Protein shakes for lunch whilst taking GLP-1 medications can be a practical nutritional strategy for many patients experiencing reduced appetite. GLP-1 receptor agonists such as semaglutide and liraglutide are increasingly prescribed for type 2 diabetes and obesity management, but their appetite-suppressing effects often make consuming adequate protein challenging. Understanding how to incorporate protein shakes safely and effectively into your diet can help preserve muscle mass during weight loss, manage gastrointestinal side effects, and maintain balanced nutrition. This article explores the evidence, practical considerations, and best practices for using protein shakes as a meal option during GLP-1 therapy.
Summary: Protein shakes can be safely consumed for lunch whilst taking GLP-1 medications and may help meet nutritional needs when appetite is reduced.
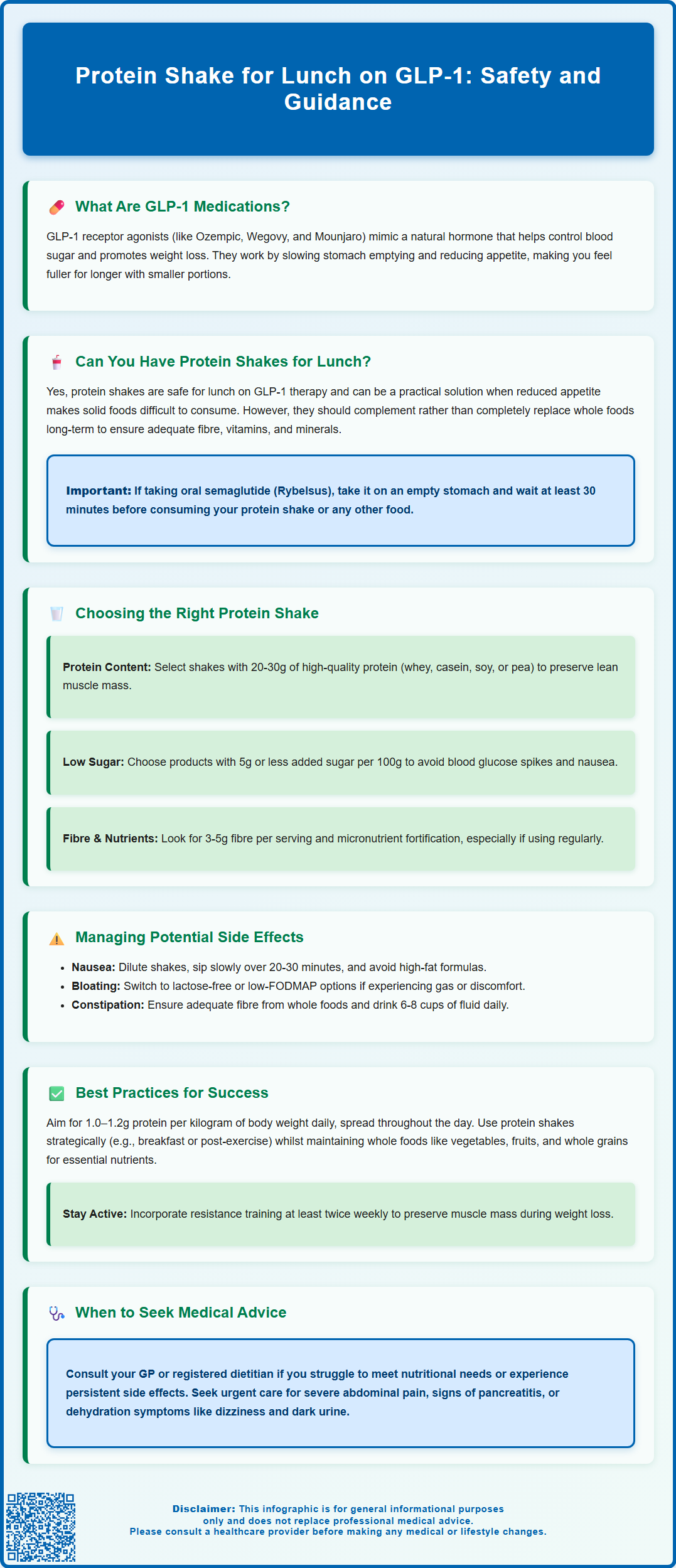
- GLP-1 receptor agonists slow gastric emptying and reduce appetite by acting on brain centres, making adequate protein intake challenging.
- A well-formulated protein shake providing 20–30g of high-quality protein can help preserve muscle mass during GLP-1-induced weight loss.
- Choose shakes low in added sugars and moderate in fat to minimise gastrointestinal side effects such as nausea and bloating.
- Protein shakes should complement, not entirely replace, whole foods to ensure adequate fibre, vitamins, and minerals.
- Discuss protein intake with your healthcare team if you have kidney disease or are taking insulin or sulfonylureas alongside GLP-1 therapy.
Table of Contents
- What Are GLP-1 Medications and How Do They Affect Appetite?
- Can You Have a Protein Shake for Lunch on GLP-1 Treatment?
- Nutritional Considerations for Protein Shakes with GLP-1 Therapy
- Potential Side Effects of Protein Shakes While Taking GLP-1
- Best Practices for Meal Replacement on GLP-1 Medications
- Frequently Asked Questions
What Are GLP-1 Medications and How Do They Affect Appetite?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, obesity. These medicines include semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), and tirzepatide (Mounjaro), though tirzepatide is actually a dual GIP/GLP-1 receptor agonist rather than a GLP-1-only medication. They work by mimicking the action of the naturally occurring GLP-1 hormone, which is released from the intestine in response to food intake.
The mechanism of action involves several pathways that collectively improve glycaemic control and promote weight loss. GLP-1 receptor agonists stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning they only trigger insulin release when blood glucose levels are elevated. This generally reduces the risk of hypoglycaemia compared with some other diabetes medications, though this risk increases when used alongside insulin or sulfonylureas. Simultaneously, these agents suppress glucagon secretion, which further helps to lower blood glucose levels.
One of the most notable effects of GLP-1 medications is their impact on appetite and satiety. They slow gastric emptying, meaning food remains in the stomach for longer, which prolongs the feeling of fullness after eating. Additionally, GLP-1 receptor agonists act on appetite centres in the brain, particularly the hypothalamus, reducing hunger signals and overall food intake. Patients commonly report feeling satisfied with smaller portions and experiencing reduced cravings.
These appetite-suppressing effects are beneficial for weight management but can also present challenges. Many individuals on GLP-1 therapy find it difficult to consume adequate nutrition, particularly protein, which is essential for preserving lean muscle mass during weight loss. Understanding how to maintain balanced nutrition whilst on these medications is crucial for optimising both metabolic health and treatment outcomes.
Can You Have a Protein Shake for Lunch on GLP-1 Treatment?
Yes, you can have a protein shake for lunch whilst taking GLP-1 medications, and for many patients, this can be a practical solution to meet nutritional needs when appetite is significantly reduced. No specific contraindication is listed in UK product information, though you should discuss this approach with your healthcare professional, particularly if you have kidney disease or other conditions requiring protein restriction.
The reduced appetite and early satiety experienced on GLP-1 treatment can make consuming traditional meals challenging. Some patients report feeling uncomfortably full after only a few bites of solid food, or they may experience nausea that makes eating less appealing. In these circumstances, a well-formulated protein shake can provide essential nutrients in a more tolerable form. Liquid nutrition is often easier to consume when solid food feels overwhelming, and it can help prevent the nutritional deficiencies that may arise from persistently low food intake.
However, it is important to consider that protein shakes should complement, not entirely replace, a varied diet over the long term. Whilst they can be a convenient option for one meal, relying exclusively on liquid nutrition may lead to inadequate intake of fibre, vitamins, minerals, and other beneficial compounds found in whole foods. The goal is to use protein shakes strategically—perhaps when appetite is at its lowest or when time constraints make preparing a balanced meal difficult—whilst still incorporating whole foods whenever possible.
Individual tolerance varies considerably among those taking GLP-1 medications. Some patients find that protein shakes sit well in the stomach, whilst others may experience bloating or discomfort, particularly if the shake is high in fat or consumed too quickly. It is advisable to start with smaller portions and assess your body's response before making protein shakes a regular part of your routine.
If you are taking oral semaglutide (Rybelsus), remember that it must be taken on an empty stomach with a small sip of water, and you should wait at least 30 minutes before eating, drinking or taking other oral medicines.
Nutritional Considerations for Protein Shakes with GLP-1 Therapy
When incorporating protein shakes into your diet whilst on GLP-1 treatment, selecting the right formulation is essential to support your health goals and avoid exacerbating gastrointestinal side effects. The ideal protein shake should provide adequate protein, be relatively low in added sugars, and contain a balance of other macronutrients to support sustained energy and satiety.
Protein content is the primary consideration. Aim for a shake that provides about 20–30 grams of high-quality protein per serving. This amount helps preserve lean muscle mass during weight loss, which is particularly important as GLP-1-induced weight reduction can include loss of both fat and muscle tissue. Whey protein, casein, soy protein, and pea protein are all suitable options, each with slightly different digestion rates and amino acid profiles. Whey protein is rapidly absorbed and rich in branched-chain amino acids, making it excellent for muscle maintenance. Plant-based proteins such as pea or soy are appropriate alternatives for those with dairy intolerance or dietary preferences. If you have kidney disease, discuss protein intake with your healthcare team, as you may need to limit your consumption.
Carbohydrate and sugar content should be monitored carefully. Many commercial protein shakes contain significant amounts of added sugars, which can cause rapid blood glucose spikes and may worsen nausea or gastrointestinal discomfort. According to UK food labelling guidance, products with 5g or less of sugar per 100g (or 2.5g or less per 100ml for liquids) are considered low in sugar. For individuals with diabetes, monitoring carbohydrate content is particularly important for maintaining stable glycaemic control.
Healthy fats can be beneficial in moderation, as they slow digestion and promote satiety. However, excessive fat content may delay gastric emptying further—on top of the effect already caused by GLP-1 medications—potentially leading to prolonged fullness, bloating, or nausea. Choose products with moderate amounts of unsaturated fats rather than those high in saturated fat.
Fibre content is worth considering, especially as constipation is a common side effect of GLP-1 medications. Some protein shakes contain added fibre, which can help maintain bowel regularity. Aim for products with 3-5g of fibre per serving, or consider adding fibre from whole foods such as fruit or oats if making your own shake.
Finally, consider micronutrient fortification. Some protein shakes are enriched with vitamins and minerals, which can help address potential deficiencies when overall food intake is reduced. If you're regularly using protein shakes as meal replacements, products specifically designed as meal replacements (with a balanced vitamin and mineral profile) may be more appropriate than pure protein supplements. Always check allergen information, particularly if you have sensitivities to common ingredients like milk, soy, or certain sweeteners.
Potential Side Effects of Protein Shakes While Taking GLP-1
Whilst protein shakes can be a valuable nutritional tool during GLP-1 therapy, they may also contribute to or exacerbate certain gastrointestinal side effects that are already common with these medications. Understanding these potential issues can help you make informed choices and adjust your approach as needed.
Nausea and gastrointestinal discomfort are among the most frequently reported adverse effects of GLP-1 receptor agonists, particularly during the initial weeks of treatment or following dose escalations. Protein shakes, especially those that are high in fat, very thick in consistency, or consumed too quickly, may worsen these symptoms. The delayed gastric emptying caused by GLP-1 medications means that the stomach takes longer to process its contents, and adding a dense liquid meal can sometimes feel heavy or uncomfortable. To minimise this, consider diluting your shake with extra water or unsweetened almond milk, sipping it slowly over 20–30 minutes, and avoiding consumption immediately after other meals.
Bloating and flatulence can occur, particularly with protein shakes that contain certain ingredients. Whey protein concentrate (as opposed to isolate) contains lactose, which may cause digestive upset in individuals with lactose intolerance. Similarly, some plant-based proteins and added fibres can increase gas production. If you experience these symptoms, switching to a lactose-free or low-FODMAP protein powder may help. Additionally, some shakes contain sugar alcohols (such as sorbitol or xylitol) as sweeteners, which are known to cause bloating and diarrhoea in sensitive individuals.
Constipation is another common side effect of GLP-1 medications, and relying heavily on protein shakes without adequate fibre intake can worsen this issue. Whilst protein is essential, it does not provide the dietary fibre found in whole foods such as vegetables, fruits, and whole grains. If protein shakes become a regular meal replacement, ensure you are consuming sufficient fibre from other sources and staying well hydrated.
Hypoglycaemia risk is generally low with GLP-1 medications alone, but can increase significantly if you are also taking insulin or sulfonylureas. If you're using these medications together, monitor your blood glucose levels regularly and discuss with your healthcare provider whether medication adjustments are needed.
There is no official evidence linking protein shakes to serious adverse interactions with GLP-1 medications. However, if you experience persistent or severe gastrointestinal symptoms, it is important to discuss these with your GP or diabetes specialist nurse, as dose adjustments or alternative strategies may be appropriate.
Seek urgent medical attention if you develop severe, persistent abdominal pain (with or without vomiting), especially if it radiates to your back, as this could indicate pancreatitis. Similarly, seek prompt care for right upper abdominal pain, fever or yellowing of the skin/eyes (possible gallbladder issues), or if you're unable to keep fluids down and show signs of dehydration such as dizziness, very dark urine, or minimal urination.
If you suspect you've experienced a side effect from your medication, you can report it via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or through the Yellow Card app.
Best Practices for Meal Replacement on GLP-1 Medications
Adopting a thoughtful approach to meal replacement whilst on GLP-1 therapy can help you maintain adequate nutrition, manage side effects, and support your overall health goals. The following best practices are informed by clinical experience and align with guidance from organisations such as NICE and the British Dietetic Association.
Prioritise protein intake across all meals and snacks. Aim for a minimum of 1.0–1.2 grams of protein per kilogram of body weight daily (based on ideal or adjusted body weight if you have obesity), and potentially higher if you are physically active or experiencing significant weight loss. If you have kidney disease, discuss appropriate protein intake with your healthcare team. Protein shakes can contribute to this target, but try to include protein-rich whole foods such as lean meats, fish, eggs, legumes, and dairy products whenever appetite allows. Distributing protein intake throughout the day, rather than concentrating it in one meal, optimises muscle protein synthesis.
Maintain variety and balance in your diet. Whilst protein shakes are convenient, they should not completely replace whole foods over extended periods. Vegetables, fruits, whole grains, and healthy fats provide essential nutrients, antioxidants, and fibre that are not present in most protein supplements. Consider using protein shakes strategically—for example, as a quick breakfast option or a post-exercise recovery drink—whilst making lunch or dinner a more varied, whole-food meal when possible.
Stay hydrated, as both GLP-1 medications and high-protein diets can increase fluid requirements. The NHS recommends 6-8 cups or glasses of fluid daily, and more if you are physically active or experiencing gastrointestinal side effects such as diarrhoea. Adequate hydration also helps prevent constipation, a common issue with GLP-1 therapy.
Include regular physical activity, particularly resistance exercises, to help preserve muscle mass during weight loss. The UK Chief Medical Officers recommend strength training activities at least twice weekly, alongside aerobic activity, for overall health benefits.
Monitor your response and adjust accordingly. Keep track of how you feel after consuming protein shakes—note any patterns of nausea, bloating, or discomfort. If certain products or timings seem to worsen symptoms, experiment with alternatives. Some patients find that consuming protein shakes earlier in the day is better tolerated than later in the evening.
Seek professional guidance when needed. If you are struggling to meet your nutritional needs, experiencing unintended muscle loss, or finding it difficult to manage side effects, consult your GP or ask for a referral to a registered dietitian. For complex obesity management or persistent nutritional issues, specialist weight management services may be appropriate. Regular monitoring of weight, body composition, and metabolic markers is also advisable to ensure your approach is supporting your health effectively.
Frequently Asked Questions
How much protein should I aim for in a shake whilst on GLP-1 medication?
Aim for 20–30 grams of high-quality protein per serving to help preserve muscle mass during weight loss. Distribute protein intake throughout the day for optimal benefit, and discuss appropriate amounts with your healthcare team if you have kidney disease.
Can protein shakes worsen nausea from GLP-1 medications?
Protein shakes may worsen nausea if they are high in fat, very thick, or consumed too quickly. Dilute your shake with extra liquid, sip slowly over 20–30 minutes, and choose products lower in fat to minimise gastrointestinal discomfort.
Should I replace all meals with protein shakes on GLP-1 therapy?
No, protein shakes should complement rather than entirely replace whole foods. Whilst convenient for one meal, relying exclusively on liquid nutrition may lead to inadequate fibre, vitamins, and minerals found in vegetables, fruits, and whole grains.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












