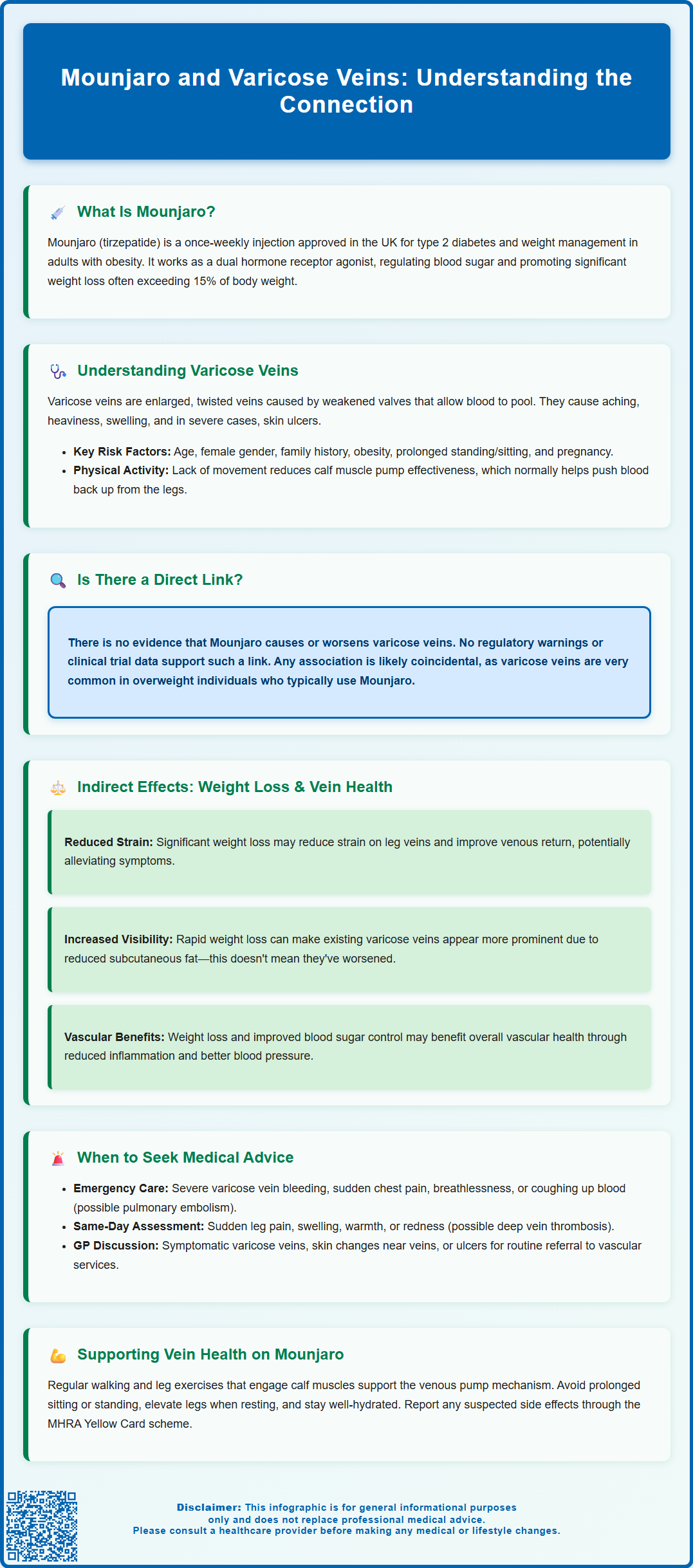
Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management. As its use increases, patients may wonder about potential effects on vein health, particularly varicose veins. Current evidence shows no direct link between Mounjaro and varicose vein development. However, understanding how weight loss and metabolic changes may indirectly influence venous health is important. This article examines the relationship between Mounjaro and varicose veins, explores relevant risk factors, and provides guidance on when to seek medical advice for leg vein concerns whilst using this medication.
Summary: There is no evidence that Mounjaro (tirzepatide) causes or worsens varicose veins.
- Tirzepatide is a dual GIP/GLP-1 receptor agonist used for type 2 diabetes and weight management in the UK.
- Varicose veins are not listed as an adverse reaction in UK regulatory documentation or clinical trial data.
- Weight loss from Mounjaro may reduce venous strain but can make existing varicose veins more visible due to reduced subcutaneous fat.
- Patients should seek urgent medical assessment for sudden leg pain, swelling, or warmth suggesting deep vein thrombosis.
- NICE recommends referral to vascular services for symptomatic varicose veins, skin changes, or venous ulcers.
Table of Contents
- Understanding Mounjaro (Tirzepatide) and Its Primary Uses
- What Are Varicose Veins and Their Common Causes
- Is There a Direct Link Between Mounjaro and Varicose Veins?
- Potential Indirect Effects: Weight Loss, Circulation, and Vein Health
- When to Seek Medical Advice: Monitoring Vein Health on Mounjaro
- Frequently Asked Questions
Understanding Mounjaro (Tirzepatide) and Its Primary Uses
Mounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. It is used as an adjunct to a reduced-calorie diet and increased physical activity. Tirzepatide belongs to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. By mimicking the action of these naturally occurring incretin hormones, tirzepatide helps regulate blood glucose levels, reduce appetite, and promote satiety.
The mechanism of action involves stimulating insulin secretion in a glucose-dependent manner, suppressing glucagon release, slowing gastric emptying, and acting on appetite centres in the brain. These combined effects lead to improved glycaemic control in people with type 2 diabetes and significant weight reduction in those using it for obesity management. Clinical trials have demonstrated that tirzepatide can result in substantial weight loss—often exceeding 15% of baseline body weight—alongside improvements in cardiovascular risk factors such as blood pressure and lipid profiles.
Mounjaro is administered as a once-weekly subcutaneous injection , with doses gradually increased over time to minimise gastrointestinal side effects. Common adverse effects include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort, which typically diminish over time. Important safety considerations include the risk of pancreatitis (seek medical attention for severe abdominal pain), gallbladder disease, dehydration and potential acute kidney injury from persistent vomiting or diarrhoea, and increased hypoglycaemia risk when used with insulin or sulfonylureas. Tirzepatide should be avoided during pregnancy and breastfeeding.
The National Institute for Health and Care Excellence (NICE) recommends tirzepatide for specific patient populations meeting eligibility criteria, with treatment typically initiated and monitored within specialist weight management services for obesity management. As with any medication, prescribing decisions should be individualised, taking into account patient history, comorbidities, and treatment goals.
What Are Varicose Veins and Their Common Causes
Varicose veins are enlarged, twisted, and often visibly bulging veins that most commonly affect the legs and feet. They occur when the valves within veins become weakened or damaged, leading to inefficient blood flow and pooling of blood in the superficial venous system. This venous insufficiency causes the veins to stretch and become tortuous, resulting in the characteristic appearance of varicose veins. While often considered a cosmetic concern, varicose veins can cause symptoms such as aching, heaviness, swelling, itching, and in severe cases, skin changes or ulceration.
Several risk factors contribute to the development of varicose veins. Age is a significant factor, as vein walls and valves naturally weaken over time. Gender also plays a role, with women being more susceptible due to hormonal influences during pregnancy, menstruation, and menopause—hormones such as progesterone can relax vein walls. Family history is another important determinant, suggesting a genetic predisposition. Obesity increases intra-abdominal pressure and places additional strain on leg veins, impairing venous return. Prolonged standing or sitting, particularly in occupations requiring long periods of immobility, can hinder circulation and contribute to venous insufficiency.
Other contributing factors include pregnancy, which increases blood volume and venous pressure, and previous deep vein thrombosis (DVT) or leg injuries that may damage venous valves. Lifestyle factors such as lack of physical activity and poor muscle tone in the legs can also reduce the efficiency of the calf muscle pump, which normally assists venous return. Understanding these risk factors is essential for both prevention and management.
According to NICE guidance, patients with symptomatic varicose veins, skin changes from chronic venous insufficiency, superficial vein thrombosis with suspected venous incompetence, or venous leg ulcers (active or healed) should be referred to a vascular service for assessment. Compression stockings are primarily recommended for symptom relief when interventional treatments are unsuitable, rather than as first-line definitive treatment.
Is There a Direct Link Between Mounjaro and Varicose Veins?
As of 2024, there is no evidence of a causal association between Mounjaro (tirzepatide) and the development or worsening of varicose veins. Varicose veins are not listed as an adverse reaction in the UK Summary of Product Characteristics (SmPC), and there are no Medicines and Healthcare products Regulatory Agency (MHRA) or European Medicines Agency (EMA) safety alerts suggesting such a link. The clinical trial data and post-marketing surveillance reports have not identified venous insufficiency or varicose vein formation as a recognised adverse effect of tirzepatide. Therefore, patients and healthcare professionals should be reassured that current evidence does not suggest varicose veins are a pharmacological consequence of this medication.
It is important to distinguish between direct pharmacological effects and coincidental associations. Varicose veins are extremely common in the general population, particularly among individuals who are overweight or obese—the very population for whom Mounjaro is often prescribed. Consequently, some patients may notice or develop varicose veins while taking tirzepatide, but this is more likely attributable to pre-existing risk factors rather than the medication itself. The temporal association does not imply causation, and careful clinical assessment is needed to evaluate individual circumstances.
That said, any new or worsening symptoms should always be discussed with a healthcare professional. If a patient on Mounjaro notices changes in their leg veins, experiences discomfort, or has concerns about venous health, a thorough evaluation is warranted. This may include a clinical examination, duplex ultrasound assessment, and consideration of other contributing factors. While current evidence does not suggest tirzepatide causes varicose veins, understanding the broader context of a patient's health, weight changes, and lifestyle is essential for comprehensive care and appropriate management of venous conditions.
Potential Indirect Effects: Weight Loss, Circulation, and Vein Health
Although current evidence does not suggest Mounjaro directly affects varicose veins, its significant weight loss effects may have indirect implications for venous health—both positive and, in some cases, potentially complex. Obesity is a well-established risk factor for varicose veins due to increased intra-abdominal pressure, reduced venous return, and chronic strain on the venous system. Therefore, substantial weight reduction achieved with tirzepatide may theoretically reduce the burden on leg veins, improve venous return, and potentially alleviate symptoms associated with venous insufficiency. Some patients report improvements in leg heaviness, swelling, and discomfort as they lose weight, which may reflect better circulatory function, though this evidence is largely anecdotal.
However, rapid or significant weight loss can also lead to changes in tissue composition, skin elasticity, and subcutaneous fat distribution. In some individuals, loss of subcutaneous fat may make pre-existing varicose veins more visible or prominent, even if the underlying venous insufficiency has not worsened. This can be disconcerting for patients who may perceive their veins as having deteriorated, when in fact they are simply more apparent due to reduced overlying tissue. It is important for healthcare professionals to explain this phenomenon and reassure patients that increased visibility does not necessarily equate to disease progression.
Additionally, improved metabolic health associated with weight loss and better glycaemic control may have favourable effects on vascular function more broadly. Reduced inflammation, improved endothelial function, and better blood pressure control can all contribute to healthier circulation. Patients are encouraged to maintain regular physical activity, particularly exercises that engage the calf muscles (such as walking or cycling), as this supports the venous pump mechanism and promotes efficient blood return from the legs.
Lifestyle measures are important for managing varicose veins. Compression stockings can provide symptom relief, particularly when interventional treatments are unsuitable, but are not generally considered definitive treatment according to NICE guidance. Leg elevation and avoiding prolonged immobility remain important self-care recommendations for managing or preventing varicose veins, regardless of medication use.
When to Seek Medical Advice: Monitoring Vein Health on Mounjaro
Patients taking Mounjaro should be vigilant about any new or worsening symptoms related to their legs and veins, and should know when to seek medical advice. While varicose veins themselves are not typically an emergency, certain warning signs warrant prompt evaluation.
Emergency situations requiring immediate attention (call 999 or go to A&E):
-
Severe bleeding from a varicose vein (apply direct pressure and elevate the leg while seeking help)
-
Sudden chest pain, breathlessness, or coughing up blood (possible pulmonary embolism)
Urgent assessment needed (same-day GP or urgent care):
- Sudden onset of leg pain, swelling, warmth, or redness, which could indicate deep vein thrombosis (DVT)
Routine referral to vascular services (discuss with GP):
-
Symptomatic varicose veins causing pain, aching, discomfort, swelling, or itching
-
Skin changes near varicose veins (discolouration, thickening, eczema-like rashes)
-
Development of ulcers near varicose veins
-
Superficial vein thrombosis with suspected venous incompetence
-
Active or healed venous leg ulcer
Routine monitoring of vein health is advisable, particularly for patients with pre-existing varicose veins or risk factors for venous insufficiency. During follow-up appointments for diabetes or weight management, patients should mention any leg symptoms, changes in vein appearance, or concerns about circulation. Healthcare professionals can perform a clinical examination and, if necessary, arrange a duplex ultrasound scan to assess venous function and rule out significant venous reflux or thrombosis. Early detection and management of venous insufficiency can prevent complications and improve quality of life.
Patients should also be encouraged to adopt lifestyle measures that support venous health. These include:
-
Maintaining regular physical activity, especially walking and leg exercises
-
Avoiding prolonged standing or sitting—taking breaks to move and stretch
-
Elevating the legs when resting to facilitate venous return
-
Wearing compression stockings if recommended by a healthcare professional for symptom relief
-
Staying well-hydrated and maintaining a balanced diet to support overall vascular health
If symptoms are bothersome or progressive, referral to a vascular specialist may be appropriate for further assessment and consideration of treatment options. According to NICE guidance, the recommended treatment sequence is: endothermal ablation first if suitable; if unsuitable, ultrasound-guided foam sclerotherapy; if unsuitable, surgery. Open communication between patients and healthcare providers is essential to ensure comprehensive, individualised care while using Mounjaro.
If you suspect any adverse effects from Mounjaro, report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Can Mounjaro cause varicose veins?
No, there is no evidence that Mounjaro (tirzepatide) causes varicose veins. Varicose veins are not listed as an adverse reaction in UK regulatory documentation, and clinical trials have not identified any causal link between tirzepatide and venous insufficiency.
Why might varicose veins become more visible whilst taking Mounjaro?
Significant weight loss from Mounjaro can reduce subcutaneous fat, making pre-existing varicose veins more visible even though the underlying venous condition has not worsened. This is a cosmetic change rather than disease progression.
When should I see a doctor about leg vein symptoms whilst on Mounjaro?
Seek urgent medical assessment for sudden leg pain, swelling, warmth, or redness (possible DVT). Arrange routine GP review for symptomatic varicose veins causing discomfort, skin changes near veins, or development of ulcers, as NICE recommends referral to vascular services for assessment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript