Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities. Whilst many patients achieve significant weight loss initially, some experience a plateau or reduced effectiveness over time. Understanding why Saxenda may stop working—whether due to metabolic adaptation, lifestyle factors, or medication issues—is essential for optimising treatment outcomes. This article explores the reasons behind reduced efficacy, how to recognise when Saxenda is no longer effective, practical steps to take, and alternative weight management options available through the NHS.
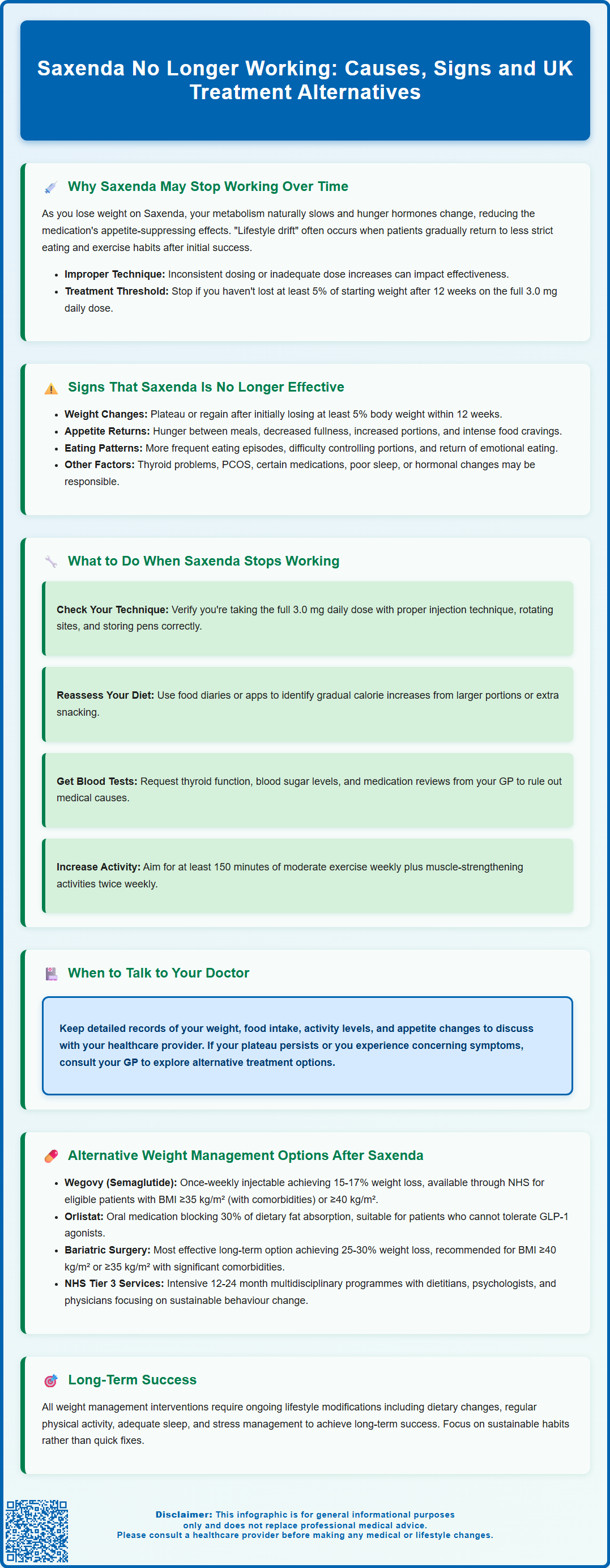
Summary: Saxenda may stop working due to metabolic adaptation, reduced basal metabolic rate with weight loss, lifestyle drift, medication adherence issues, or hormonal changes that increase hunger and reduce satiety.
- Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with comorbidities.
- Treatment should be discontinued if patients have not lost at least 5% of initial body weight after 12 weeks on the full 3.0 mg daily dose.
- Metabolic adaptation, including reduced basal metabolic rate and hormonal changes affecting appetite regulation, can reduce Saxenda's effectiveness over time.
- Signs of reduced efficacy include weight plateau lasting 8–12 weeks, return of appetite, increased portion sizes, and more frequent snacking despite continued treatment.
- Management includes reviewing injection technique and adherence, comprehensive lifestyle reassessment, medical evaluation to exclude underlying causes, and intensifying behavioural support.
- Alternative options include Wegovy (semaglutide), orlistat, specialist NHS weight management services (Tier 3), and bariatric surgery for eligible patients.
Table of Contents
Why Saxenda May Stop Working Over Time
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with a BMI ≥30 kg/m², or ≥27 kg/m² with at least one weight-related comorbidity, as an adjunct to a reduced-calorie diet and increased physical activity. Whilst many patients experience significant weight loss during the initial months of treatment, some report a plateau or reduced effectiveness over time. Understanding why this occurs is essential for managing expectations and optimising treatment outcomes.
Physiological adaptation is one of the primary reasons Saxenda may appear less effective. The body naturally adapts to pharmacological interventions through various compensatory mechanisms. As weight decreases, basal metabolic rate typically declines, meaning fewer calories are required to maintain body weight. Additionally, hormonal changes associated with weight loss—including alterations in leptin, ghrelin, and other appetite-regulating hormones—can increase hunger signals and reduce satiety, partially counteracting Saxenda's appetite-suppressing effects.
Some patients report what appears to be reduced response over time, though the mechanisms are not fully understood and there is limited evidence for true pharmacological tolerance to liraglutide. It is important to note that there is no established link between duration of use and complete loss of efficacy in clinical trials.
Other contributing factors include lifestyle drift, where initial dietary and physical activity modifications become less stringent over time, and medication adherence issues. Patients may unconsciously relax their calorie restriction or exercise routines once initial weight loss goals are achieved. Additionally, improper injection technique, inconsistent dosing, or inadequate dose escalation during the titration phase can all impact treatment effectiveness. Psychological factors, including weight loss fatigue and reduced motivation, may further compound these challenges.
According to the Saxenda SmPC, treatment should be discontinued if patients have not lost at least 5% of their initial body weight after 12 weeks on the full 3.0 mg daily dose.
Signs That Saxenda Is No Longer Effective
Recognising when Saxenda has stopped working effectively is crucial for timely intervention and treatment adjustment. The most obvious indicator is a weight loss plateau or weight regain. According to the MHRA/SmPC guidance, patients should achieve at least 5% weight loss after 12 weeks at the maintenance dose (3.0 mg daily). If weight loss stalls completely for 8–12 weeks despite continued treatment and adherence to lifestyle modifications, this may suggest reduced medication efficacy.
Return of appetite and reduced satiety are key clinical signs. Patients who initially experienced significant appetite suppression may notice a gradual return of hunger between meals, increased portion sizes, or more frequent snacking. The characteristic feeling of fullness that Saxenda provides may diminish, making it harder to maintain calorie restriction. Some patients report that food cravings, particularly for high-calorie or carbohydrate-rich foods, become more intense or frequent.
Changes in eating behaviour patterns can also signal reduced effectiveness. These may include:
-
Increased frequency of eating episodes throughout the day
-
Difficulty adhering to previously manageable portion sizes
-
Return of emotional or stress-related eating patterns
-
Reduced duration of post-meal satiety
It is important to distinguish between true medication failure and other factors affecting weight management. Concurrent medical conditions such as hypothyroidism, polycystic ovary syndrome, or Cushing's syndrome can impair weight loss. Certain medications, including some antidepressants, antipsychotics, corticosteroids, and beta-blockers, may promote weight gain or hinder weight loss efforts. Patients should not stop or change any prescribed medications without consulting their healthcare provider. Additionally, inadequate sleep, chronic stress, and hormonal changes (such as menopause) can all impact weight management independently of Saxenda's pharmacological action.
Patients experiencing these signs should maintain detailed records of their weight, dietary intake, physical activity, and any changes in appetite or eating patterns to discuss with their healthcare provider.
Important safety note: Seek urgent medical attention if you experience severe, persistent abdominal pain (with or without vomiting), signs of gallbladder problems, or persistent vomiting that prevents you from keeping fluids down.
What to Do When Saxenda Stops Working
When Saxenda appears to lose effectiveness, a systematic approach is essential before considering treatment discontinuation or alternatives. The first step is to review adherence and injection technique with your GP or prescribing clinician. Ensure you are consistently administering the full 3.0 mg maintenance dose daily. Verify proper injection technique, including rotating injection sites (abdomen, thigh, or upper arm) to prevent lipohypertrophy, which can impair absorption. Check that pens are stored correctly (refrigerated before first use at 2-8°C; after first use, keep below 30°C or refrigerated; do not freeze; protect from light; discard after one month) and that medication has not expired.
Comprehensive lifestyle reassessment is crucial. Work with a dietitian or weight management specialist to evaluate your current dietary intake honestly. Food diaries or smartphone applications can reveal unintentional calorie creep—gradual increases in portion sizes or snacking that accumulate over time. Consider whether your physical activity levels have declined from the initial treatment phase. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity aerobic activity weekly, combined with muscle-strengthening activities on two or more days, for optimal weight management.
Medical evaluation should exclude underlying causes of weight plateau or regain. Your GP may arrange blood tests to assess:
-
Thyroid function (TSH, free T4)
-
Fasting glucose and HbA1c
-
Lipid profile
-
Appropriate screening tests for Cushing's syndrome if clinically indicated (such as overnight dexamethasone suppression test), which would typically involve endocrinology referral
Review all current medications with your healthcare provider, as some may interfere with weight loss. Discuss any recent life changes, stress factors, or sleep disturbances that might impact weight management.
Behavioural support intensification can reinvigorate weight loss efforts. This may include referral to specialist weight management services, cognitive behavioural therapy for eating behaviours, or structured group support programmes. Some patients benefit from working with a physiotherapist or exercise specialist to develop a more intensive or varied physical activity programme. NHS exercise referral schemes may be available in your area.
If treatment is interrupted for any reason, your clinician will advise on re-titrating the dose when restarting to minimise gastrointestinal side effects. Any decision about continuing or stopping Saxenda should be made in consultation with your healthcare provider, considering your individual circumstances, degree of weight loss achieved, presence of comorbidities, and overall treatment goals.
Alternative Weight Management Options After Saxenda
When Saxenda no longer provides adequate benefit despite optimisation efforts, several alternative pharmacological and non-pharmacological options exist within the UK healthcare system. Treatment decisions should be individualised based on BMI, comorbidities, previous treatment response, and patient preferences.
Alternative GLP-1 receptor agonists represent a logical next step. Wegovy (semaglutide 2.4 mg) is a once-weekly injectable GLP-1 agonist licensed for weight management in the UK. Clinical trials demonstrate superior weight loss compared to liraglutide, with patients achieving average weight reductions of 15–17% of initial body weight. According to NICE Technology Appraisal 875, Wegovy is available through specialist weight management services for adults with a BMI of at least 35 kg/m² (or 32.5 kg/m² for certain ethnic groups) with at least one weight-related condition, or a BMI of at least 40 kg/m² without comorbidities. Treatment is limited to a maximum of two years. NHS availability may be subject to local service constraints. The medication shares a similar adverse effect profile to Saxenda, including nausea, vomiting, diarrhoea, and constipation, though these typically diminish over time.
Orlistat is an alternative mechanism for weight management, available both on NHS prescription and over-the-counter at lower doses. This lipase inhibitor reduces dietary fat absorption by approximately 30%. It typically produces modest additional weight loss compared to lifestyle changes alone. It may suit patients who cannot tolerate GLP-1 agonists or prefer oral medication. Patients must adhere to a reduced-fat diet to minimise gastrointestinal adverse effects, including oily stools, faecal urgency, and flatulence.
Combination therapies are emerging in weight management. Mounjaro (tirzepatide), a dual GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptor agonist, has received MHRA approval for type 2 diabetes and is being evaluated for weight management indications in the UK.
Bariatric surgery remains the most effective long-term intervention for severe obesity. NICE recommends considering surgery for adults with:
-
BMI ≥40 kg/m², or
-
BMI 35–40 kg/m² with significant obesity-related comorbidities (type 2 diabetes, hypertension, sleep apnoea)
-
BMI 30–35 kg/m² with recent-onset type 2 diabetes (particularly if poorly controlled)
-
Who have tried all appropriate non-surgical measures
Procedures include sleeve gastrectomy, Roux-en-Y gastric bypass, and adjustable gastric banding. Patients typically achieve 25–30% total body weight loss with sustained improvement in comorbidities. However, surgery carries procedural risks and requires lifelong dietary modifications and nutritional supplementation.
Specialist weight management services (Tier 3) provide intensive multidisciplinary support, including specialist dietitians, psychologists, physiotherapists, and physicians. These NHS services offer structured programmes typically lasting 12–24 months, focusing on sustainable behaviour change without medication. Referral criteria vary by local NHS services, so check with your GP about local eligibility requirements.
Regardless of the chosen approach, ongoing lifestyle modification remains fundamental. No pharmacological or surgical intervention succeeds without sustained dietary changes, regular physical activity, adequate sleep, and stress management. Patients should maintain regular follow-up with their healthcare team to monitor progress, manage adverse effects, and adjust treatment as needed. If you are considering stopping Saxenda or exploring alternatives, discuss your options thoroughly with your GP or specialist to develop an individualised plan that addresses your specific circumstances and health goals.
If you experience any suspected side effects from weight management medications, report them through the MHRA Yellow Card scheme.
Frequently Asked Questions
How long does Saxenda continue to work effectively?
Saxenda's effectiveness varies individually, but patients should achieve at least 5% weight loss after 12 weeks at the full 3.0 mg dose. Some patients experience reduced effectiveness over time due to metabolic adaptation, though clinical trials show no established link between duration of use and complete loss of efficacy.
What should I do if Saxenda stops working for weight loss?
First, review your injection technique and adherence with your GP, reassess your diet and physical activity levels, and exclude underlying medical causes such as thyroid dysfunction. Your healthcare provider may recommend intensifying lifestyle support, switching to alternative medications like Wegovy, or referring you to specialist weight management services.
Can I switch from Saxenda to Wegovy on the NHS?
Wegovy (semaglutide 2.4 mg) is available through specialist NHS weight management services for eligible patients with BMI ≥35 kg/m² (or ≥32.5 kg/m² for certain ethnic groups) with weight-related comorbidities, or BMI ≥40 kg/m² without comorbidities. Discuss eligibility and local availability with your GP or specialist, as access may vary by region.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










