Ozempic (semaglutide) is a once-weekly subcutaneous injection licensed in the UK for type 2 diabetes mellitus. Correct administration technique, including proper selection of Ozempic shot locations on the body, is essential for optimal medication absorption, treatment efficacy, and patient comfort. The MHRA and manufacturer specify three approved injection sites: the abdomen, thigh, and upper arm. Understanding where and how to inject Ozempic, alongside systematic site rotation, helps minimise injection site reactions and ensures consistent glycaemic control. This guide provides evidence-based recommendations aligned with UK clinical guidance to support safe, effective Ozempic administration.
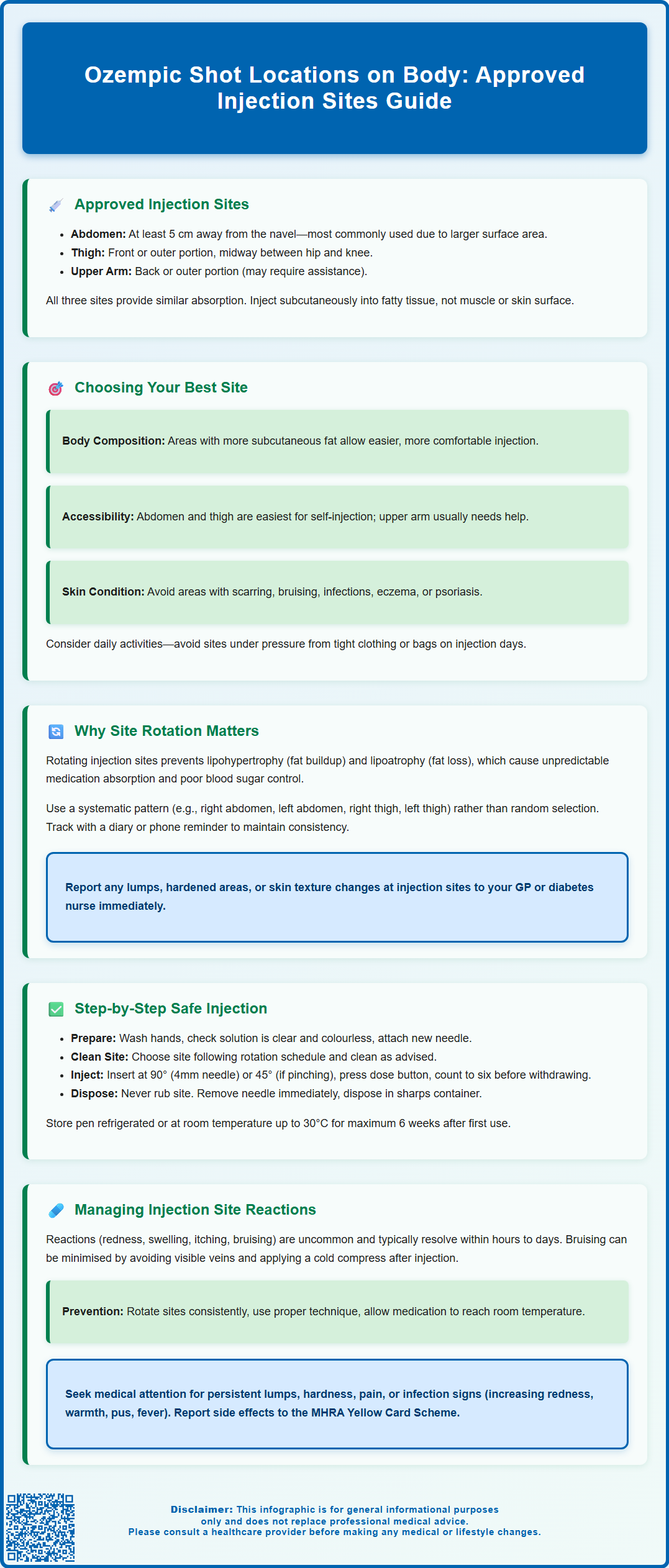
Summary: Ozempic should be injected subcutaneously into one of three approved body sites: the abdomen (at least 5 cm from the navel), the front or outer thigh, or the back or outer upper arm.
- Semaglutide (Ozempic) is a GLP-1 receptor agonist administered once weekly via subcutaneous injection for type 2 diabetes mellitus management.
- All three approved injection sites provide similar medication absorption when proper subcutaneous technique is used.
- Systematic site rotation with each dose prevents lipodystrophy (abnormal fat tissue changes) and ensures predictable medication absorption.
- Injection site reactions such as redness, bruising, or mild swelling are uncommon and typically resolve within hours to days without intervention.
- Patients should avoid injecting into areas with scarring, active skin conditions, or signs of infection, and report persistent lumps or reactions to their GP or diabetes nurse.
Table of Contents
Where to Inject Ozempic: Approved Body Sites
Ozempic (semaglutide) is a once-weekly subcutaneous injection licensed in the UK for the treatment of type 2 diabetes mellitus. A different semaglutide formulation, Wegovy, is licensed for weight management under NICE guidance. The Medicines and Healthcare products Regulatory Agency (MHRA) and the manufacturer specify three approved injection sites for Ozempic administration: the abdomen (tummy), the thigh (front or outer areas), and the upper arm (back or outer portion).
The abdomen is often the most commonly used site, as it typically offers a larger surface area with adequate subcutaneous fat for comfortable injection. According to standard injection technique guidance, patients should inject at least 5 centimetres away from the navel (belly button) to avoid areas with less subcutaneous tissue or increased vascularity. The thigh provides an accessible alternative, particularly for patients who prefer self-administration in a seated position. The recommended area is the front or outer aspect of the thigh, midway between the hip and knee. The upper arm is the third approved site, though it may be more challenging for self-injection and is often used when a carer or healthcare professional administers the medication.
It is essential to inject Ozempic subcutaneously (under the skin, into the fatty tissue) rather than intramuscularly or intradermally. Subcutaneous administration ensures appropriate absorption and reduces the risk of adverse effects. Patients should avoid injecting into areas with scarring, bruising, redness, or skin abnormalities. According to the Ozempic SmPC, the medication's exposure remains similar regardless of which approved injection site is used. However, proper technique and site rotation remain critical for patient comfort and treatment adherence.
How to Choose the Best Injection Site for Ozempic
Selecting the most appropriate injection site for Ozempic depends on several individual factors, including body composition, personal comfort, accessibility, and any pre-existing skin conditions. Patients with more subcutaneous fat in the abdominal area may find this site most comfortable, as adequate fatty tissue facilitates easier needle insertion and reduces discomfort. Conversely, individuals with less abdominal fat might prefer the thigh, where subcutaneous tissue is often more accessible.
Accessibility and ease of self-administration are important practical considerations. The abdomen and thigh are generally easier to reach independently, whilst the upper arm typically requires assistance for safe subcutaneous administration. Patients with limited mobility, arthritis, or visual impairment should discuss their preferred injection site with their diabetes specialist nurse or GP, who can provide tailored advice and training.
Certain medical conditions or skin changes may influence site selection. Patients should avoid areas with active skin infections, inflammation, eczema, psoriasis, or recent surgical scars. Those with lipodystrophy (abnormal fat distribution) from previous injectable therapies should select sites with healthy subcutaneous tissue. Additionally, individuals who engage in activities that place pressure on specific body areas—such as wearing tight waistbands or carrying bags on the shoulder—may wish to avoid injecting in those locations on days when such pressure is anticipated.
Patients should also consider their injection schedule and routine. Some individuals prefer to use the same general area (e.g., always the abdomen) but rotate within that region, whilst others alternate between different body sites each week. There is no single "best" site for everyone; the optimal choice is one that the patient can access comfortably, perform safely, and maintain consistently as part of their weekly treatment regimen. Healthcare professionals can provide individualised guidance during initial training and follow-up appointments.
Rotating Ozempic Injection Sites: Why It Matters
Systematic rotation of injection sites is a fundamental aspect of safe Ozempic administration and is recommended in the manufacturer's guidance and Forum for Injection Technique (FIT UK) recommendations. Repeatedly injecting into the same spot can lead to lipohypertrophy (localised fat accumulation) or lipoatrophy (loss of fatty tissue), both forms of lipodystrophy that can compromise medication absorption and glycaemic control.
Lipohypertrophy presents as firm lumps or thickened areas under the skin, resulting from chronic trauma to subcutaneous tissue. These areas have altered vascularity and may cause unpredictable absorption of semaglutide, potentially leading to suboptimal diabetes management or increased variability in blood glucose levels. While lipodystrophy is more commonly associated with insulin therapy, it can occur with other subcutaneous injections, which is why site rotation remains a cornerstone of good injection practice.
Proper rotation also reduces the risk of injection site reactions, including pain, bruising, and localised inflammation. By rotating sites with each dose and avoiding the exact same spot, patients minimise cumulative tissue trauma. This is particularly important for long-term treatment with Ozempic's once-weekly dosing schedule.
Patients should develop a systematic rotation pattern rather than random site selection. For example, one might use the right abdomen one week, left abdomen the next, then right thigh, left thigh, and so forth. Keeping a simple diary or using a smartphone reminder can help maintain this pattern. During routine diabetes reviews, healthcare professionals should examine injection sites for signs of lipodystrophy and reinforce the importance of rotation. Patients who notice any lumps, hardened areas, or changes in skin texture should report these to their GP or diabetes nurse promptly.
Step-by-Step Guide to Injecting Ozempic Safely
Preparation is essential for safe Ozempic administration. Begin by washing your hands thoroughly with soap and water, then dry them completely. Remove the Ozempic pen from the refrigerator approximately 15–30 minutes before injection if desired, as this may reduce injection discomfort, though this is optional. Check the medication's appearance through the pen window—it should be clear and colourless. Do not use the pen if the solution appears cloudy, discoloured, or contains particles.
Attach a new needle to the pen for each injection, following the manufacturer's instructions. Remove both the outer and inner needle caps. Perform a flow check before your first use of each new pen to ensure proper function, as detailed in the patient information leaflet. Select your injection site according to your rotation schedule, ensuring the area is clean and dry. Whilst the manufacturer does not require alcohol swabbing for patients with good hygiene and intact skin, some healthcare professionals recommend it—follow your diabetes team's specific advice.
To inject: If using a 4 mm needle (the preferred length), insert at a 90-degree angle without pinching the skin. If you have very little subcutaneous fat or are using a longer needle, gently pinch a fold of skin between your thumb and forefinger and insert the needle at a 45-degree angle. Press the dose button fully and hold it down whilst keeping the needle in the skin. Count slowly to six (as directed in your patient leaflet) to ensure complete dose delivery, then withdraw the needle straight out.
After injection, do not rub the site, as this may affect absorption. For safe needle disposal, use the outer needle cap to carefully remove the needle, then dispose of it immediately in a sharps container. Replace the pen cap and store the pen as directed (refrigerated before first use, then either refrigerated or at room temperature up to 30°C for up to 6 weeks/42 days after first use). Record the injection site and date to maintain your rotation schedule. If you notice bleeding, apply gentle pressure with a clean tissue; minor bleeding is normal and not a cause for concern.
Common Injection Site Reactions and How to Manage Them
Injection site reactions can occur with Ozempic and typically resolve without intervention. The most frequently reported reactions include temporary redness, slight swelling, itching, or bruising at the injection site. These reactions usually appear shortly after injection and resolve within a few hours to several days. According to the Ozempic SmPC, injection site reactions are uncommon, making them less frequent than gastrointestinal side effects but still worth recognising.
Bruising occurs when the needle inadvertently punctures a small blood vessel. Whilst generally harmless, frequent bruising may indicate poor injection technique or use of excessive force. To minimise bruising, ensure the needle is inserted smoothly, avoid injecting into areas with visible veins, and do not rub the site after injection. Applying a cold compress (not ice directly on skin) for a few minutes after injection may help reduce bruising and discomfort.
Persistent lumps, hardness, or pain at injection sites warrant medical attention, as these may indicate lipodystrophy or, rarely, infection. Signs of infection include increasing redness, warmth, swelling, pus, or fever. Patients experiencing these symptoms should contact their GP promptly. Allergic reactions at the injection site—characterised by extensive redness, severe itching, or hives—are uncommon but require medical assessment. Systemic allergic reactions (difficulty breathing, facial swelling, rapid heartbeat) are rare but constitute a medical emergency requiring immediate attention via 999.
To manage minor reactions: rotate sites diligently, ensure proper injection technique, allow the medication to reach room temperature before injecting if preferred, and avoid injecting into areas with existing irritation. If you experience any suspected side effects, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk). If injection site reactions persist beyond a few days, worsen over time, or significantly affect quality of life, patients should consult their diabetes specialist nurse or GP. Most reactions can be effectively managed through technique refinement and site rotation, allowing patients to continue their Ozempic therapy safely and comfortably.
Frequently Asked Questions
Can I inject Ozempic in the same spot each week?
No, you should rotate injection sites with each dose to prevent lipodystrophy (tissue changes) that can affect medication absorption and glycaemic control. Develop a systematic rotation pattern across approved sites rather than using the exact same spot repeatedly.
Which Ozempic injection site is best for self-administration?
The abdomen and thigh are generally easiest for self-injection, as they are more accessible than the upper arm. The optimal site depends on individual factors including body composition, comfort, and any pre-existing skin conditions—discuss your preference with your diabetes specialist nurse.
What should I do if I notice a lump at my Ozempic injection site?
Persistent lumps, hardness, or pain at injection sites may indicate lipodystrophy and warrant medical attention. Avoid injecting into affected areas and contact your GP or diabetes nurse promptly for assessment and guidance on site selection.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript