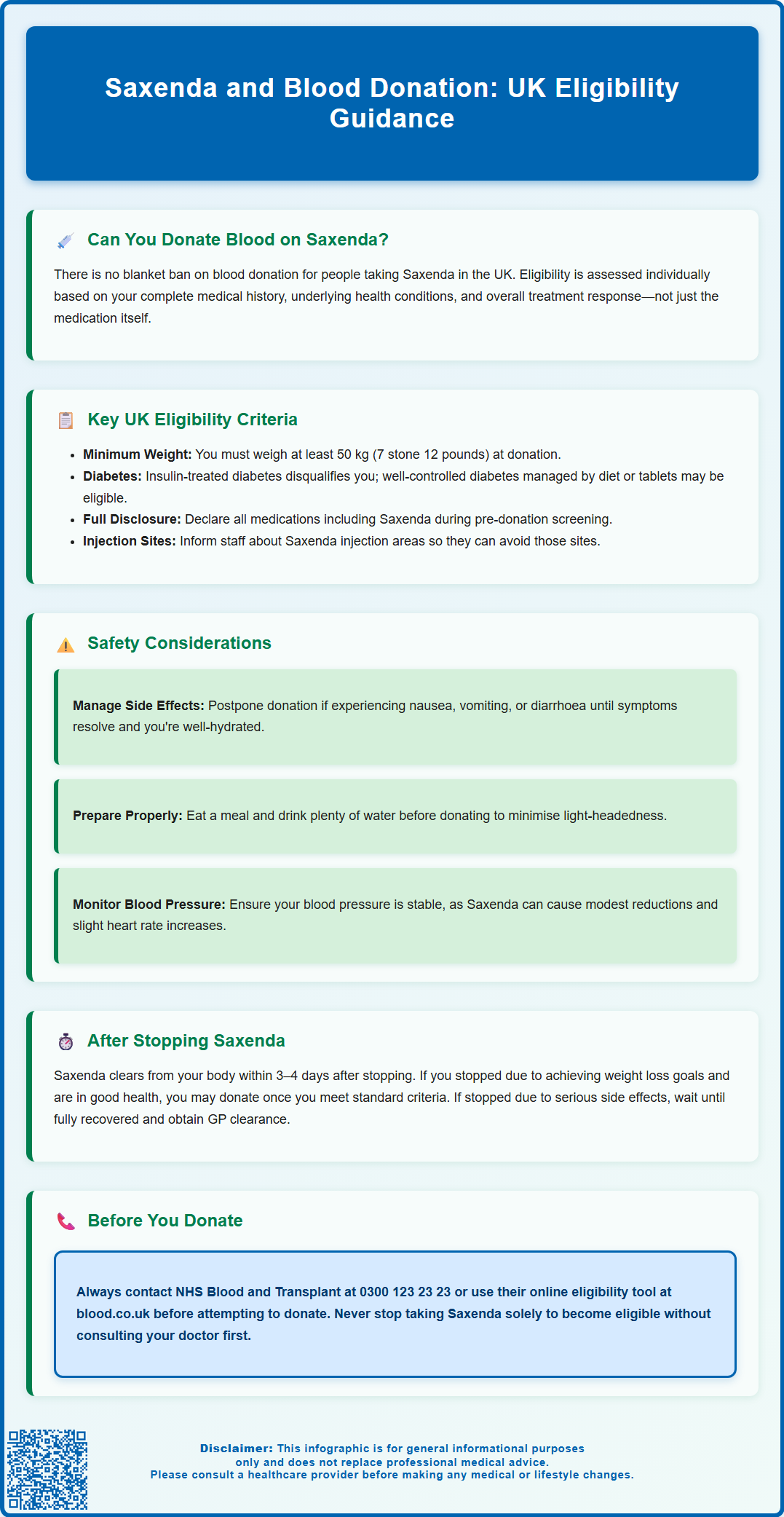
Many patients prescribed Saxenda (liraglutide) for weight management wonder whether they can continue donating blood during treatment. Saxenda is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for obesity management in adults. Currently, there is no blanket prohibition on blood donation for individuals taking Saxenda. NHS Blood and Transplant (NHSBT) assesses each potential donor individually based on complete medical history, overall health status, and whether underlying conditions affect eligibility. Anyone taking Saxenda who wishes to donate should contact NHSBT directly via their helpline (0300 123 23 23) or use the online eligibility checker before attending a donation session.
Summary: There is no blanket prohibition on blood donation for individuals taking Saxenda in the UK, but NHS Blood and Transplant assesses each donor individually based on complete medical history and overall health status.
- Saxenda (liraglutide) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities.
- Blood donation eligibility depends on meeting standard NHSBT criteria including minimum weight of 50 kg, adequate haemoglobin levels, and being in good general health.
- Common gastrointestinal side effects such as nausea and vomiting may cause dehydration, making donation inadvisable until symptoms resolve and hydration is restored.
- Liraglutide has a half-life of approximately 13 hours and is largely eliminated within 3–4 days after discontinuation, though eligibility depends on overall clinical stability.
- Potential donors taking Saxenda should contact NHSBT on 0300 123 23 23 or use the online eligibility checker before attending a donation session.
Table of Contents
Can You Donate Blood While Taking Saxenda?
Saxenda (liraglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Many patients prescribed Saxenda wonder whether they can continue to donate blood whilst receiving treatment. The answer depends on several factors, including the reason for taking the medication, overall health status, and specific guidance from NHS Blood and Transplant (NHSBT).
Currently, there is no blanket prohibition on blood donation for individuals taking Saxenda in the UK. However, blood donation services assess each potential donor individually based on their complete medical history rather than focusing solely on a single medication. The primary considerations include whether the underlying condition being treated affects donation eligibility, and whether the donor meets all other standard criteria for safe blood donation.
The key principle underpinning blood donation eligibility is donor and recipient safety. NHSBT must ensure that donated blood is safe for transfusion and that the donation process does not harm the donor. Whilst Saxenda itself is not typically considered a contraindication to donation, the metabolic conditions it treats may require additional assessment. It's important to note that Saxenda is specifically for weight management, not diabetes (liraglutide for diabetes is marketed as Victoza, with different dosing).
It is important to note that eligibility criteria can change, and individual circumstances vary considerably. Anyone taking Saxenda who wishes to donate blood should contact NHSBT directly via their helpline (0300 123 23 23) or use the 'Check if you can donate' tool on the NHSBT website. Never stop taking prescribed medications solely to become eligible for blood donation without consulting your prescribing clinician.
UK Blood Donation Eligibility Criteria and Saxenda
NHS Blood and Transplant operates comprehensive eligibility criteria designed to protect both blood donors and recipients. These criteria assess numerous factors including recent travel, medical history, current medications, and overall health status. When considering donation whilst taking Saxenda, several standard eligibility requirements become particularly relevant.
General eligibility requirements for blood donation in the UK include:
-
Being aged 17–66 years for first-time donors (existing donors may continue beyond 70 subject to assessment)
-
Weighing at least 50 kg (7 stone 12 pounds)
-
Being in good general health
-
Meeting haemoglobin level requirements (at least 135 g/L for men and 125 g/L for women)
-
Having adequate venous access
For individuals taking Saxenda, the weight criterion is particularly noteworthy. Saxenda is prescribed for weight management, and some patients may be working towards achieving a healthier weight. Donors must meet the minimum weight requirement at the time of donation to ensure their blood volume can safely accommodate the donation without adverse effects.
The underlying medical condition being treated with Saxenda requires consideration. If you have diabetes, eligibility depends on your treatment: those on insulin are generally not eligible to donate, while those with well-controlled diabetes managed by diet or tablets may be eligible if they have no complications. Note that Saxenda is not licensed for diabetes in the UK (Victoza is the liraglutide product for diabetes). If obesity-related comorbidities such as cardiovascular disease are present, these conditions are assessed independently.
Medication disclosure is mandatory during the pre-donation health screening. Donation centre staff use this information alongside clinical guidelines to determine eligibility. Saxenda is administered via subcutaneous injection, and donors should inform staff about injection sites to avoid venepuncture in areas that might be affected by recent injections or local reactions. Standard venepuncture sites typically avoid common Saxenda injection areas.
Safety Considerations for Blood Donors on Liraglutide
Liraglutide's mechanism of action and side effect profile warrant careful consideration in the context of blood donation. As a GLP-1 receptor agonist, liraglutide works by enhancing glucose-dependent insulin secretion, suppressing glucagon release, slowing gastric emptying, and promoting satiety. These physiological effects have implications for the donation process.
Gastrointestinal side effects are common with Saxenda, particularly during dose titration. Nausea, vomiting, diarrhoea, and constipation affect many patients, especially in the initial weeks of treatment. These symptoms can lead to dehydration or electrolyte imbalances, which would make blood donation inadvisable. Potential donors experiencing significant gastrointestinal symptoms should postpone donation until these effects have resolved and they are well-hydrated and feeling well.
Hypoglycaemia risk with GLP-1 agonists like Saxenda is generally low when used alone, but may increase if combined with insulin or sulfonylureas. Blood donation itself can occasionally cause vasovagal reactions, light-headedness, or dizziness. NHSBT advises eating a meal or snack and drinking plenty of water before donation – do not fast. This is particularly important for those on Saxenda to minimise any risk of feeling unwell during or after donation.
Cardiovascular considerations are also relevant. Liraglutide typically causes a small increase in heart rate (average 2–3 beats per minute) and a modest reduction in blood pressure. Whilst these effects are generally well-tolerated, individuals with pre-existing cardiovascular conditions should have these assessed as part of the standard donation eligibility screening. Blood pressure should be stable before donation.
Injection site reactions such as redness, itching, or bruising occur in some patients. Donation staff should be informed of injection sites to select an appropriate venepuncture site that avoids areas of local inflammation or recent injection, ensuring both successful donation and donor comfort.
If you experience any suspected side effects from Saxenda, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
When to Resume Blood Donation After Stopping Saxenda
For individuals who have discontinued Saxenda, questions often arise about when it becomes safe to donate blood. The pharmacokinetic properties of liraglutide provide guidance on appropriate waiting periods, though there is no official specific deferral period mandated by NHSBT solely for liraglutide cessation.
Liraglutide has a half-life of approximately 13 hours following subcutaneous administration. After discontinuation, the medication is largely eliminated from the body within 3–4 days (approximately 5 half-lives). From a purely pharmacological perspective, the drug would not be present in significant concentrations in donated blood after this timeframe. However, the decision to resume donation depends on multiple factors beyond drug clearance, including your overall clinical stability and meeting all NHSBT criteria.
The reason for stopping Saxenda is clinically significant. If treatment was discontinued due to adverse effects, particularly serious ones such as pancreatitis, severe gastrointestinal symptoms, or significant adverse reactions, potential donors should wait until they have fully recovered and been medically cleared. Recovery time varies depending on the nature and severity of the adverse event. After any serious adverse event or hospitalisation, seek GP clearance and confirm eligibility with NHSBT before attempting to donate.
If Saxenda was stopped because treatment goals were achieved (successful weight loss and weight maintenance), and the individual is in good general health, they may be eligible to donate once they meet all standard NHSBT criteria. This includes maintaining adequate weight (≥50 kg), having stable health parameters, and feeling well.
Transition to other weight management strategies should be considered. If individuals have moved to other medications or interventions following Saxenda discontinuation, these new treatments must also be assessed for donation eligibility. Anyone uncertain about their eligibility should contact NHSBT's donor helpline (0300 123 23 23) for personalised advice based on their complete medical history and current health status.
Guidance from NHS Blood and Transplant on Weight-Loss Medications
NHS Blood and Transplant maintains detailed guidance on medication use and blood donation eligibility, though specific policies on newer weight-loss medications like Saxenda continue to evolve as these treatments become more widely prescribed. NHSBT's approach prioritises evidence-based assessment of both donor safety and blood product safety.
The general principle applied to weight-loss medications is that the medication itself may not preclude donation, but the underlying health conditions, treatment response, and overall medical status require comprehensive evaluation. NHSBT provides an online 'Check if you can donate' tool and condition/medicine pages, though not every medication may be specifically listed.
Potential donors taking any medication, including Saxenda, should:
-
Contact NHSBT before attending a donation session if uncertain about eligibility (telephone: 0300 123 23 23)
-
Use the NHSBT 'Check if you can donate' tool on the blood.co.uk website
-
Provide complete medication information during the pre-donation health questionnaire, including drug name, dose, and duration of treatment
-
Disclose the indication for treatment (weight management, diabetes, or other)
-
Report any side effects or complications experienced whilst taking the medication
-
Inform staff of any other medical conditions or medications
NHSBT's medical staff make final eligibility determinations based on current clinical guidelines, scientific evidence, and individual donor assessment. Decisions consider whether the medication or underlying condition might affect blood quality, whether donation could harm the donor, and whether any infectious or safety risks exist.
For the most current guidance, potential donors should consult the NHSBT website (www.blood.co.uk) or contact the donor helpline directly. Policies may be updated as new evidence emerges about GLP-1 receptor agonists and their use in weight management. Donors should never discontinue prescribed medications solely to become eligible for blood donation without consulting their prescribing clinician, as the health benefits of continuing treatment typically outweigh the desire to donate blood.
If you experience any suspected side effects from Saxenda, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Frequently Asked Questions
Can I donate blood if I'm currently taking Saxenda?
There is no blanket prohibition on blood donation whilst taking Saxenda in the UK. NHS Blood and Transplant assesses each potential donor individually based on complete medical history, overall health status, and whether you meet standard eligibility criteria including minimum weight requirements and adequate haemoglobin levels.
How long after stopping Saxenda can I donate blood?
Liraglutide is largely eliminated from the body within 3–4 days after discontinuation. However, eligibility to donate depends on the reason for stopping treatment, your overall clinical stability, and meeting all standard NHSBT criteria rather than a specific waiting period.
Who should I contact to check my blood donation eligibility whilst on Saxenda?
Contact NHS Blood and Transplant directly via their donor helpline on 0300 123 23 23 or use the 'Check if you can donate' tool on the NHSBT website (www.blood.co.uk) before attending a donation session. Never stop prescribed medications solely to become eligible for donation without consulting your prescribing clinician.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript