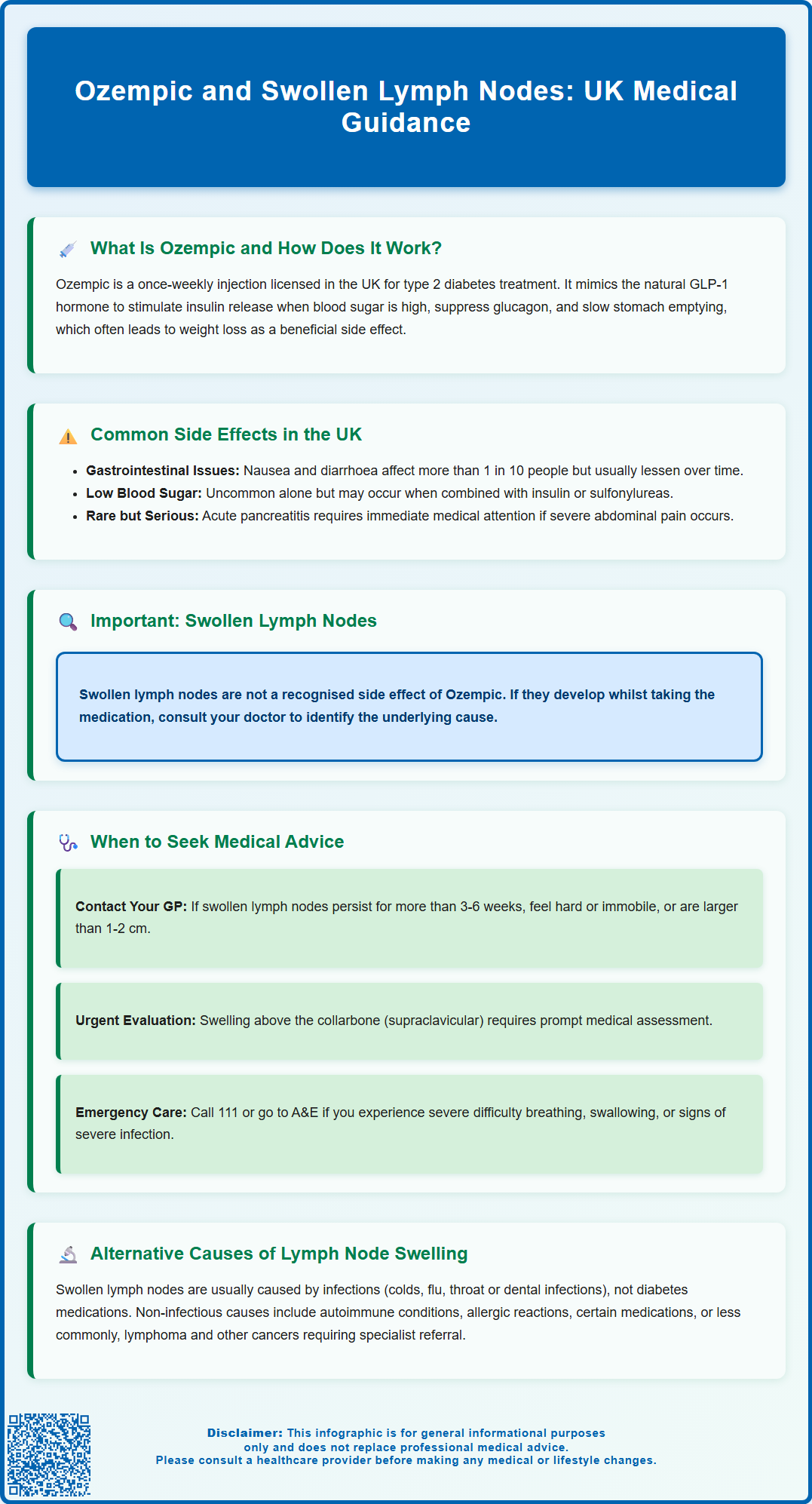
Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for treating type 2 diabetes mellitus in adults. Whilst gastrointestinal symptoms such as nausea and diarrhoea are well-recognised side effects, swollen lymph nodes are not listed among the known adverse reactions to Ozempic in UK regulatory documentation. Lymphadenopathy can arise from numerous causes, including infections, autoimmune conditions, and other medical issues unrelated to diabetes medication. If you develop swollen lymph nodes whilst taking Ozempic, it is important to seek medical evaluation to identify the underlying cause and ensure appropriate management.
Summary: Swollen lymph nodes are not a recognised side effect of Ozempic (semaglutide) according to UK regulatory documentation.
- Ozempic is a GLP-1 receptor agonist licensed for type 2 diabetes treatment, not weight management alone.
- Common side effects include gastrointestinal symptoms such as nausea, diarrhoea, vomiting, and constipation.
- Lymphadenopathy has numerous causes including infections, autoimmune conditions, and malignancies requiring medical assessment.
- Seek GP review if lymph nodes remain swollen beyond 3–6 weeks, are hard or fixed, or accompanied by unexplained weight loss or night sweats.
- NICE guidance recommends urgent two-week referral for lymphadenopathy with features suggestive of malignancy.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medicines called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone in the body.
The mechanism of action of Ozempic involves several complementary pathways. Primarily, it stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released only when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications. Simultaneously, semaglutide suppresses glucagon secretion, a hormone that raises blood glucose levels, thereby helping to maintain more stable glycaemic control throughout the day.
Beyond its effects on insulin and glucagon, Ozempic slows gastric emptying, which means food moves more slowly from the stomach into the small intestine. This contributes to increased satiety and reduced appetite, often resulting in weight loss—a beneficial effect for many patients with type 2 diabetes who are overweight or obese. The medication also acts on appetite centres in the brain, further supporting weight management.
Ozempic is administered as a once-weekly subcutaneous injection, typically in the abdomen, thigh, or upper arm. The MHRA-approved dosing schedule begins with 0.25 mg weekly for four weeks (a non-therapeutic starter dose to improve tolerability), followed by an increase to 0.5 mg weekly. Depending on glycaemic control and tolerability, the dose may be further increased to 1 mg weekly after at least four weeks. For patients requiring additional glycaemic control, the dose may be increased to 2 mg once weekly after at least four weeks at the 1 mg dose.
In the UK, Ozempic is available on NHS prescription for eligible patients meeting NICE criteria for GLP-1 receptor agonist therapy in type 2 diabetes management. It is important to note that while weight loss may occur with Ozempic, it is specifically licensed for type 2 diabetes treatment, not for weight management alone.
Common Side Effects of Ozempic in the UK
Like all medications, Ozempic can cause side effects, though not everyone experiences them. According to the UK Summary of Product Characteristics (SmPC), the most frequently reported adverse effects are gastrointestinal in nature, reflecting the drug's mechanism of slowing gastric emptying and affecting the digestive system.
Gastrointestinal symptoms are the predominant side effects and include:
-
Nausea – very common (may affect more than 1 in 10 people)
-
Diarrhoea – very common
-
Vomiting – common (may affect up to 1 in 10 people)
-
Constipation – common
-
Abdominal pain or discomfort – common
These gastrointestinal effects are usually mild to moderate in severity and tend to diminish over time as the body adjusts to the medication. Managing these symptoms may include eating smaller, low-fat meals, avoiding large or fatty meals, staying well-hydrated, and following the recommended gradual dose titration schedule.
Other notable side effects include:
-
Injection site reactions – such as redness, itching, or bruising at the injection site
-
Fatigue – some patients report feeling more tired than usual
-
Hypoglycaemia – low blood sugar is uncommon with Ozempic alone but may occur when used alongside insulin or sulfonylureas (doses of these medications may need adjustment by your prescriber)
Important safety warnings from the UK SmPC include:
-
Acute pancreatitis – seek immediate medical attention for severe, persistent abdominal pain, with or without vomiting
-
Gallbladder disease – including gallstones and inflammation of the gallbladder
-
Diabetic retinopathy complications – particularly in patients with pre-existing retinopathy when blood glucose improves rapidly
-
Dehydration and kidney problems – severe gastrointestinal side effects may lead to dehydration and acute kidney injury
-
Hypersensitivity reactions – including rash, itching and rarely, anaphylactic reactions
It is important to note that swollen lymph nodes are not listed among the recognised side effects of Ozempic in the UK SmPC or patient information leaflet. If you develop swollen lymph nodes whilst taking Ozempic, this warrants medical evaluation to identify the underlying cause.
Do not stop taking Ozempic without consulting your healthcare provider. If you suspect you are experiencing a side effect from Ozempic, you can report it through the MHRA Yellow Card scheme.
When to Seek Medical Advice About Swollen Lymph Nodes
Swollen lymph nodes (lymphadenopathy) can occur for numerous reasons and should always be evaluated by a healthcare professional, particularly if they persist or are accompanied by other concerning symptoms. While there is no established link between Ozempic and lymph node swelling, any new or unexplained symptom whilst taking medication deserves medical attention.
You should contact your GP or healthcare provider if you notice:
-
Lymph nodes that remain swollen for more than 3-6 weeks without obvious cause
-
Nodes that are hard, fixed, or immobile rather than soft and moveable
-
Progressive enlargement of lymph nodes over time
-
Swollen nodes in multiple areas of the body simultaneously (generalised lymphadenopathy)
-
Supraclavicular lymph nodes (above the collarbone) – these are particularly concerning
-
Nodes measuring more than 1–2 cm in diameter
-
Lymph node swelling accompanied by unexplained weight loss
-
Night sweats that soak your bedclothes
-
Persistent fever without an obvious infection
-
Difficulty breathing or swallowing if nodes are in the neck area
Many of these features may warrant an urgent suspected cancer referral (two-week wait) as per NICE guidance.
Seek urgent medical attention (contact 111 or attend A&E) if:
-
You develop severe difficulty breathing or swallowing
-
Lymph node swelling is accompanied by signs of severe infection, such as high fever, severe pain, or rapidly spreading redness
-
You experience chest pain, severe abdominal pain, or other acute symptoms
Your GP will conduct a thorough clinical assessment, including taking a detailed history and performing a physical examination. They may arrange blood tests, imaging studies, or referral to a specialist if indicated. It is helpful to inform your doctor of all medications you are taking, including Ozempic, as this provides important context for your overall health picture.
Alternative Causes of Lymph Node Swelling While Taking Ozempic
Lymph nodes are small, bean-shaped structures that form part of the immune system, filtering lymphatic fluid and helping to fight infections. They can become swollen for many reasons, most of which are unrelated to diabetes medications like Ozempic.
Common infectious causes include:
-
Upper respiratory tract infections – colds, flu, and throat infections frequently cause cervical (neck) lymph node swelling
-
Dental infections or gum disease – can lead to swelling of nodes under the jaw or in the neck
-
Skin infections – cellulitis or infected wounds may cause regional lymph node enlargement
-
Viral infections – including Epstein-Barr virus (glandular fever), cytomegalovirus, or HIV
-
Bacterial infections – such as streptococcal or staphylococcal infections
Non-infectious causes that may coincide with Ozempic treatment include:
-
Autoimmune conditions – such as rheumatoid arthritis or lupus, which can occur alongside type 2 diabetes
-
Medications – certain drugs can cause lymphadenopathy as a side effect, though this is not listed for Ozempic
-
Allergic reactions – to foods, environmental allergens, or other substances
-
Lymphoma or other malignancies – whilst less common, these require exclusion, particularly with persistent or progressive lymphadenopathy
It's important to note that thyroid enlargement (goitre) can sometimes be mistaken for lymph node swelling in the neck, but these are distinct conditions requiring different assessments.
Investigation and management will depend on the clinical presentation. Your GP may arrange:
-
Blood tests – including full blood count, inflammatory markers (CRP, ESR), and specific infection screens
-
Ultrasound imaging – to characterise the lymph nodes and surrounding structures
-
Fine needle aspiration or biopsy – if there is concern about the nature of the swelling (excisional biopsy may be preferred if lymphoma is suspected)
-
Referral to specialist services – such as haematology, infectious diseases, or ear, nose, and throat (ENT) specialists
NICE guidance emphasises the importance of thorough assessment of unexplained lymphadenopathy, with urgent referral (within two weeks) if features suggestive of malignancy are present. The appropriate investigation will identify the underlying cause, allowing for targeted treatment.
Frequently Asked Questions
Can Ozempic cause swollen lymph nodes?
Swollen lymph nodes are not listed as a recognised side effect of Ozempic in UK regulatory documentation. If you develop lymphadenopathy whilst taking Ozempic, seek medical evaluation to identify the underlying cause.
What are the most common side effects of Ozempic?
The most common side effects of Ozempic are gastrointestinal, including nausea, diarrhoea, vomiting, constipation, and abdominal discomfort. These typically diminish over time as the body adjusts to the medication.
When should I see a doctor about swollen lymph nodes?
Contact your GP if lymph nodes remain swollen for more than 3–6 weeks, are hard or fixed, measure over 1–2 cm, or are accompanied by unexplained weight loss, night sweats, or persistent fever.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript