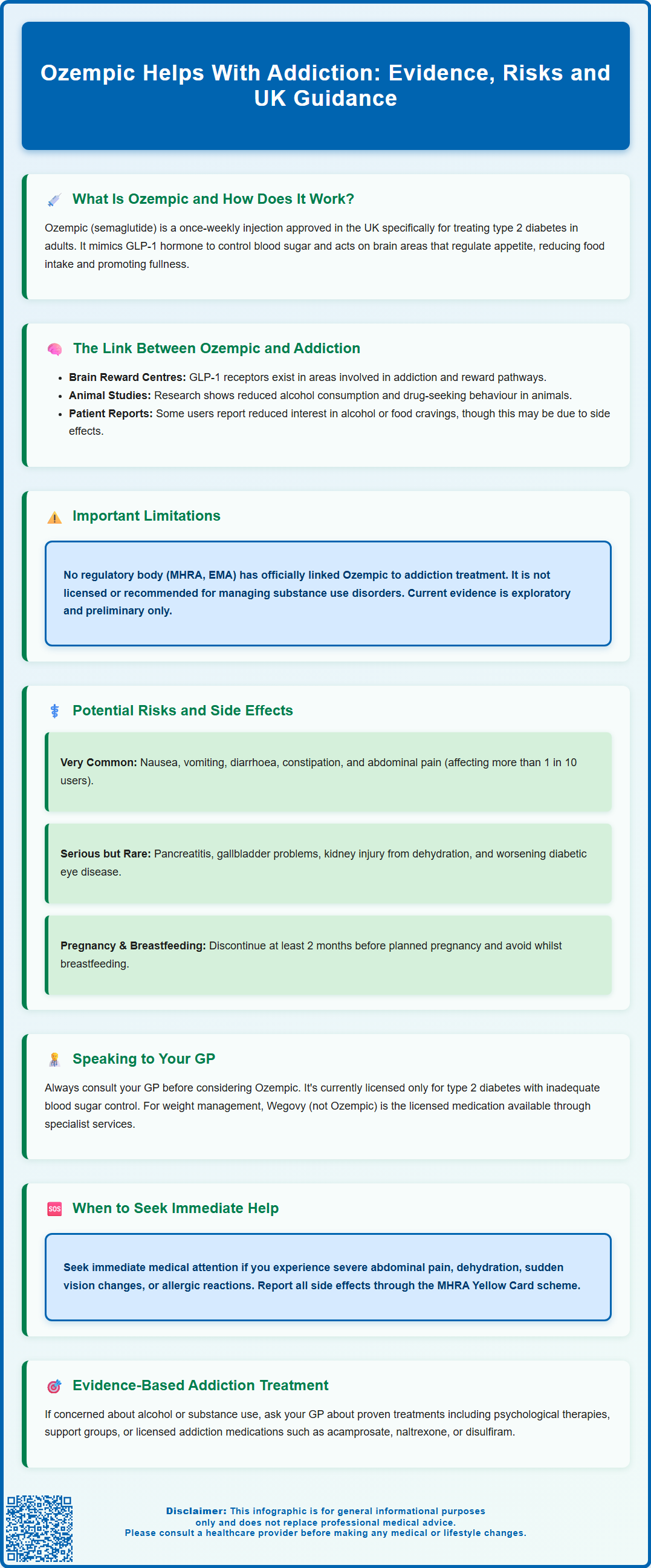
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus in adults. Emerging research suggests that GLP-1 receptor agonists may influence addictive behaviours, including alcohol use disorder and substance misuse, by acting on brain reward pathways. However, Ozempic is not approved by the MHRA or recommended by NICE for addiction treatment, and evidence remains preliminary. This article examines the current research, potential mechanisms, safety considerations, and the importance of consulting your GP before considering any off-label use.
Summary: Ozempic is not approved for addiction treatment in the UK, though emerging research suggests GLP-1 receptor agonists may influence reward pathways involved in addictive behaviours.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed only for type 2 diabetes mellitus management in the UK.
- Preclinical studies show GLP-1 receptor agonists may reduce alcohol consumption and drug-seeking behaviour in animal models by modulating brain reward circuitry.
- Human evidence remains preliminary, with no established regulatory link between Ozempic and addiction treatment by the MHRA or NICE.
- Common side effects include nausea, vomiting, diarrhoea, and abdominal pain; serious risks include pancreatitis, gallbladder problems, and hypoglycaemia when combined with certain diabetes medications.
- Patients interested in Ozempic for any reason should consult their GP for individualised assessment, as off-label use for addiction is not recommended outside clinical trials.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults, as an adjunct to diet and exercise. It belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone called GLP-1. This hormone plays several important roles in regulating blood sugar levels and appetite.
The primary mechanism of action involves stimulating insulin secretion from the pancreas when blood glucose levels are elevated, whilst simultaneously suppressing the release of glucagon, a hormone that raises blood sugar. Ozempic also slows gastric emptying, meaning food moves more slowly from the stomach into the small intestine, which helps to reduce post-meal blood sugar spikes and promotes a feeling of fullness. Additionally, GLP-1 receptor agonists act on areas of the brain involved in appetite regulation, particularly the hypothalamus, which can lead to reduced food intake.
Ozempic is administered as a once-weekly subcutaneous injection, typically starting at an initiation dose of 0.25 mg for 4 weeks, then increasing to 0.5 mg. The dose may be increased to 1 mg or 2 mg after at least 4 weeks at each dose level, depending on individual response and tolerability. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Ozempic specifically for glycaemic control in type 2 diabetes, often in combination with other glucose-lowering medications or as monotherapy when metformin is not tolerated. It is not indicated for type 1 diabetes or diabetic ketoacidosis.
Whilst Ozempic has gained considerable attention for its effects on weight loss, it is not licensed for weight management in the UK. A higher-dose formulation called Wegovy (also semaglutide, 2.4 mg) has been specifically licensed for weight management. Understanding how this medication works in the brain and body is essential context for exploring emerging research into its potential effects on addictive behaviours.
The Link Between Ozempic and Addiction: What Research Shows
Emerging research has begun to explore whether GLP-1 receptor agonists like Ozempic might influence addictive behaviours, including alcohol use disorder, substance misuse, and behavioural addictions. This interest stems from the fact that GLP-1 receptors are found not only in the pancreas and gastrointestinal tract but also in key brain regions associated with reward processing, including the mesolimbic dopamine system—the same neural pathway implicated in addiction.
Several preclinical studies in animal models have demonstrated that GLP-1 receptor agonists can reduce alcohol consumption, drug-seeking behaviour, and the rewarding effects of substances such as cocaine and nicotine. These findings suggest that activation of GLP-1 receptors may modulate the brain's reward circuitry, potentially dampening the reinforcing effects of addictive substances. Some researchers hypothesise that by influencing dopamine signalling and reducing the hedonic response to rewards, these medications might help individuals reduce cravings and consumption.
Human research in this area remains preliminary. Some patients prescribed semaglutide for diabetes or weight management have reported reduced interest in alcohol or decreased cravings for certain foods in small observational studies. However, it is important to note that these effects could be attributable to the medication's gastrointestinal side effects and appetite suppression, rather than direct effects on reward pathways. Systematic reviews of GLP-1 receptor agonists in substance use disorders suggest the need for larger, well-designed clinical trials before drawing conclusions.
It is crucial to emphasise that there is no official link established by regulatory bodies such as the MHRA or the European Medicines Agency (EMA) between Ozempic and addiction treatment. The medication is not licensed for managing substance use disorders, and GLP-1 receptor agonists are not recommended for substance use disorders by NICE or the MHRA. These medications should not be used off-label for addiction outside of clinical trials. Current evidence remains largely exploratory, and healthcare professionals should interpret these findings with appropriate caution whilst awaiting more definitive research.
Potential Risks and Side Effects to Consider
Like all medications, Ozempic carries potential adverse effects that patients and healthcare professionals must carefully consider. The most commonly reported side effects are gastrointestinal in nature, affecting a significant proportion of users, particularly during dose escalation. These include:
-
Nausea and vomiting (very common, affecting more than 1 in 10 people)
-
Diarrhoea or constipation
-
Abdominal pain and bloating
-
Reduced appetite, which whilst therapeutically beneficial for some, may be problematic for others
These gastrointestinal symptoms typically improve over time as the body adjusts to the medication, but they can occasionally be severe enough to require dose reduction or discontinuation.
More serious but less common risks include:
-
Pancreatitis (inflammation of the pancreas)—patients should seek immediate medical attention if they experience severe, persistent abdominal pain
-
Gallbladder problems, including gallstones and cholecystitis
-
Hypoglycaemia (low blood sugar), particularly when used in combination with insulin or sulphonylureas (risk is lower when used alone)
-
Diabetic retinopathy complications in patients with pre-existing eye disease
-
Acute kidney injury, especially in patients who become dehydrated from vomiting or diarrhoea
-
Hypersensitivity reactions including angioedema and injection-site reactions
-
Small increases in heart rate
Animal studies have shown an increased risk of thyroid C-cell tumours in rodents, though the relevance to humans is unknown. Patients should report any symptoms such as a neck mass, difficulty swallowing, breathing difficulties, or persistent hoarseness to their healthcare provider.
Ozempic should be avoided during pregnancy and should be discontinued at least 2 months before a planned pregnancy. It is also not recommended during breastfeeding.
When starting Ozempic, insulin should not be abruptly reduced or stopped due to the risk of diabetic ketoacidosis. Any adjustments to insulin or other diabetes medications should be made under medical supervision.
Regarding addiction-related considerations, if Ozempic does indeed reduce reward-seeking behaviour, there is a theoretical concern about whether this might affect motivation or pleasure in other areas of life, though this has not been systematically studied.
If you experience any side effects while taking Ozempic, report them to your healthcare provider and consider reporting them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Speaking to Your GP: Is Ozempic Right for You?
If you are interested in Ozempic—whether for diabetes management, weight control, or because you have read about potential effects on addictive behaviours—the first step is always a comprehensive consultation with your GP or specialist. It is essential to approach this conversation with realistic expectations and an understanding that Ozempic is currently licensed only for specific indications.
Questions to discuss with your healthcare provider include:
-
Whether you meet the clinical criteria for Ozempic prescription (type 2 diabetes with inadequate glycaemic control)
-
Your complete medical history, including any history of pancreatitis, thyroid disease, kidney problems, or diabetic eye disease
-
Current medications and potential drug interactions
-
Your individual risk-benefit profile, considering both potential therapeutic benefits and adverse effects
-
Realistic expectations about outcomes, timelines, and the need for ongoing monitoring
-
Pregnancy plans or breastfeeding status, as Ozempic should be avoided in these circumstances
If you are specifically interested in weight management, be aware that Wegovy (semaglutide 2.4 mg) rather than Ozempic is licensed for this purpose. NICE guidance specifies eligibility criteria including BMI thresholds (typically BMI ≥35 kg/m² with weight-related comorbidities, or ≥30 kg/m² with type 2 diabetes), use within specialist weight management services, and treatment duration limits.
If you are concerned about alcohol use or other addictive behaviours, it is vital to be open and honest with your GP about these issues. Whilst Ozempic is not an approved treatment for addiction, your doctor can:
-
Assess whether you might benefit from evidence-based addiction treatments, such as psychological therapies, support groups, or medications specifically licensed for substance use disorders (such as acamprosate, naltrexone or disulfiram for alcohol dependence)
-
Refer you to specialist NHS alcohol or drug services if appropriate
-
Discuss smoking cessation services and support if relevant
-
Discuss whether Ozempic might be suitable for you if you also have type 2 diabetes
-
Monitor you carefully if Ozempic is prescribed, watching for both intended effects and any unexpected changes in behaviour or wellbeing
NICE guidance emphasises shared decision-making and individualised care. Your GP will consider your unique circumstances, preferences, and clinical needs when determining the most appropriate treatment pathway. Remember that emerging research, whilst promising, does not yet constitute sufficient evidence to prescribe Ozempic off-label for addiction management outside of clinical trials.
If you experience any concerning symptoms whilst taking Ozempic, such as severe abdominal pain, signs of dehydration, sudden vision changes, or allergic reactions, contact your GP promptly or seek urgent care through NHS 111 or 999 if symptoms are severe. Never alter your diabetes medications, especially insulin, without medical guidance.
Frequently Asked Questions
Is Ozempic approved for treating addiction in the UK?
No, Ozempic is not approved by the MHRA or recommended by NICE for treating addiction. It is licensed only for type 2 diabetes mellitus management, and evidence for addiction treatment remains preliminary and exploratory.
How might Ozempic affect addictive behaviours?
GLP-1 receptors are found in brain regions associated with reward processing, and preclinical studies suggest GLP-1 receptor agonists may reduce cravings and reward-seeking behaviour by modulating dopamine signalling. However, human research is limited and inconclusive.
What should I do if I'm interested in Ozempic for addiction concerns?
Speak openly with your GP about addiction concerns. They can assess whether you meet criteria for Ozempic if you have type 2 diabetes, refer you to evidence-based addiction services, and discuss approved treatments for substance use disorders such as psychological therapies or licensed medications.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript