients may remain on lower doses depending on tolerability and response.
Another GLP-1 receptor agonist available in the UK is liraglutide (Saxenda), though this requires daily rather than weekly administration at a maximum dose of 3.0 mg. Whilst not fitting the weekly injection category, it serves as an alternative for patients who may prefer or require daily dosing. Dulaglutide (Trulicity) is a weekly GLP-1 injection licensed for type 2 diabetes management in the UK, but it is not approved for obesity treatment and should not be used off-label for weight management in individuals without diabetes.
Availability of these medications has been affected by global supply constraints, with the NHS implementing prescribing restrictions to prioritise patients with greatest clinical need, as outlined in NHS England's Medicines Supply Notifications. According to NICE Technology Appraisal 875, semaglutide is recommended for weight management in adults with at least one weight-related comorbidity and a BMI of 35 kg/m² or greater, or a BMI of 30-34.9 kg/m² with exceptional circumstances. NHS-funded treatment is typically limited to a maximum of 2 years. Private prescriptions are available through registered healthcare providers, though costs vary considerably. Patients should only obtain these medications through legitimate healthcare channels, as the MHRA has issued alerts regarding counterfeit products that pose serious health risks.
Who Can Use Weekly Weight Loss Injections?
Weekly weight loss injections are not suitable for everyone seeking to lose weight. NICE Technology Appraisal 875 specifies that semaglutide for weight management should be considered for adults with a BMI of 35 kg/m² or above, or a BMI of 30-34.9 kg/m² in the presence of at least one weight-related comorbidity such as type 2 diabetes, hypertension, dyslipidaemia, obstructive sleep apnoea, or cardiovascular disease. For individuals from Black, Asian, and other minority ethnic backgrounds, NICE Public Health Guideline 46 recommends lower BMI thresholds, with obesity risk identified at BMI ≥27.5 kg/m² for South Asian, Chinese, and Black populations, reflecting differences in body composition and metabolic risk.
Before prescribing, healthcare professionals conduct comprehensive assessments including medical history, current medications, and screening for precautions. The UK Summary of Product Characteristics (SmPC) includes special warnings regarding medullary thyroid carcinoma and multiple endocrine neoplasia syndrome type 2; while not absolute contraindications in the UK, patients with personal or family history of these conditions should discuss risks with their healthcare provider. These medications should not be used during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception during treatment. For semaglutide specifically, the SmPC advises discontinuation at least 2 months before a planned pregnancy.
Patients must demonstrate commitment to lifestyle modification, including dietary changes and increased physical activity, as these medications are intended as adjuncts rather than replacements for behavioural interventions. Those with severe gastrointestinal disease, including inflammatory bowel disease or gastroparesis, may not be suitable candidates. Individuals with a history of pancreatitis require careful evaluation, as GLP-1 receptor agonists have been associated with pancreatitis in some cases, though causality remains uncertain. Healthcare providers also consider mental health status, as rapid weight loss can affect psychological wellbeing, and patients with active eating disorders typically require specialist input before commencing treatment.
Side Effects and Safety Considerations
Gastrointestinal side effects represent the most common adverse reactions to weekly weight loss injections, affecting the majority of users to varying degrees. Nausea, vomiting, diarrhoea, constipation, and abdominal discomfort typically occur during dose escalation phases and often diminish over time as the body adapts to the medication. These effects result from the medication's action on gastric emptying and gastrointestinal motility. Starting at low doses and gradually increasing helps minimise these symptoms, though some individuals may require dose reduction or discontinuation if side effects prove intolerable.
Persistent vomiting or diarrhoea can lead to dehydration and potentially acute kidney injury. Patients should maintain adequate fluid intake and seek urgent medical attention if experiencing reduced urine output, severe thirst, or symptoms of dehydration. People with diabetes using these medications should be aware of potential diabetic retinopathy complications, particularly if blood glucose levels improve rapidly; regular eye examinations are recommended, and any visual changes should be reported promptly.
More serious adverse effects requiring immediate medical attention include acute pancreatitis, presenting with severe, persistent abdominal pain that may radiate to the back. Gallbladder problems, including cholelithiasis and cholecystitis, occur more frequently in individuals losing weight rapidly. Symptoms include right upper quadrant pain, particularly after fatty meals. Hypoglycaemia risk increases when these injections are used alongside other glucose-lowering medications, particularly insulin or sulphonylureas, necessitating dose adjustments of concurrent diabetes treatments.
Patients should call 999 or attend A&E immediately for severe allergic reactions (difficulty breathing, severe rash, swelling of face/throat), severe persistent abdominal pain, or symptoms of severe dehydration. For less urgent concerns such as injection site reactions, mild gastrointestinal symptoms, or general questions about side effects, patients should contact their healthcare provider during normal hours. Regular follow-up appointments allow healthcare providers to monitor efficacy, tolerability, and the emergence of any concerning symptoms requiring intervention.
Getting Weekly Weight Loss Injections Through the NHS
Access to weekly weight loss injections through the NHS follows specific pathways determined by NICE guidance and local commissioning decisions. According to NICE Technology Appraisal 875, semaglutide for weight management should be initiated within specialist weight management services (tier 3) with multidisciplinary team support. Patients cannot self-refer for these treatments; instead, they must be assessed by their GP who may refer eligible individuals to these specialist services. The NHS prioritises those with highest clinical need, meaning individuals with significant obesity-related health complications who have attempted other weight loss methods without sustained success.
NHS-funded treatment with semaglutide for weight management is typically limited to a maximum of 2 years, as specified in NICE guidance. Continuation depends on achieving specified weight loss targets, with treatment reviewed after 12 weeks at the maintenance dose. For liraglutide (Saxenda), NICE Technology Appraisal 664 specifies that treatment should only continue beyond 12 weeks if the patient has lost at least 5% of their initial body weight since starting treatment.
Baseline investigations before starting treatment include blood tests to assess renal function, thyroid function, glucose metabolism (HbA1c), and lipid profiles. For people with diabetes, retinopathy screening is recommended, and women of childbearing potential may require pregnancy testing. Ongoing monitoring continues throughout treatment, with frequency determined by individual risk factors and local protocols.
Patients receive education on proper injection technique, storage requirements, and recognition of adverse effects. Due to current NHS capacity constraints and supply issues, many eligible patients face waiting lists or may be advised to pursue lifestyle interventions through tier 2 services initially. Those unable to access NHS provision may consider private healthcare options, though they should ensure prescribers are appropriately qualified and registered with the General Medical Council, and that ongoing medical supervision is included in any private treatment package.
Scientific References
- Semaglutide for managing overweight and obesity.
- Wegovy 0.25 mg, FlexTouch solution for injection in pre-filled pen - Summary of Product Characteristics.
- BMI: preventing ill health and premature death in Black, Asian and other minority ethnic groups.
- GLP-1 medicines for weight loss and diabetes: what you need to know.
- Once-Weekly Semaglutide in Adults with Overweight or Obesity.
Frequently Asked Questions
How much weight can you lose with weekly injections?
Clinical trials show that semaglutide (Wegovy) can lead to significant weight reduction when combined with lifestyle changes, though individual results vary considerably based on adherence, baseline characteristics, and concurrent dietary and physical activity modifications. Treatment effectiveness is monitored regularly, with continuation dependent on achieving specified weight loss targets at 12 weeks.
Can I get weekly weight loss injections on the NHS?
NHS access to semaglutide for weight management requires GP referral to specialist weight management services (tier 3) for eligible patients meeting NICE criteria, including specific BMI thresholds and weight-related comorbidities. Treatment is typically limited to 2 years, though current supply constraints and capacity issues may result in waiting lists.
Are weekly weight loss injections safe?
Weekly weight loss injections are MHRA-approved medications with established safety profiles when used under medical supervision, though they carry risks including gastrointestinal side effects, pancreatitis, and gallbladder problems. Comprehensive assessment, ongoing monitoring, and adherence to prescribing guidelines help minimise risks, and patients should only obtain these medications through legitimate healthcare channels.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












