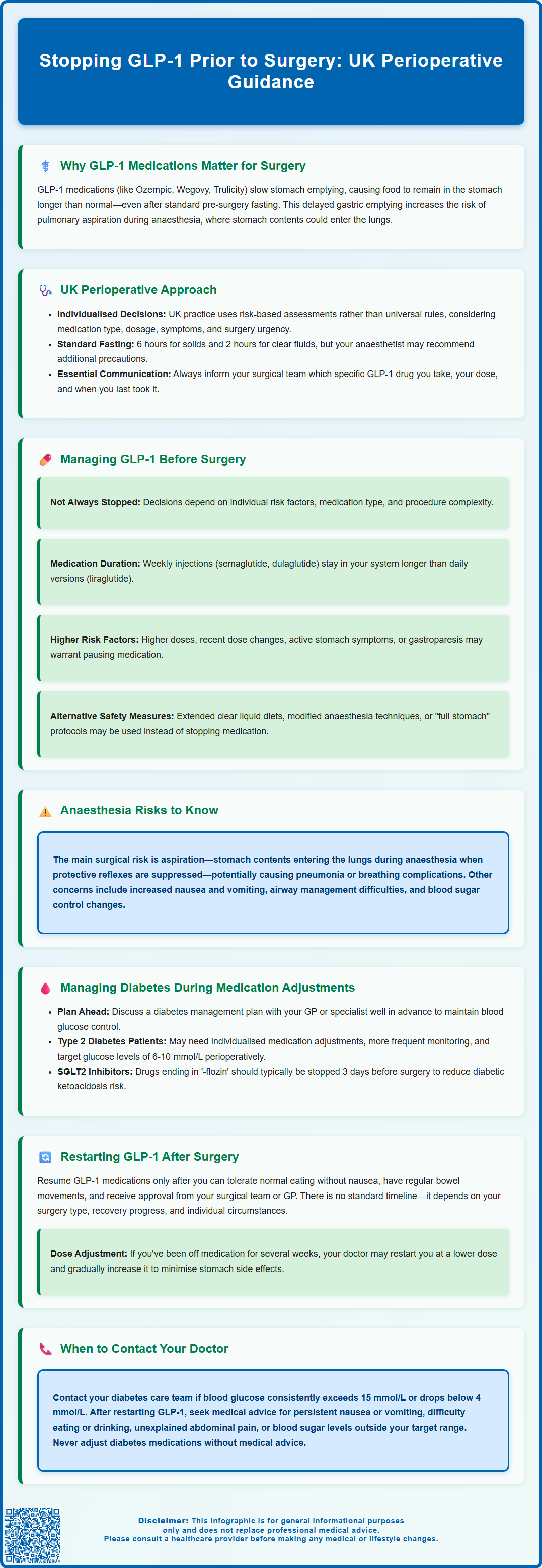
Glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide, dulaglutide, and liraglutide are increasingly prescribed for type 2 diabetes and weight management across the UK. When stopping GLP-1 prior to surgery, careful consideration is needed due to these medications' effect on gastric emptying, which may increase aspiration risk during anaesthesia. Current UK practice involves individualised risk assessment rather than universal cessation protocols. Your anaesthetist and surgical team will evaluate factors including medication type, dosage, gastrointestinal symptoms, and procedure complexity to determine the safest perioperative approach. Always inform your healthcare team about GLP-1 use during pre-operative assessment to ensure appropriate planning and maintain glycaemic control throughout your surgical journey.
Summary: GLP-1 medications may be temporarily paused before surgery based on individualised risk assessment, as they delay gastric emptying and potentially increase aspiration risk during anaesthesia.
- GLP-1 receptor agonists slow gastric emptying, which may cause stomach contents to remain present longer than expected despite appropriate fasting.
- UK practice involves risk-based assessment considering medication type, dosage, gastrointestinal symptoms, procedure complexity, and individual patient factors rather than universal cessation.
- The main perioperative concern is pulmonary aspiration during general anaesthesia when protective airway reflexes are suppressed.
- Patients with type 2 diabetes require careful planning to maintain glycaemic control if GLP-1 therapy is adjusted, with typical perioperative glucose targets of 6-10 mmol/L.
- Resuming GLP-1 after surgery depends on adequate oral intake, normal bowel function, stable recovery, and medical team approval, with possible dose re-titration after prolonged cessation.
Table of Contents
GLP-1 Medications and Surgery: Perioperative Considerations
Glucagon-like peptide-1 (GLP-1) receptor agonists — including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda) — are widely prescribed for type 2 diabetes and weight management. These medications delay gastric emptying, which may have implications for surgical procedures requiring general anaesthesia or deep sedation.
The mechanism of GLP-1 agonists involves slowing the rate at which food leaves the stomach. While this effect helps control blood glucose and promotes satiety for weight loss, it means that stomach contents may remain present longer than expected, even after following standard fasting guidance before surgery. This creates a potential risk of pulmonary aspiration during anaesthesia, where stomach contents could enter the lungs.
Current UK practice typically involves a risk-based approach to GLP-1 medications before surgery. Decisions about whether to continue or temporarily pause these medications are individualised based on factors such as:
-
The specific GLP-1 medication and dosage
-
Whether you're in a dose-escalation phase
-
Presence of gastrointestinal symptoms
-
Type and urgency of surgery
-
Individual risk factors for aspiration
Standard UK fasting guidance typically recommends 6 hours for solids and 2 hours for clear fluids before surgery. Your anaesthetist may recommend additional precautions or modifications to this guidance if you're taking GLP-1 medications.
Patients should always inform their surgical team and anaesthetist about GLP-1 use, including the specific medication, dose, and timing of the last administration, to ensure appropriate perioperative planning.
Perioperative Management of GLP-1 Medications
The approach to GLP-1 medications before surgery varies based on individual risk assessment and local hospital policies. There is no universal UK requirement to stop these medications before all procedures, and practice continues to evolve.
Factors that may influence perioperative management include:
-
Medication characteristics: Daily GLP-1 medications (liraglutide, oral semaglutide) have shorter durations of action than weekly formulations (injectable semaglutide, dulaglutide, exenatide extended-release)
-
Risk factors: Higher doses, recent dose increases, active gastrointestinal symptoms, or known gastroparesis may increase risk
-
Procedure type: More complex surgeries or those requiring general anaesthesia may warrant different approaches than minor procedures
-
Individual patient factors: BMI, presence of diabetes, and other medical conditions
Some anaesthetists may recommend temporarily pausing GLP-1 therapy before certain procedures, particularly for patients with additional risk factors. When cessation is advised, timeframes often consider the medication's dosing frequency, though specific recommendations vary between hospitals and clinicians.
Mitigation strategies that may be employed include:
-
Extended clear liquid diet before surgery
-
Modified anaesthetic techniques
-
Additional monitoring
-
Treating as a 'full stomach' case with appropriate precautions
It is essential to discuss your specific medication regimen with your surgical team during pre-operative assessment, ideally several weeks before your procedure. Never stop or adjust diabetes medications without medical guidance, as this requires careful planning to maintain glycaemic control whilst ensuring surgical safety.
Potential Risks During Anaesthesia
The main concern with GLP-1 receptor agonists during surgery relates to their effect on gastric emptying. When gastric emptying is delayed, food and liquid may remain in the stomach longer than expected, even when patients have followed nil-by-mouth instructions correctly.
During general anaesthesia, protective airway reflexes are suppressed, and if regurgitation occurs, gastric contents could enter the lungs (aspiration). This can cause chemical pneumonitis, bacterial pneumonia, or airway complications. While the absolute risk of aspiration is uncertain and likely low for most patients, case reports and observational studies have documented instances where unexpected gastric contents were found during intubation in patients taking GLP-1 medications who had appropriately fasted.
Other considerations during the perioperative period may include:
-
Potential for nausea and vomiting
-
Challenges with airway management if emergency intubation is required
-
Effects on post-operative recovery and nutrition
-
Changes in blood glucose control
Anaesthetists may modify their approach based on individual risk assessment, potentially including techniques to reduce aspiration risk or additional monitoring. For emergency or urgent procedures, surgery typically proceeds with appropriate precautions according to local policy.
If you experience any side effects or adverse reactions related to your GLP-1 medication, you or your healthcare professional can report these to the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Managing Your Diabetes When Adjusting GLP-1 Therapy
If your healthcare team recommends temporarily adjusting your GLP-1 medication before surgery, careful planning is needed to maintain adequate blood glucose control, particularly for patients with type 2 diabetes. Your diabetes management plan should be discussed with your GP or diabetes specialist well in advance of surgery.
For patients using GLP-1 agonists primarily for weight management rather than diabetes control, temporary adjustment typically poses less immediate concern regarding blood glucose levels. However, you should still monitor for any unexpected changes.
For those with type 2 diabetes, your healthcare team may recommend several strategies:
-
Individualised medication plan: Specific guidance for each of your diabetes medications (metformin, sulfonylureas, SGLT2 inhibitors, insulin) following established UK protocols
-
Enhanced blood glucose monitoring: More frequent self-monitoring to identify any changes in control
-
Dietary consistency: Maintaining regular eating patterns where possible
-
Clear targets: Typical perioperative blood glucose targets are 6-10 mmol/L (with an acceptable range of 4-12 mmol/L)
SGLT2 inhibitors (medications ending in '-flozin') are typically stopped 3 days before surgery to reduce the risk of diabetic ketoacidosis, according to UK guidance.
On the day of surgery, you will receive specific instructions about diabetes medications based on the Joint British Diabetes Societies (JBDS) and Centre for Perioperative Care (CPOC) guidelines, which vary by medication class and procedure timing.
Patients should contact their diabetes care team if blood glucose levels consistently exceed 15 mmol/L or fall below 4 mmol/L. Never attempt to adjust diabetes medications without medical advice, as this may cause hypoglycaemia or other complications.
When to Resume GLP-1 After Surgery
Resuming GLP-1 therapy after surgery should be guided by your healthcare team based on your recovery progress, ability to tolerate oral intake, and overall post-operative course. There is no standardised timeline, as the appropriate restart point varies based on the type of surgery performed and individual circumstances.
General principles for restarting GLP-1 medications include:
-
Adequate oral intake: You should be tolerating a normal diet (or your usual post-operative diet plan) without significant nausea or vomiting
-
Resolution of post-operative ileus: Normal bowel function should have returned, particularly after abdominal or pelvic surgery
-
Stable clinical condition: Any post-operative complications should be resolved, and you should be recovering as expected
-
Medical team approval: Always confirm with your surgical team or GP before restarting
If you've been off a GLP-1 medication for several weeks, your doctor may recommend re-titrating the dose (starting at a lower dose and gradually increasing) to minimise gastrointestinal side effects when restarting. This is particularly important for higher-dose formulations.
Following major surgery — particularly gastrointestinal, bariatric, or other complex procedures — your surgeon will provide specific guidance on when to resume GLP-1 therapy. Some bariatric procedures may require permanent adjustment of GLP-1 therapy or alternative diabetes management strategies.
Contact your GP or diabetes specialist if you experience:
-
Persistent nausea or vomiting after restarting GLP-1 medication
-
Difficulty maintaining adequate nutrition or hydration
-
Unexplained abdominal pain or bloating
-
Blood glucose levels outside your target range
Your healthcare team will provide individualised guidance based on your specific circumstances, ensuring that resumption of GLP-1 therapy supports both your diabetes management goals and surgical recovery.
Scientific References
Frequently Asked Questions
How long before surgery should I stop taking my GLP-1 medication?
There is no universal UK requirement to stop GLP-1 medications before all procedures. Your anaesthetist will provide individualised guidance based on your specific medication, dosage, procedure type, and risk factors during pre-operative assessment, ideally several weeks before surgery.
Why might GLP-1 medications need to be paused before surgery?
GLP-1 medications delay gastric emptying, meaning stomach contents may remain present longer than expected even after appropriate fasting. This creates a potential risk of pulmonary aspiration during general anaesthesia when protective airway reflexes are suppressed.
When can I restart my GLP-1 medication after surgery?
You can typically resume GLP-1 therapy once you're tolerating a normal diet without nausea or vomiting, normal bowel function has returned, and your surgical team approves. After prolonged cessation, your doctor may recommend re-titrating the dose to minimise gastrointestinal side effects.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












