Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist widely prescribed in the UK for managing type 2 diabetes mellitus. Whilst highly effective at improving glycaemic control, Ozempic delayed gastric emptying is a key pharmacological action that can lead to digestive symptoms. Understanding how this medication affects gastric motility helps patients and healthcare professionals anticipate and manage common gastrointestinal side effects. This article explores the mechanisms behind delayed gastric emptying, associated symptoms, practical management strategies, and when to seek medical advice, all aligned with UK clinical guidance from NICE, the MHRA, and NHS recommendations.
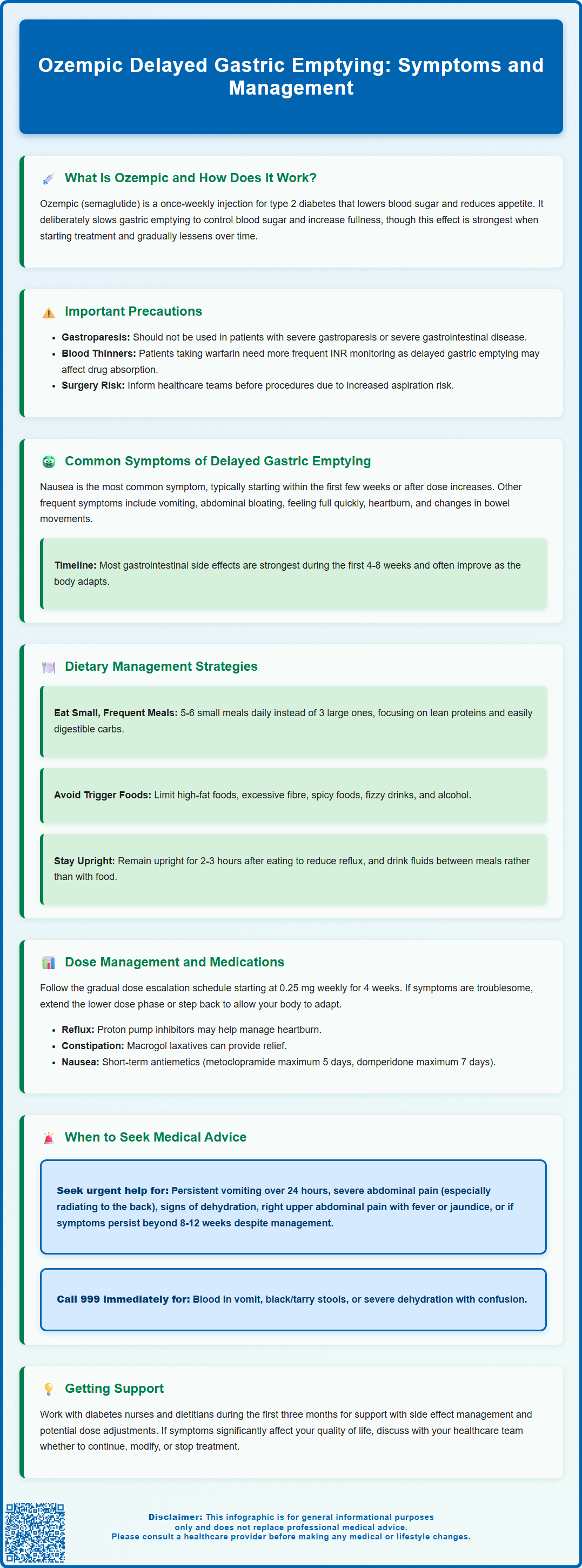
Summary: Ozempic (semaglutide) delays gastric emptying by activating GLP-1 receptors in the gastrointestinal tract, slowing food transit from the stomach to the small intestine.
- Semaglutide is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus, administered as a once-weekly subcutaneous injection.
- Delayed gastric emptying is most pronounced early in treatment and typically attenuates over time with continued use.
- Common symptoms include nausea, vomiting, abdominal bloating, early satiety, and reflux, usually improving within 4–8 weeks.
- Management involves smaller frequent meals, avoiding high-fat foods, gradual dose titration, and symptomatic relief under GP guidance.
- Patients should seek urgent medical advice for persistent vomiting, severe abdominal pain, signs of pancreatitis, dehydration, or gastrointestinal bleeding.
- Semaglutide is not recommended in patients with severe gastroparesis or severe gastrointestinal disease according to the SmPC.
Table of Contents
What Is Ozempic and How Does It Affect Gastric Emptying?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works through multiple mechanisms to improve glycaemic control, including enhancing insulin secretion, suppressing glucagon release, and reducing appetite. The Medicines and Healthcare products Regulatory Agency (MHRA) approved Ozempic based on clinical trial data demonstrating significant reductions in HbA1c levels and body weight.
One of the pharmacological actions of semaglutide is its effect on gastric motility. GLP-1 receptors are present throughout the gastrointestinal tract, and when activated, they slow the rate at which food moves from the stomach into the small intestine—a process known as gastric emptying. This delayed gastric emptying is most pronounced early in treatment and tends to attenuate over time with continued use, though it may still influence postprandial glucose levels. Clinical studies have shown that semaglutide prolongs gastric emptying time compared to placebo, particularly during initial therapy.
Patients taking warfarin or other coumarin derivatives should have more frequent INR monitoring when starting Ozempic, as the delayed gastric emptying may affect drug absorption. Understanding this pharmacological action is essential for both healthcare professionals and patients, as it explains many of the digestive symptoms associated with Ozempic therapy and informs appropriate management strategies. The National Institute for Health and Care Excellence (NICE) recognises GLP-1 receptor agonists as valuable treatment options within structured diabetes care pathways.
Symptoms of Delayed Gastric Emptying on Ozempic
Delayed gastric emptying associated with Ozempic can manifest through a range of gastrointestinal symptoms, which are among the most commonly reported adverse effects of GLP-1 receptor agonist therapy. The most frequent symptoms include:
-
Nausea: Often the earliest and most prevalent symptom, typically occurring within the first few weeks of treatment or following dose escalation. Nausea may be mild to moderate and often improves with continued therapy.
-
Vomiting: Less common than nausea but can occur, particularly if large meals are consumed or if dose titration is too rapid.
-
Abdominal discomfort and bloating: Patients may experience a sensation of fullness, distension, or pressure in the upper abdomen, even after consuming small amounts of food.
-
Early satiety: Feeling full quickly during meals, which whilst contributing to weight loss, can be uncomfortable and may affect nutritional intake.
-
Indigestion and reflux: Delayed gastric emptying can exacerbate gastro-oesophageal reflux symptoms, including heartburn and regurgitation.
-
Constipation and diarrhoea: Both are common adverse effects that may require management strategies if persistent.
The severity and duration of these symptoms vary considerably between individuals. According to clinical trial data, gastrointestinal adverse effects are most pronounced during the initial weeks of treatment and during dose escalation phases. For many patients, symptoms often improve within 4-8 weeks as physiological adaptation occurs, though some may experience persistent symptoms requiring intervention.
Patients taking insulin or sulfonylureas should be aware that reduced food intake due to these symptoms, combined with the glucose-lowering effects of their medications, may increase the risk of hypoglycaemia. Dose adjustments of these medications may be necessary and should be discussed with their healthcare team.
It is important to note that whilst these symptoms are related to the pharmacological action of Ozempic, they do not necessarily indicate a pathological condition. However, severe or persistent symptoms warrant clinical assessment to exclude other gastrointestinal pathology and to ensure appropriate management. Healthcare professionals should counsel patients about these potential effects before initiating therapy to set realistic expectations and improve treatment adherence.
Managing Digestive Side Effects While Taking Ozempic
Effective management of digestive side effects related to delayed gastric emptying can significantly improve treatment tolerance and adherence. Dietary modifications represent the cornerstone of symptom management:
-
Smaller, more frequent meals: Consuming 5–6 small meals throughout the day rather than 3 large meals reduces the gastric burden and minimises symptoms of fullness and nausea.
-
Avoiding high-fat foods: Fatty meals delay gastric emptying further and may exacerbate symptoms. Patients should focus on lean proteins, vegetables, and easily digestible carbohydrates.
-
Limiting fibre intake temporarily: Whilst dietary fibre is generally beneficial, excessive amounts may worsen bloating during the adaptation period.
-
Adequate hydration: Maintaining fluid intake between meals (rather than with meals) helps prevent dehydration, particularly if vomiting occurs.
-
Avoiding lying down after eating: Remaining upright for at least 2–3 hours after meals can reduce reflux symptoms.
-
Avoiding triggers: Spicy foods, fizzy drinks, and alcohol may worsen symptoms and should be limited.
Medication strategies should be implemented in consultation with healthcare professionals:
-
Gradual dose titration: Following the recommended dose escalation schedule (typically starting at 0.25 mg weekly for 4 weeks, then 0.5 mg) allows the gastrointestinal system to adapt gradually. If symptoms are troublesome, extending the 0.25 mg phase or stepping back to a previously tolerated dose may be appropriate.
-
Timing of administration: Some patients find that administering the injection on a specific day when they can rest if needed helps manage initial side effects.
-
Symptomatic relief: For persistent reflux symptoms, acid suppression therapy (such as proton pump inhibitors or H2-receptor antagonists) may be prescribed by a GP. For constipation, macrogol laxatives may be appropriate if dietary measures are insufficient.
-
Antiemetics: Short-term use of antiemetics may be appropriate for persistent nausea, but only under GP guidance. Metoclopramide should be used for a maximum of 5 days, and domperidone for a maximum of 7 days at the lowest effective dose. Domperidone should be avoided in patients with cardiac conditions, QT prolongation, or those taking interacting medications.
Patients should follow 'sick day rules' and contact their healthcare team promptly if unable to maintain adequate fluid intake, as dehydration can affect kidney function. Those taking insulin or sulfonylureas may need dose adjustments if food intake is reduced, to prevent hypoglycaemia.
Regular contact with the diabetes care team is essential, particularly during the first three months of treatment. NHS diabetes specialist nurses and dietitians can provide valuable support and practical advice for managing side effects. If symptoms are severe or significantly impact quality of life, dose reduction or temporary treatment interruption may be necessary, followed by slower re-titration. Documentation of symptoms and their impact on daily activities can help healthcare professionals make informed decisions about treatment adjustments.
When to Seek Medical Advice About Gastric Emptying Issues
Whilst mild gastrointestinal symptoms are expected with Ozempic therapy, certain warning signs require prompt medical assessment. Patients should contact their GP or diabetes care team urgently if they experience:
-
Persistent vomiting: Inability to keep down fluids for more than 24 hours, which may lead to dehydration and electrolyte disturbances.
-
Severe abdominal pain: Particularly if constant, worsening, or accompanied by fever. If the pain is severe and persistent, especially if radiating to the back (with or without vomiting), this could indicate pancreatitis—a rare but serious adverse effect. If pancreatitis is suspected, stop Ozempic immediately and seek urgent medical attention.
-
Signs of dehydration: Including reduced urine output, dizziness, dry mouth, or confusion. Call 999 or go to A&E if experiencing severe dehydration or confusion.
-
Unintentional weight loss exceeding expected parameters: Whilst weight reduction is often desirable, excessive or rapid weight loss may indicate inadequate nutritional intake.
-
Blood in vomit or black/tarry stools: This requires immediate medical attention (call 999 or go to A&E) to exclude gastrointestinal bleeding.
-
Right upper quadrant pain, fever, or jaundice: These may indicate gallbladder disease (cholelithiasis or cholecystitis), which occurs more frequently in patients taking GLP-1 receptor agonists.
-
Worsening of pre-existing gastroparesis: Patients with known diabetic gastroparesis should be monitored closely, as Ozempic may exacerbate this condition. Semaglutide is not recommended in patients with severe gastroparesis or severe gastrointestinal disease.
Regular monitoring is essential for all patients on Ozempic therapy. NICE guidance recommends ongoing assessment of treatment response, tolerability, and adverse effects. Healthcare professionals should:
-
Review gastrointestinal symptoms at each follow-up appointment
-
Monitor nutritional status and body weight trends
-
Assess glycaemic control and adjust diabetes management accordingly
-
Consider alternative treatment options if side effects are intolerable despite management strategies
Patients should inform their healthcare team before undergoing endoscopy or surgery, as delayed gastric emptying may increase aspiration risk. Anaesthetists and endoscopists should be made aware of Ozempic use, and local perioperative guidance should be followed.
If symptoms persist beyond 8–12 weeks despite appropriate management, or if they significantly impair quality of life, referral for further assessment may be warranted. This might include tests such as lipase measurement (for pancreatitis), liver function tests and ultrasound (for gallbladder disease), or gastric emptying studies. The decision to continue, modify, or discontinue Ozempic should be made collaboratively between the patient and healthcare team, considering both glycaemic control benefits and tolerability.
Patients are encouraged to report suspected adverse reactions to Ozempic via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
How long does delayed gastric emptying last on Ozempic?
Delayed gastric emptying is most pronounced during the first few weeks of Ozempic treatment and typically improves within 4–8 weeks as the body adapts, though some effect may persist with continued use.
Can I take medication for nausea whilst on Ozempic?
Yes, short-term antiemetics may be prescribed by your GP for persistent nausea. Metoclopramide should be used for a maximum of 5 days and domperidone for a maximum of 7 days at the lowest effective dose, avoiding domperidone in patients with cardiac conditions.
Should I stop Ozempic if I have severe digestive symptoms?
Do not stop Ozempic without consulting your healthcare team. If you experience severe symptoms such as persistent vomiting, severe abdominal pain, or signs of pancreatitis, seek urgent medical advice immediately, as dose adjustment or temporary interruption may be necessary.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript