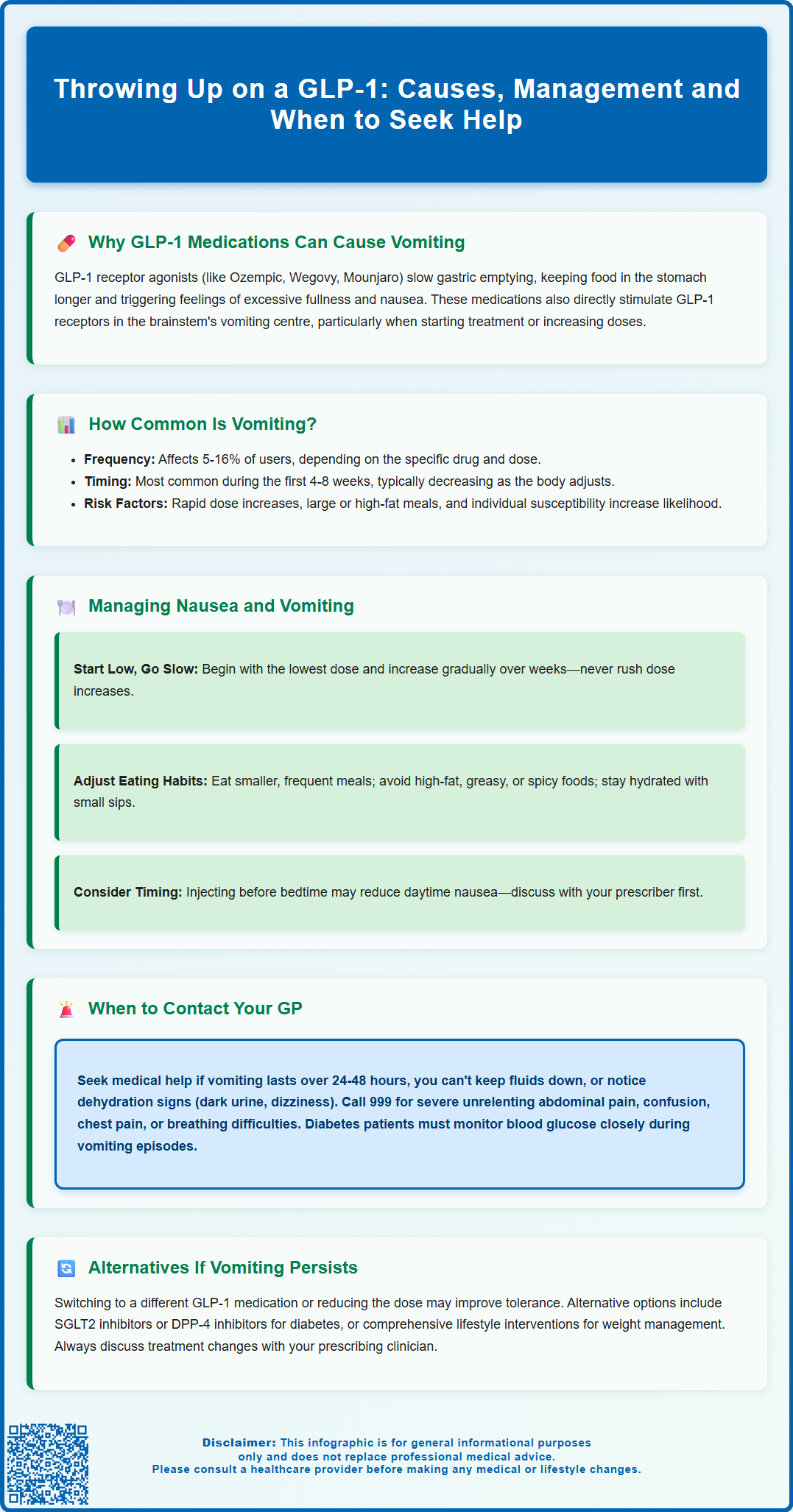
Throwing up on a GLP-1 medication is a recognised side effect that affects a notable proportion of patients using these treatments for type 2 diabetes or weight management. GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), and tirzepatide (Mounjaro) work by slowing gastric emptying and activating receptors in the brainstem, which can trigger nausea and vomiting. Whilst these symptoms are most common during initial treatment or dose increases, they often improve over time. Understanding why vomiting occurs, how to manage it effectively, and when to seek medical advice can help patients continue treatment safely and comfortably.
Summary: Vomiting on GLP-1 medications occurs because these drugs slow gastric emptying and stimulate receptors in the brainstem that trigger the vomiting reflex.
- GLP-1 receptor agonists include semaglutide, liraglutide, dulaglutide, and tirzepatide, used for type 2 diabetes and weight management.
- Vomiting affects approximately 5–16% of patients depending on the specific medication and dose, most commonly during initial treatment or dose escalation.
- Gradual dose titration, smaller meals, avoiding high-fat foods, and staying upright after eating can reduce nausea and vomiting.
- Contact your GP if vomiting persists beyond 24–48 hours, you cannot keep fluids down, or you develop signs of dehydration or severe abdominal pain.
- Switching to a different GLP-1 medication, reducing the dose, or considering alternative drug classes may be appropriate if symptoms remain intolerable.
Table of Contents
Why GLP-1 Medications Can Cause Vomiting
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications increasingly prescribed for type 2 diabetes management and, more recently, for weight management in adults with obesity. These medicines include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and tirzepatide (Mounjaro), which is a dual GIP/GLP-1 receptor agonist. Whilst highly effective, gastrointestinal side effects—particularly nausea and vomiting—are amongst the most commonly reported adverse reactions.
The mechanism behind these side effects relates directly to how these medications work. They mimic the action of naturally occurring GLP-1, a hormone released by the intestine in response to food intake. By activating GLP-1 receptors in multiple locations throughout the body, these drugs slow gastric emptying (the rate at which food leaves the stomach), enhance feelings of satiety, and reduce appetite. This delayed gastric emptying means food remains in the stomach for longer periods, which can trigger sensations of fullness, nausea, and in some cases, vomiting.
Additionally, GLP-1 receptors are present in the brainstem area postrema—a region involved in the vomiting reflex. Direct stimulation of these receptors may contribute to nausea and emesis, particularly during the initial weeks of treatment or following dose escalation. The gastrointestinal effects are generally dose-dependent, meaning higher doses are associated with increased likelihood and severity of symptoms. Understanding this pharmacological basis helps both patients and healthcare professionals anticipate and manage these side effects more effectively, rather than viewing them as unexpected complications.
How Common Is Vomiting on GLP-1 Treatment?
Nausea is the most frequently reported gastrointestinal side effect of GLP-1 receptor agonists, with vomiting occurring less commonly but still affecting a significant proportion of users. The incidence varies considerably between different medications and doses:
-
Semaglutide (Ozempic): Vomiting occurs in approximately 5-10% of patients at diabetes doses
-
Semaglutide (Wegovy): At the higher weight management dose (2.4mg), vomiting affects up to 16% of patients
-
Liraglutide (Victoza): Vomiting affects approximately 5% of patients
-
Liraglutide (Saxenda): At weight management doses, vomiting occurs in about 7-10% of patients
-
Dulaglutide (Trulicity): Vomiting affects approximately 7-9% of patients
-
Tirzepatide (Mounjaro): Vomiting occurs in approximately 5-10% of patients, varying by dose
These side effects are most pronounced during the initial treatment phase, particularly in the first 4–8 weeks, and often diminish as the body adapts to the medication. Clinical trial data demonstrates that most patients who experience nausea or vomiting find these symptoms are transient and mild to moderate in severity. However, a small percentage of patients discontinue treatment specifically due to persistent or severe gastrointestinal side effects.
Key factors influencing vomiting risk include:
-
Dose escalation speed – rapid increases in dose are associated with higher symptom rates
-
Individual susceptibility – some patients are inherently more prone to gastrointestinal side effects
-
Concurrent medications – other drugs affecting gastric motility may compound effects
-
Dietary habits – large, high-fat meals can exacerbate symptoms
It is important to note that whilst mild, occasional vomiting can be an expected side effect, severe or persistent vomiting is not normal and may indicate complications requiring medical assessment. The MHRA and EMA continuously monitor the safety of these medications, and patients are encouraged to report suspected side effects via the MHRA Yellow Card scheme.
Managing Nausea and Vomiting While Taking GLP-1s
Effective management of nausea and vomiting can significantly improve treatment tolerance and adherence to GLP-1 therapy. The cornerstone of management involves both pharmacological strategies and practical lifestyle modifications that work synergistically to minimise gastrointestinal disturbance.
Dose titration represents the most important preventative strategy. NICE guidance and manufacturer recommendations emphasise gradual dose escalation, typically starting at the lowest available dose and increasing slowly over several weeks or months. This approach allows the gastrointestinal system to adapt progressively to the medication's effects. Patients should never increase their dose more rapidly than prescribed, even if they feel they are tolerating the current dose well. If symptoms are severe, your prescriber may recommend stepping back to a previously tolerated dose or extending the time between dose increases.
Dietary modifications can substantially reduce symptoms:
-
Consume smaller, more frequent meals rather than large portions
-
Avoid high-fat, greasy, or heavily spiced foods that delay gastric emptying further
-
Eat slowly and chew food thoroughly
-
Stay well-hydrated, taking small sips of water throughout the day
-
Avoid lying down immediately after eating (remain upright for 2–3 hours post-meal)
-
Identify and avoid personal trigger foods that worsen nausea
Timing of medication administration may also help. Some patients find that injecting their GLP-1 medication before bedtime reduces daytime nausea, though this approach should be discussed with your prescriber first. Weekly GLP-1 medications can be administered at any time of day according to product information.
If symptoms persist despite these measures, your GP may consider prescribing anti-emetic medications for short-term use. Options include:
-
Metoclopramide: May help with delayed gastric emptying but should only be used for short courses (maximum 5 days) due to risk of neurological side effects
-
Prochlorperazine: Can be effective for nausea and vomiting
-
Cyclizine: An alternative that works through a different mechanism
-
Ondansetron: Sometimes used but may cause constipation
-
Domperidone: Used cautiously due to risk of heart rhythm problems (QT prolongation), particularly in older adults, those with heart conditions, or those taking other medications affecting heart rhythm
For people with diabetes, it's important to follow sick-day rules if experiencing vomiting. Monitor blood glucose levels more frequently, check ketones if advised by your healthcare team, and consider temporarily adjusting other diabetes medications (particularly insulin, metformin or SGLT2 inhibitors) after seeking clinical advice if you're unable to eat or drink normally.
When to Contact Your GP About GLP-1 Side Effects
Whilst mild to moderate nausea and occasional vomiting are expected side effects that often improve with time, certain symptoms warrant prompt medical attention. Patients should be aware of warning signs that indicate potentially serious complications or the need for treatment adjustment.
Contact your GP or healthcare professional if you experience:
-
Persistent vomiting lasting more than 24–48 hours, particularly if you cannot keep down fluids
-
Signs of dehydration including dark urine, dizziness, dry mouth, reduced urination, or feeling faint when standing
-
Abdominal pain, especially if severe, constant or located in the upper abdomen radiating to the back
-
Visual changes in vomit, such as blood (appearing red or resembling coffee grounds)
-
Inability to take other essential medications due to vomiting
-
Significant weight loss beyond expected therapeutic effects
-
Symptoms of gallbladder disease including pain in the upper right abdomen, fever, or yellowing of the skin/eyes
-
Symptoms of bowel obstruction such as abdominal distension, inability to pass stool or gas
If your GP is unavailable, contact NHS 111 for advice.
Seek immediate medical attention (call 999 or attend A&E) if you develop:
-
Severe, unrelenting abdominal pain
-
Signs of severe dehydration with confusion or altered consciousness
-
Persistent vomiting with inability to retain any fluids for more than 24 hours
-
Chest pain or difficulty breathing alongside gastrointestinal symptoms
For patients with diabetes taking GLP-1 medications, persistent vomiting poses additional risks. Inability to eat normally whilst taking other diabetes medications (particularly insulin or sulphonylureas) can lead to hypoglycaemia. Conversely, if you're unable to take your GLP-1 medication due to illness, blood glucose levels may rise. Regular blood glucose monitoring becomes particularly important during periods of gastrointestinal upset, and you should contact your diabetes care team for guidance on medication adjustment during illness. If you use insulin or SGLT2 inhibitors, you may need to check ketones when unwell.
Prolonged vomiting can also lead to dehydration and potentially acute kidney injury, which may require assessment with blood tests. Always report suspected side effects to your healthcare professional and consider using the MHRA Yellow Card scheme to report adverse reactions.
Alternatives If Vomiting Persists on GLP-1 Therapy
When vomiting remains problematic despite dose adjustment and supportive measures, several alternative approaches merit consideration. The decision to modify or discontinue GLP-1 therapy should always be made in consultation with your prescribing clinician, weighing the therapeutic benefits against the impact of side effects on quality of life.
Switching to a different GLP-1 medication represents a reasonable first-line strategy. Individual tolerance varies considerably between different agents in this class. For example, patients who experience significant side effects with once-weekly semaglutide might tolerate once-daily liraglutide better, or vice versa. The pharmacokinetic profiles differ between medications, and some patients find certain formulations easier to tolerate than others. Tirzepatide, a dual GIP/GLP-1 receptor agonist, has a slightly different receptor activity profile and may be tolerated differently, though gastrointestinal side effects remain common.
Dose reduction offers another option. Some patients achieve acceptable glycaemic control or weight management benefits at lower doses that produce fewer side effects. Whilst this may result in less robust therapeutic effects, a tolerable lower dose that patients can maintain long-term often proves more beneficial than a higher dose that leads to discontinuation.
Alternative medication classes should be considered if GLP-1 therapy proves intolerable:
-
SGLT2 inhibitors (such as dapagliflozin, empagliflozin) for type 2 diabetes, which work via a completely different mechanism and rarely cause gastrointestinal side effects
-
DPP-4 inhibitors (such as sitagliptin, linagliptin), which enhance endogenous GLP-1 activity more gently
-
Metformin remains first-line for type 2 diabetes, though it can also cause gastrointestinal side effects
-
Orlistat for weight management, though this also has gastrointestinal side effects of a different nature
For weight management specifically, NICE recommends a comprehensive approach including dietary modification, increased physical activity, and behavioural interventions, with or without pharmacotherapy. In the UK, GLP-1 medications for weight management (such as Wegovy) are typically initiated within specialist weight management services according to NICE criteria. For eligible patients with severe obesity, bariatric surgery may be considered as per NICE guidelines. The decision-making process should be individualised, considering your specific clinical circumstances, treatment goals, and personal preferences regarding the balance between therapeutic benefit and side effect burden.
Frequently Asked Questions
How long does vomiting last when starting a GLP-1 medication?
Vomiting and nausea are most common during the first 4–8 weeks of GLP-1 treatment and typically diminish as your body adapts to the medication. Symptoms often improve with gradual dose escalation and dietary modifications.
Can I take anti-sickness medication with my GLP-1 injection?
Yes, your GP may prescribe short-term anti-emetic medications such as metoclopramide, prochlorperazine, or cyclizine if nausea and vomiting persist despite lifestyle measures. Always discuss this with your healthcare professional before starting any new medication.
Should I stop my GLP-1 medication if I keep vomiting?
Do not stop your GLP-1 medication without consulting your prescriber. If vomiting persists for more than 24–48 hours or you cannot keep fluids down, contact your GP urgently for advice on whether to temporarily pause treatment and how to manage your symptoms safely.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript